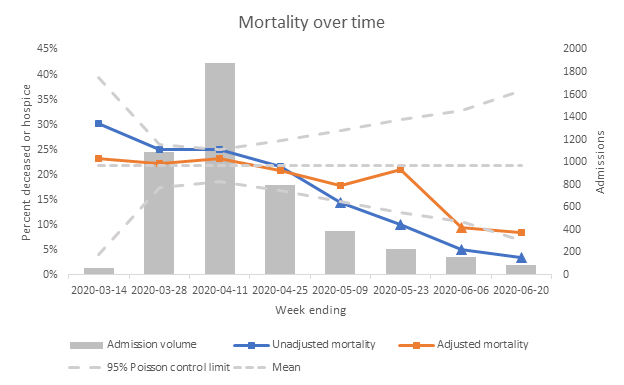
Our new paper in @JAMANetworkOpen shows no disparity in adjusted outcomes between Black/Hispanic/White #COVID19 patients @nyulangone once hospitalized; if anything, Blacks seem to do a little better. Is this an anomaly? @gbengaogedegbe ja.ma/3n1NKhC /Thread 

Actually, several other papers have now found the same. This study of 11,210 hospitalized patients at 92 @ascensionorg hospitals found no sig difference in mortality between Blacks & Whites @BYehia jamanetwork.com/journals/jaman…
This @cdcgov study of 2,491 hospitalized patients at 154 hospitals across the US confirms the findings academic.oup.com/cid/advance-ar…
Not to mention this study of 1,382 hospitalized patients @OchsnerHealth and several other single site studies @Dr_E_PH nejm.org/doi/full/10.10…
Yet, it is indisputable that Black, Hispanic and Indigenous communities have 2-4 times greater age-adjusted #COVID19 mortality rates than Whites @apmresearch
apmresearchlab.org/covid/deaths-b…
apmresearchlab.org/covid/deaths-b…

So, why is that? Recall disparities can arise at any point in causal pathway. In this case, several other steps in the pathway are the likely culprits:
Higher risk of getting infected (more front-line jobs/less ability to work from home, more crowded living conditions); e.g. high risk Blacks & Hispanics more likely to live with someone in a high risk job pubmed.ncbi.nlm.nih.gov/32663045/
Living in worse environmental conditions, potentially increasing mortality risk @DrTMersha pubmed.ncbi.nlm.nih.gov/32389591/
More difficulty accessing (timely) care. Testing, e.g., less available in minority communities. Plus Blacks are 1.5 times more likely to be uninsured than Whites; Hispanics >2.5x. kff.org/racial-equity-…
Possibly, more likely to be cared for in lower quality/less well-resourced hospitals. I haven’t seen data on #COVID19 mortality differences by hospital in US, but in other conditions, minority-serving hospitals often do worse on quality measures, e.g. pubmed.ncbi.nlm.nih.gov/31400737/
So, what our study and those of others show is that the degree of within-hospital bias seems to be relatively minimal; not enough to affect outcomes. That’s some good news, but more importantly, should help prioritize the many other areas we need to focus on to improve outcomes.
• • •
Missing some Tweet in this thread? You can try to
force a refresh