As you turned the corner on the second flight of stairs, you felt your breath pull a little deeper, the next one come a little earlier. Your heart said 👋🏼, bounding softly in your neck.
Ten seconds down the hall, all that faded. You were back to mulling some thought.
1/
Ten seconds down the hall, all that faded. You were back to mulling some thought.
1/
But hold on. Let’s pause for a minute and retrace the steps.
A lot happened before the extra breath and the tug in your neck caught your attention.
And it’s all so damn cool.
2/
A lot happened before the extra breath and the tug in your neck caught your attention.
And it’s all so damn cool.
2/
At the foot of the stairs, anticipation of exertion 🔔 and the stretch of muscle fibers 🦵🏽sent a signal to the sympathetic nervous system: start the car.
3/
3/
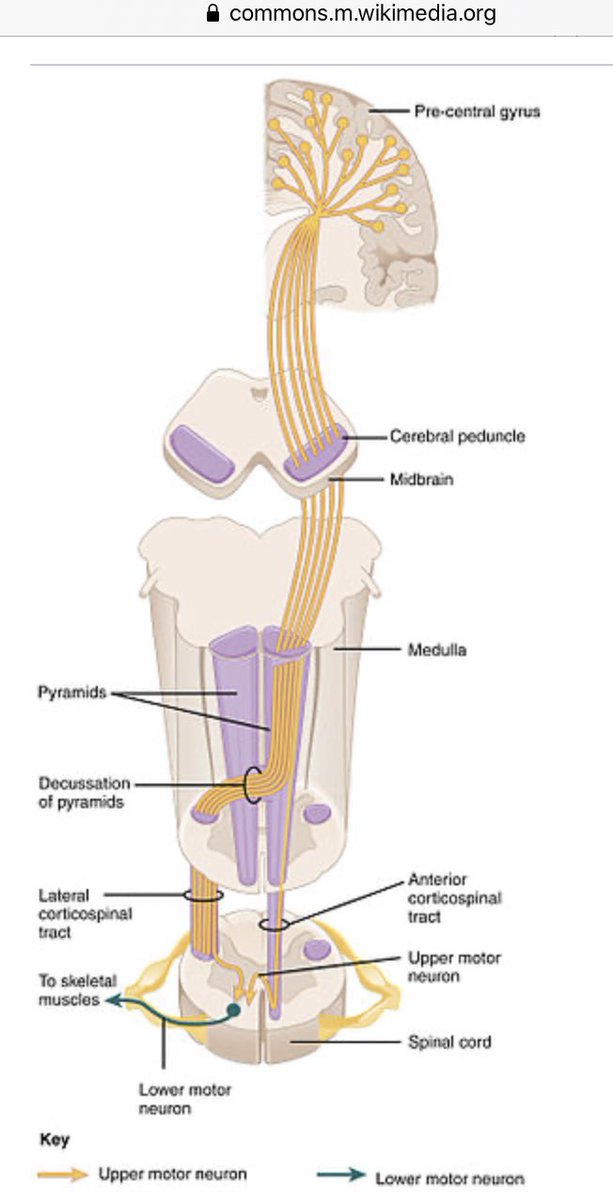
Then your brain made your legs move.
Basal ganglia 👋🏼. Pre-frontal motor cortex⚡️thru internal capsule, brainstem 🔀, corticospinal tract.
Alpha-motor neuron⚡️thru spinal root and nerve to neuromuscular junction.
Acetylcholine+🥩=⚡️
Actin + myosin shorten. ATP releases.
3/
Basal ganglia 👋🏼. Pre-frontal motor cortex⚡️thru internal capsule, brainstem 🔀, corticospinal tract.
Alpha-motor neuron⚡️thru spinal root and nerve to neuromuscular junction.
Acetylcholine+🥩=⚡️
Actin + myosin shorten. ATP releases.
3/
Your big muscles doing work led to two things.
First, locally released vasodilatory substances made a new path of least resistance for your cardiac output. More blood flowed there, less everywhere else.
..but only for a second.
4/
First, locally released vasodilatory substances made a new path of least resistance for your cardiac output. More blood flowed there, less everywhere else.
..but only for a second.
4/
The pressure receptors in your aorta and carotids felt the drop. Less ⚡️up the vagal and glossopharyngeal nerves disinhibited sympathetic outflow from the brainstem.
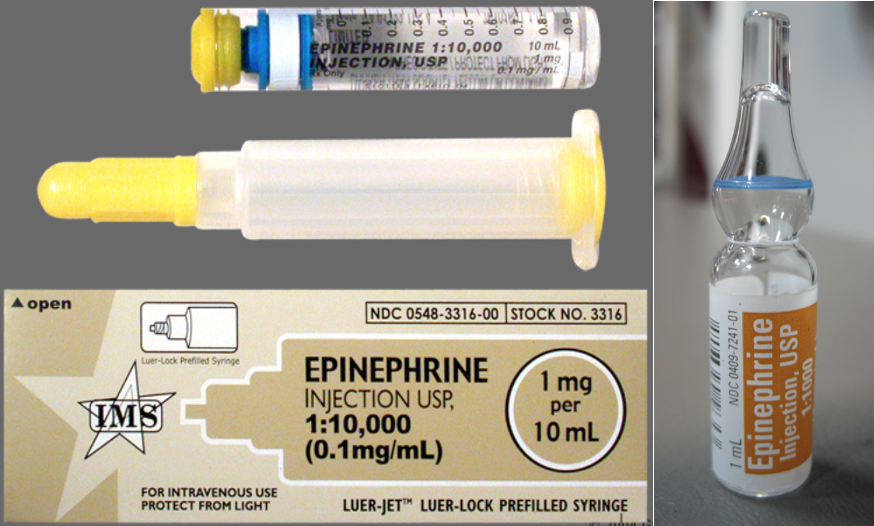
Foot on the gas. The spike in norepinephrine made your heart squeeze harder and faster.
5/
Foot on the gas. The spike in norepinephrine made your heart squeeze harder and faster.
5/
Your cardiac output doubled, to make sure to still send the usual 5 L/min to the brain and kidneys and such on top of the extra 5 L/min your legs were suddenly siphoning.
Then when your legs stopped siphoning, you felt some extra pep go up your carotids.
6/
Then when your legs stopped siphoning, you felt some extra pep go up your carotids.
6/
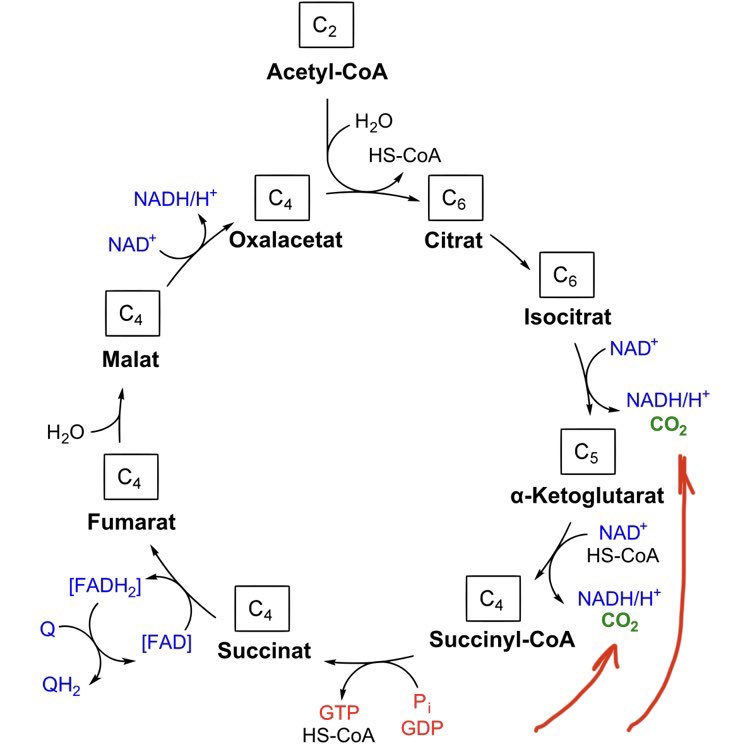
And all of this was to bring extra O2 and fuel to the muscles (without making you faint). But what happened to those?
O2 + glucose ➡️ CO2 + H2O.
A little electron transporting here, a little Kreb’s cycling there made this happen.
7/
O2 + glucose ➡️ CO2 + H2O.
A little electron transporting here, a little Kreb’s cycling there made this happen.
7/
And the Kreb’s cycle has a little byproduct that the body likes to keep in a very exact range: CO2.
8/
8/
As the extra CO2 coursed through your🩸, peripheral receptors told your medulla that your pCO2 was now 42 and not 40. Two sec later, 44. Uh-oh.
Chemoreceptors in medulla itself sensed a pH of 7.33. Some of that was from the CO2... some from a little lactate in the mix.
9/
Chemoreceptors in medulla itself sensed a pH of 7.33. Some of that was from the CO2... some from a little lactate in the mix.
9/
Nearby, the pontine respiratory groups got the message, and signaled your diaphragm and company to breathe deeper and faster. To blow off more CO2 and bring it (and the 🩸 pH) back to set point.
10/
10/
One of the things that can make us feel aware of our breathing (or feel short of breath) is a mismatch between ventilatory demand and ventilatory reality. In this case, it was mild and transient, as your compensation caught up and the exertion soon ended.
11/
11/
There’s a lot of other things that happened and changed on those stairs and in the hallway after (... and every second since).
Being aware of even a small fraction of it can bring wonder and aesthetic joy.
12/fin
Being aware of even a small fraction of it can bring wonder and aesthetic joy.
12/fin
• • •
Missing some Tweet in this thread? You can try to
force a refresh