1/ Covid (@UCSF) Chronicles, Day 276
Here’s my summary of yesterday’s fascinating grand rounds (sorry it's a day late), here: Far-ranging discussion re: the problems at the CDC, vaccine roll-out @ucsf, and the complex matter of immunity passports.
Here’s my summary of yesterday’s fascinating grand rounds (sorry it's a day late), here: Far-ranging discussion re: the problems at the CDC, vaccine roll-out @ucsf, and the complex matter of immunity passports.
2/ Session began with a fireside chat w/ Julie Gerberding, a @UCSF adjunct faculty member who ran @CDCgov from 2002-2009, and led @Merck's vaccine development program afterwards. I asked Julie about how the CDC prepared for a pandemic during her tenure as director. 

3/ “SARS was a wakeup call,” she said, particularly after post-9/11 anthrax attacks. “After that, we got very serious about influenza… it led to a major investment in pandemic preparedness,” including full scale table-top pandemic preparedness exercises with every state.
4/ Were they ready for Covid-like threat? Partly. But, in retrospect she says, in preparing for flu testing isn’t that critical – patients have classic symptoms. But Covid’s superpower of asymptomatic disease & transmission left CDC unprepared for a huge diagnostic testing need.
5/ Second, while they appreciated need for social distancing, schools closures, shelter-in-place, they didn’t engage enough w/ legislative & appropriations process to sufficiently “prepare for how they would offset the economic consequences of the public health interventions.”
6/ That said, they were generally ready for the tension between public health & economy, & the U.S.'s libertarian streak. “We did [expect that these would be issues]… History repeats itself. The 1918 experience is very similar to… now in terms of pushback, regional variations.”
7/ Unfortunately, all the CDC's prep work eroded. “It’s crisis-to-complacency,” she said sadly. Over time, without a major pandemic threat, “all of that focus and energy got displaced into other priorities; that’s the tragedy of our long-term preparedness planning in America.”
8/ Keys to communication in a pandemic: “Tell people what you know, & also what you don’t know… & what you’ll do to get answers.” They don’t expect you to have all the answers, but they expect you to tell the truth. That’s how you gain people’s trust.” Didn’t happen with Covid.
9/ CDC has improved recently, but communication is still flawed: “It's way too oriented toward #'s, statistics, factual information. That’s not really what people want to hear.” People do want fast, accurate info..."But mostly they want to know you care. We are so missing that…
10/ …piece of the conversation….[They need to know that Covid] is touching people’s hearts, hurting their families, that it's sad, it’s frightening… Too much of the time they’re taking a very left brain approach, and it moves people away from trust.”
Turning to vaccines...
Turning to vaccines...
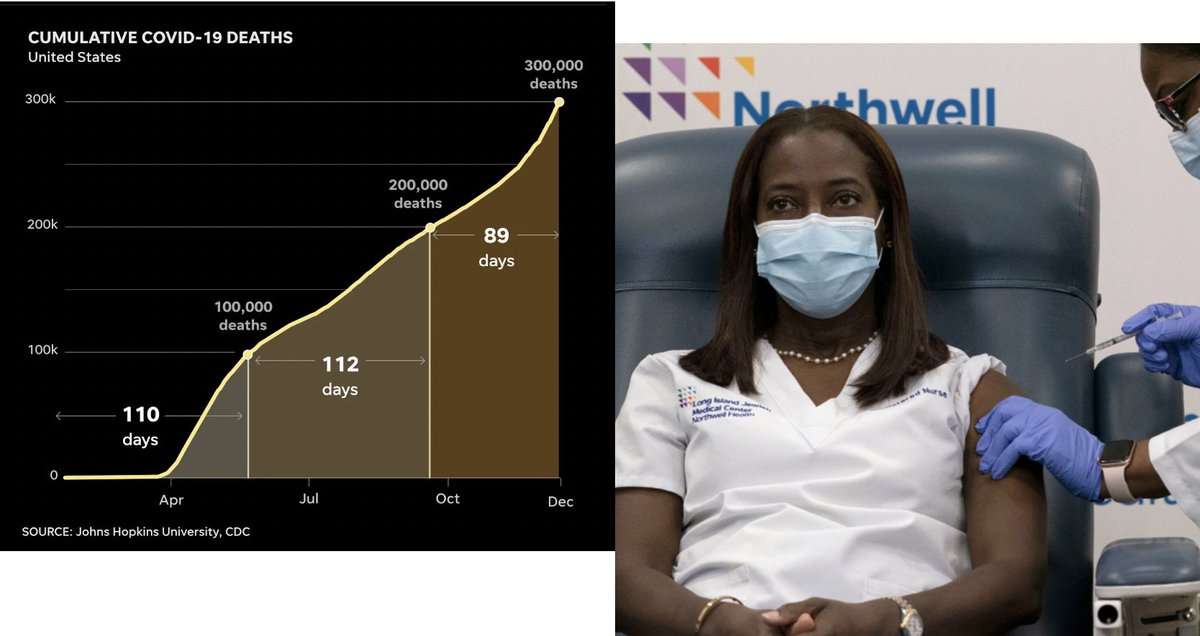
11/ ...I asked Julie when she anticipated a vaccine when she learned of Covid in Jan. “I didn’t think it would be this year….It's a very high risk business, it’s really hard to get everything right." "What I first worried about in January was that Covid would have a mortality…
12/ ...rate of 10% (like SARS) or 50% (like MERS). It could be so much worse.” But she was confident that SARS-CoV2 is “a vaccinable pathogen.” Some of its characteristics make it a relatively easy target: large virus, little genetic drift, & spike protein is a “great immunogen.”
13/ On safety: We have “great efficacy & safety profile after two months in ~50K pts. I acknowledge that we may have unpleasant surprises, but everything is signaling that these are really good & effective vaccines.” Says she would take vaccine now if she were a frontline worker.
14/ Five hurdles to overcome: efficacy (great), safety (good so far), durability (don’t know yet), what will the virus do (will it drift?). Last is uptake/access/distribution: “hardest one…it’s the sociologic factors, globalism vs. nationalism… we really need to restore trust.”
15/ Next was an update on UCSF’s vaccine distribution, starting w/ vaccinating our healthcare workers. Such programs have become controversial – it’s a tricky thing to get right. @UCSF's plan, which prioritized our front-line providers into 4 groups, and randomized within…
16/ …each group, is generally going smoothly. It’s made easier by fact that our supply is better than we thought (~4000 doses now, w/ potential for another ~8000 coming next week). That should allow us to get through most of our front-line clinicians & other essential staff…
17/ … in the next few wks. Fig (from town hall today) shows status as of 12/18; >500 vaccinations/day, new email invites going out nightly. Sound decision by @UCSF to include students, residents, custodial staff, interpreters, transporters, etc – not every hospital did. And… 

18/…the randomization seems fair & also ensures we don’t vaccinate everybody in a given area (wards, ED, ICU) on the same day. (Parenthetically, I received my shot 11 hours ago and I still feel just fine.) Picture is of Susan Smith and Desi Kotis describing the complex process. 

19/ Final topic: Immunity Passports (aka “Immunity Certification”), by David Studdert of @Stanford. To me, one of the most interesting – & sure-to-be controversial – questions for next few mths. It came up early in pandemic, but receded since nobody knew how well immunity worked.
20/ But the question is roaring back with the availability of highly effective vaccines. Now, says Studdert, “immunity certification programs seem inevitable.” In fact, “from a policy standpoint, we might want such programs as a way of incentivizing…vaccination.” 

21/ From unpublished study by Studdert, public views on Immunity Passports are split; 55% oppose, 45% support. Most remarkably, this may be the one issue in Covid that does not split along usual lines, including by risk status, race/ethnicity, or even political affiliation. 

22/ I asked what'll happen when bipartisanship dissolves, as it will. Nuanced: “On one hand, conservatives are interested in getting business up & running… but anything that’s govt or centrally controlled won’t be attractive. Liberals will be suspect of it from the get-go, but…
23/ …it may “have a leveling effect – rewarding bus drivers for [being] on front lines, getting vaccinated & resuming valuable work – that could be appealing to liberals.” Since poor/minorities have high rates of Covid, “it could…act as a class leveler, not a class divider.”
24/ I pushed DS re: whether he thinks Passports are good idea. “It’s a necessary idea…I can’t see how we can hold back on some selective privileging to get the economy moving & people back to work. But we have to be really careful…history is strewn with bad programs like this.” 

25/ I hope you’ll watch this great discussion, again here: tinyurl.com/y75bq29s
This was last Grand Rds of 2020. Thanks to fab production team & extraordinary speakers, who have taught me (& ~1.5M viewers) so much about this infinitely sad yet fascinating topic. Stay safe.
This was last Grand Rds of 2020. Thanks to fab production team & extraordinary speakers, who have taught me (& ~1.5M viewers) so much about this infinitely sad yet fascinating topic. Stay safe.
• • •
Missing some Tweet in this thread? You can try to
force a refresh