Study showing that children can be infected with #SARSCoV2, but still test negative.
Two parents infected their 3 children, who tested negative 11 times (NP swab PCR test). Antibody blood tests were also negative, but saliva antibody tests were positive.
nature.com/articles/s4146…
Two parents infected their 3 children, who tested negative 11 times (NP swab PCR test). Antibody blood tests were also negative, but saliva antibody tests were positive.
nature.com/articles/s4146…
In this study, 2 parents from Melbourne attended an interstate wedding without their children, during which they were infected. They returned home and developed symptoms 3 days later. 
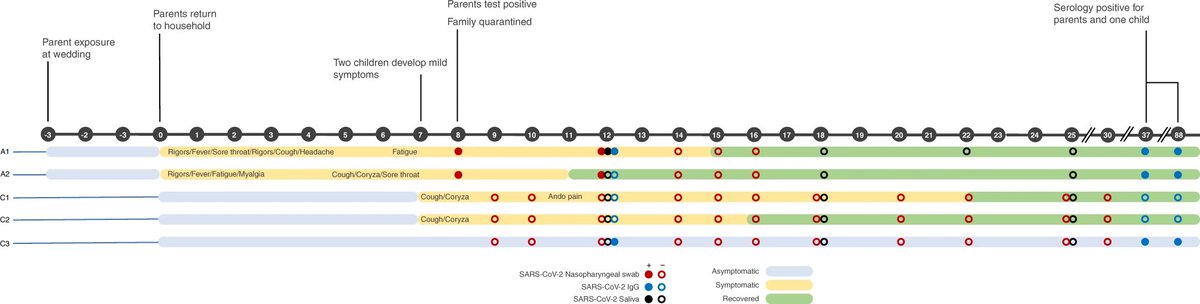
Seven days after this, 2 of their 3 children developed symptoms.
The oldest child (male, 9 years) developed respiratory and gastrointestinal symptoms.
The oldest child (male, 9 years) developed respiratory and gastrointestinal symptoms.
The second child (male, 7 years) developed respiratory symptoms.
The third child (female, 5 years) remained asymptomatic.
The third child (female, 5 years) remained asymptomatic.
Eight days after the parents had developed symptoms, they were traced as contacts and tested for #SARSCoV2.
The parents tested positive, but all children repeatedly tested negative (11 times by nasopharyngeal swab PCR test).
The parents tested positive, but all children repeatedly tested negative (11 times by nasopharyngeal swab PCR test).
Blood, saliva, and faecal samples were collected every 2-3 days from the family, along with nasopharyngeal swab samples.
All saliva, faecal, and swab samples from the children were negative for #SARSCoV2 by PCR, although all children tested positive for rhinovirus (the common cold) on day 10.
Blood samples were used to measure the cellular immune response of family members on days 12, 37, and 88.
The profile in all family members was consistent with #SARSCoV2 infection.
The profile in all family members was consistent with #SARSCoV2 infection.
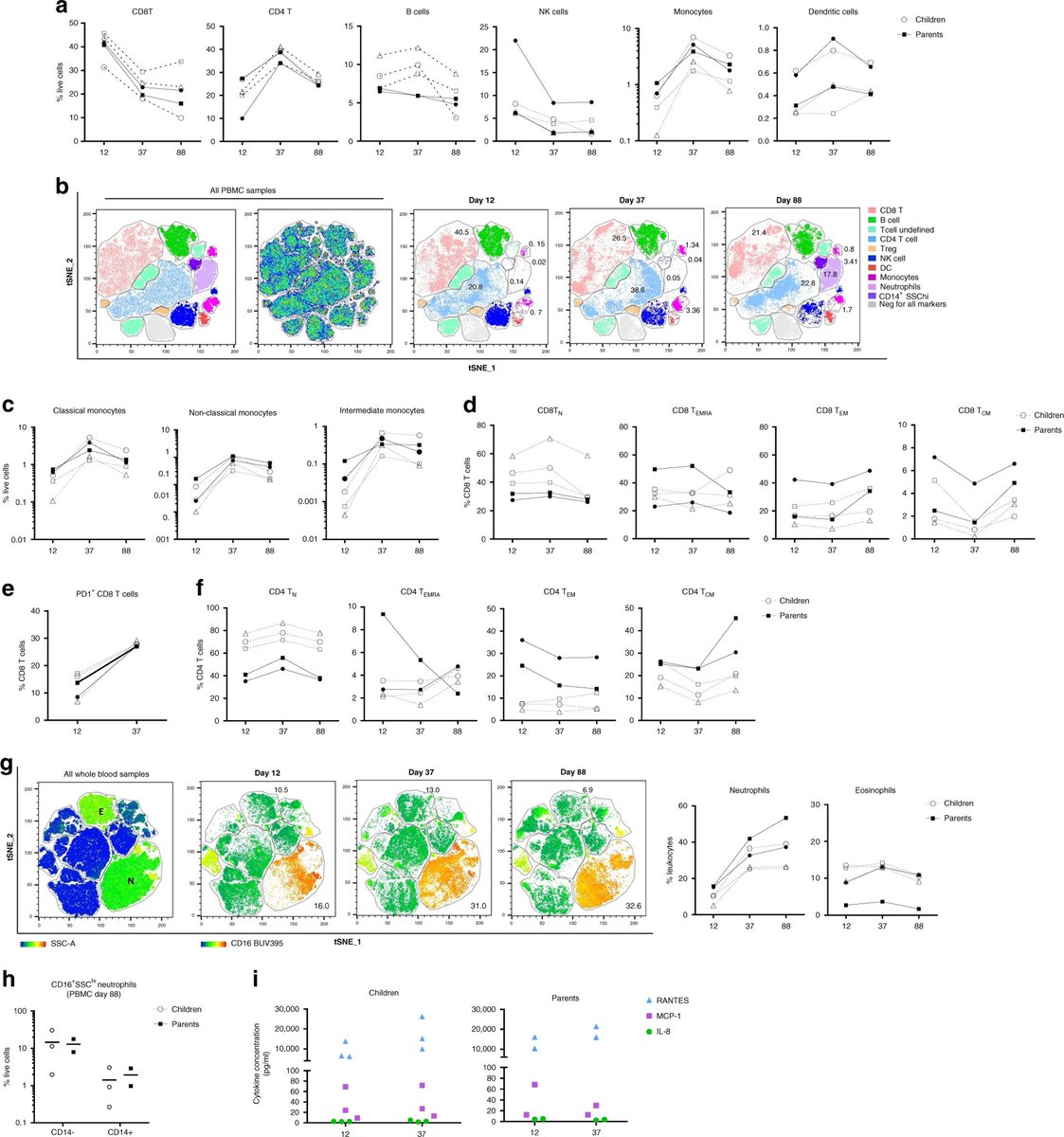
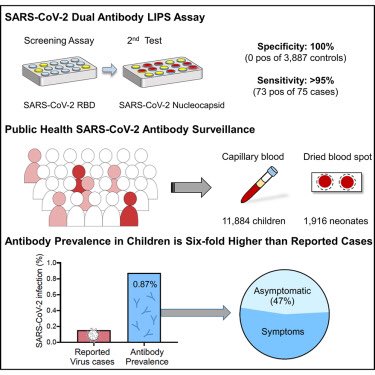
Saliva from all family members tested positive for IgA antibodies against the #SARSCoV2 spike protein at all time points. IgG and IgM antibodies were more variable.
IgG antibodies were readily detected in blood in both parents, while only the asymptomatic child tested positive.
Only one parent had a robust neutralising antibody response. The second parent and asymptomatic child mounted a limited response.
Only one parent had a robust neutralising antibody response. The second parent and asymptomatic child mounted a limited response.
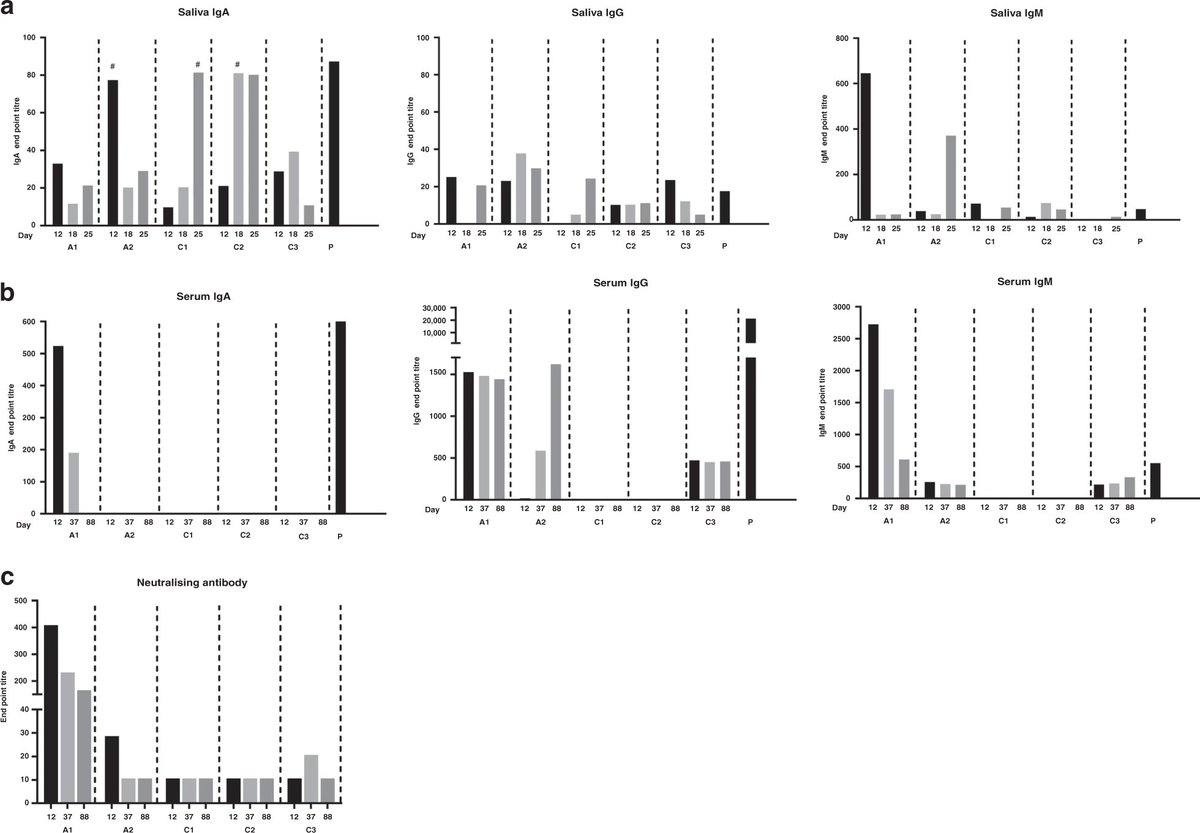
Interestingly, among the children, the strongest antibody response was produced by the asymptomatic child.
The children were tested on multiple occasions while 2 out of 3 were symptomatic, which makes it unlikely that they cleared the virus before being tested.
Instead, the study suggests the children mounted an immune response which was highly effective in limiting replication of the virus.
However, it is unclear if this family will be protected from reinfection, because only one parent had a robust neutralising antibody response.
In conclusion, this study shows that children can be infected with #SARSCoV2, but may not test positive using either a nasopharyngeal swab PCR test, or an antibody blood test.
A saliva IgA antibody test might be a useful adjunct for detecting cases in children.
A saliva IgA antibody test might be a useful adjunct for detecting cases in children.
Addendum: I’d like to reiterate a key point.
Neither nasopharyngeal swab PCR tests nor saliva PCR tests were able to detect these cases. Only saliva antibody testing could.
So, regular saliva tests will still miss these cases. The adjunct test must be a saliva antibody test.
Neither nasopharyngeal swab PCR tests nor saliva PCR tests were able to detect these cases. Only saliva antibody testing could.
So, regular saliva tests will still miss these cases. The adjunct test must be a saliva antibody test.
• • •
Missing some Tweet in this thread? You can try to
force a refresh