(1/8) Important study demonstrating “opportunistic airborne” transmission of #SARSCoV2 in just five minutes at a restaurant in South Korea, confirmed by CCTV.
Air conditioning may have enabled infection over a distance of more than 4 metres to occur.
jkms.org/DOIx.php?id=10…
Air conditioning may have enabled infection over a distance of more than 4 metres to occur.
jkms.org/DOIx.php?id=10…

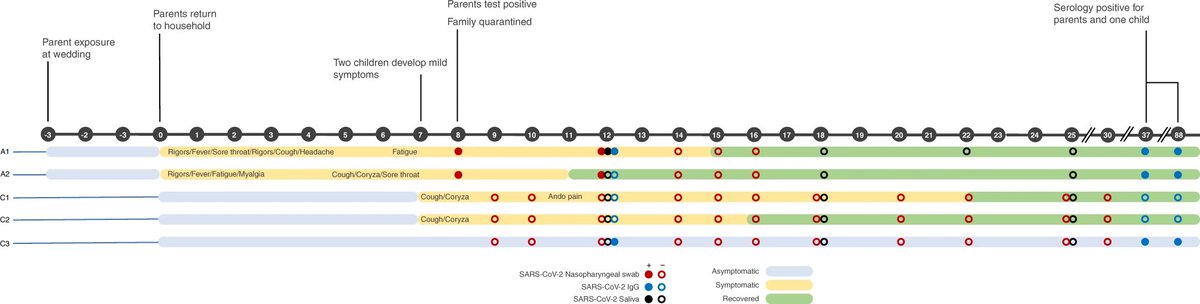
(2/8) In this study, #COVID19 was detected in a person (case A) on 17 June.
The investigators discovered case A had visited the same restaurant as a previous confirmed case (case B) on 12 June.
It was determined case B had probably infected case A.
The investigators discovered case A had visited the same restaurant as a previous confirmed case (case B) on 12 June.
It was determined case B had probably infected case A.

(3/8) All the people who came into contact with case B at the restaurant were then tested.
One more case (case C) was detected among these people.
In total, 2 of the 13 people (15%) who had been in the restaurant at the same time as case B were infected.
One more case (case C) was detected among these people.
In total, 2 of the 13 people (15%) who had been in the restaurant at the same time as case B were infected.
(4/8) The restaurant was 9 x 10 m in size, & had no windows. Two air conditioning units were mounted on the ceiling.
Case A entered at 15:57, and finished their meal before case B entered at 17:15. Case B sat 6.5 m away.
Cases A and B talked with their companions without masks.
Case A entered at 15:57, and finished their meal before case B entered at 17:15. Case B sat 6.5 m away.
Cases A and B talked with their companions without masks.

(5/8) At 17:20, case A left the restaurant.
Two minutes later at 17:22, case C entered the restaurant and sat 5 m away from case B.
21 minutes later, case B left the restaurant.
Two minutes later at 17:22, case C entered the restaurant and sat 5 m away from case B.
21 minutes later, case B left the restaurant.
(6/8) Environmental samples were taken, of which all 39 tested negative.
Air conditioning may have helped respiratory droplets and/or aerosols travel over a distance of 4.8 metres and greater from case B to cases A and C.
Case A had only 5 minutes exposure.
Air conditioning may have helped respiratory droplets and/or aerosols travel over a distance of 4.8 metres and greater from case B to cases A and C.
Case A had only 5 minutes exposure.
(7/8) The authors conclude that transmission over distances greater than 2 metres is possible, and that contact tracing definitions should be updated to reflect this.
(8/8) The authors also write that tables in indoor restaurants should be separated by more than 2 metres.
Masks should only be removed while eating, and conversations during meals should be avoided.
Masks should only be removed while eating, and conversations during meals should be avoided.
• • •
Missing some Tweet in this thread? You can try to
force a refresh