Am concerned that implicit use of uninformed priors has severely limited pandemic responses:
(i) Inaction is favored over action.
(ii) Information void is soon filled by misinformation.
From masks to immunity to vaccines; let's not keep making the same class of mistake. 🧵
(i) Inaction is favored over action.
(ii) Information void is soon filled by misinformation.
From masks to immunity to vaccines; let's not keep making the same class of mistake. 🧵
Ex 1: No evidence of being airborne, despite this being a respiratory illness.
Just because airborne spread wasn't fully vetted does not mean it wasn't likely. Mask use delays are a consequence of remaining 'uninformed' about routes despite many examples (choir/etc.).
Just because airborne spread wasn't fully vetted does not mean it wasn't likely. Mask use delays are a consequence of remaining 'uninformed' about routes despite many examples (choir/etc.).
Ex 2: No evidence of protection from reinfection, despite the nearly universal absence of reinfections.
Without looking to SARS-1/MERS, then proactive steps to leverage and expand sero testing and interventions were missed (including surveys for missed infections).
Without looking to SARS-1/MERS, then proactive steps to leverage and expand sero testing and interventions were missed (including surveys for missed infections).
Ex 3: No evidence of protection from transmission w/vaccines, only reduction of severe illness.
Thankfully, it seems shift is happening, but messaging must balance the impacts on hesitancy if the message remains that there is no evidence of reduction in infection/transmission.
Thankfully, it seems shift is happening, but messaging must balance the impacts on hesitancy if the message remains that there is no evidence of reduction in infection/transmission.
Ex 4: No evidence asymptomatic transmission is major route.
The use of symptom based checks predominates despite ample evidence of asymptomatic/presymptomatic spread. Recognizing this route shifts messaging to mask wearing + testing (still under-utilized as mitigation).
The use of symptom based checks predominates despite ample evidence of asymptomatic/presymptomatic spread. Recognizing this route shifts messaging to mask wearing + testing (still under-utilized as mitigation).
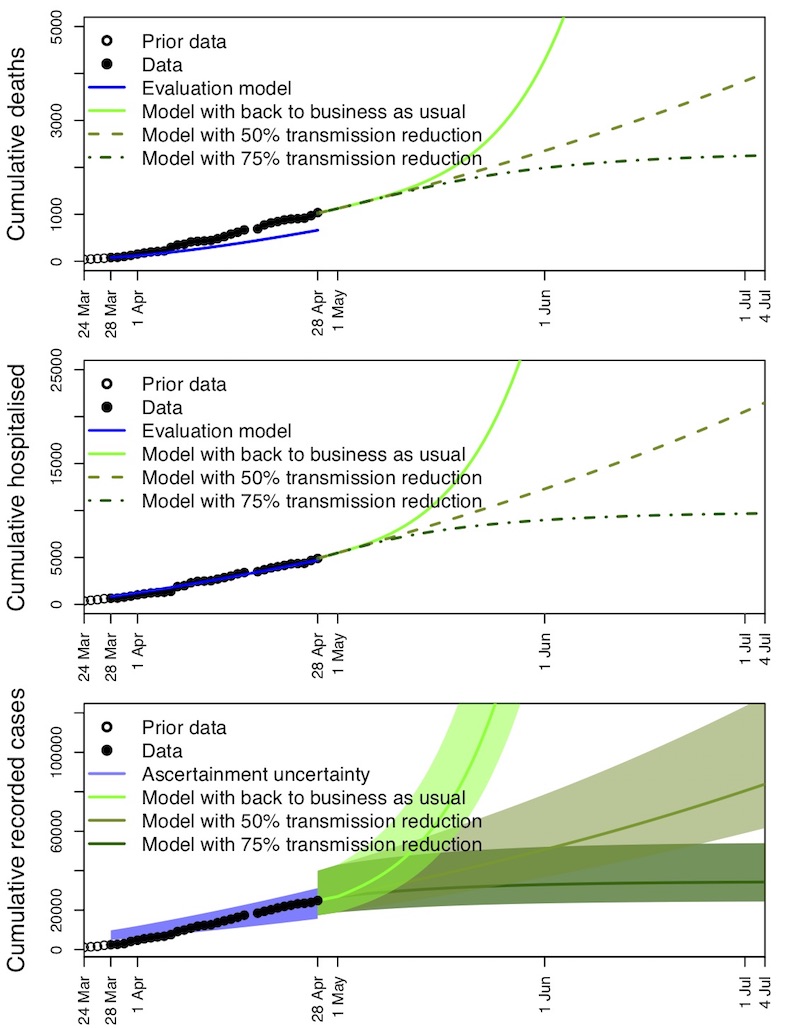
Ex 5: Testing is not proven as a means of mitigation.
Even simple models reveal how this could work; and those few innovators who did so have made a difference. The CDC could have shaped the landscape by value-ing testing as mitigation given early successes.
Even simple models reveal how this could work; and those few innovators who did so have made a difference. The CDC could have shaped the landscape by value-ing testing as mitigation given early successes.
In total, the burden of proof is higher if one starts off with completely uninformed priors, so much so that it can paralyze action and public understanding. Yes, one must proceed carefully, but doing so w/completely uninformed priors misrepresents the dynamics at play.
Perhaps this is too meta, but don't think so.
Am hopeful that the vaccine story can shift quickly from 'no evidence that vaccines reduce transmission' which, if predominates, will almost certainly be proven wrong and almost certainly negatively impact vaccine uptake.
Am hopeful that the vaccine story can shift quickly from 'no evidence that vaccines reduce transmission' which, if predominates, will almost certainly be proven wrong and almost certainly negatively impact vaccine uptake.
• • •
Missing some Tweet in this thread? You can try to
force a refresh