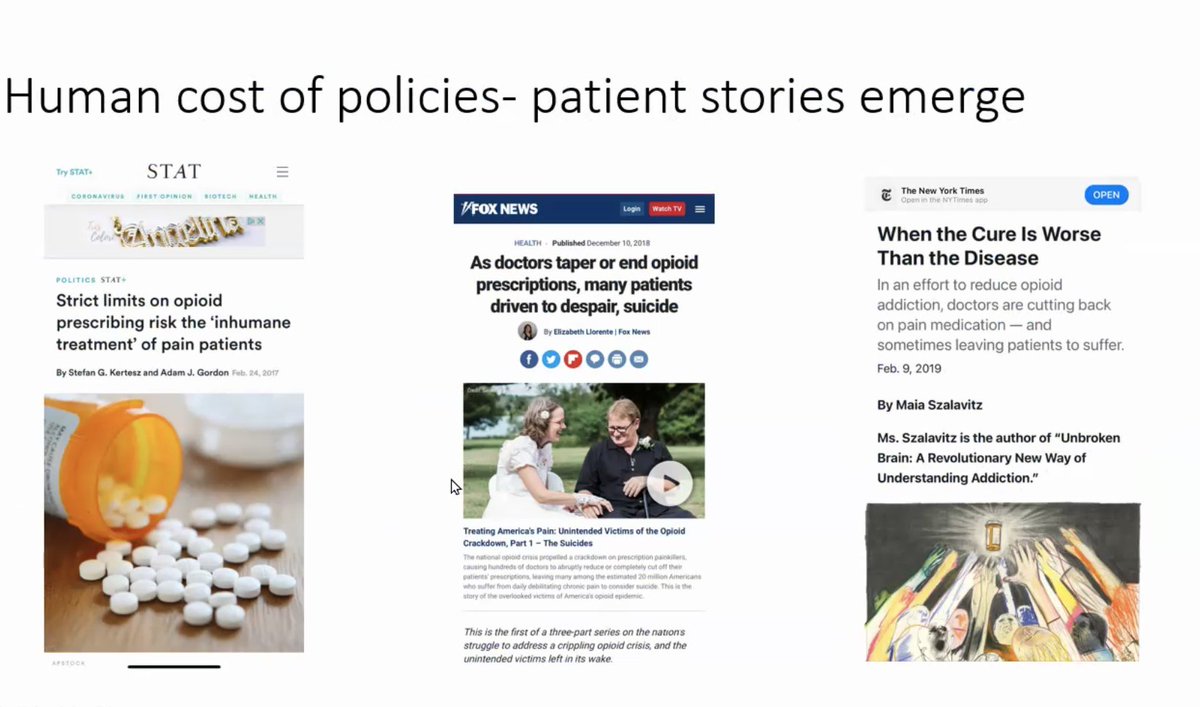
1/I'm excited that Dr. @AjayManhapra is presenting on concerns about mandatory opioid taper for VA's MAT-VA journal club, based on our shared paper... he notes Human costs of mandatory and widespread opioid taper 
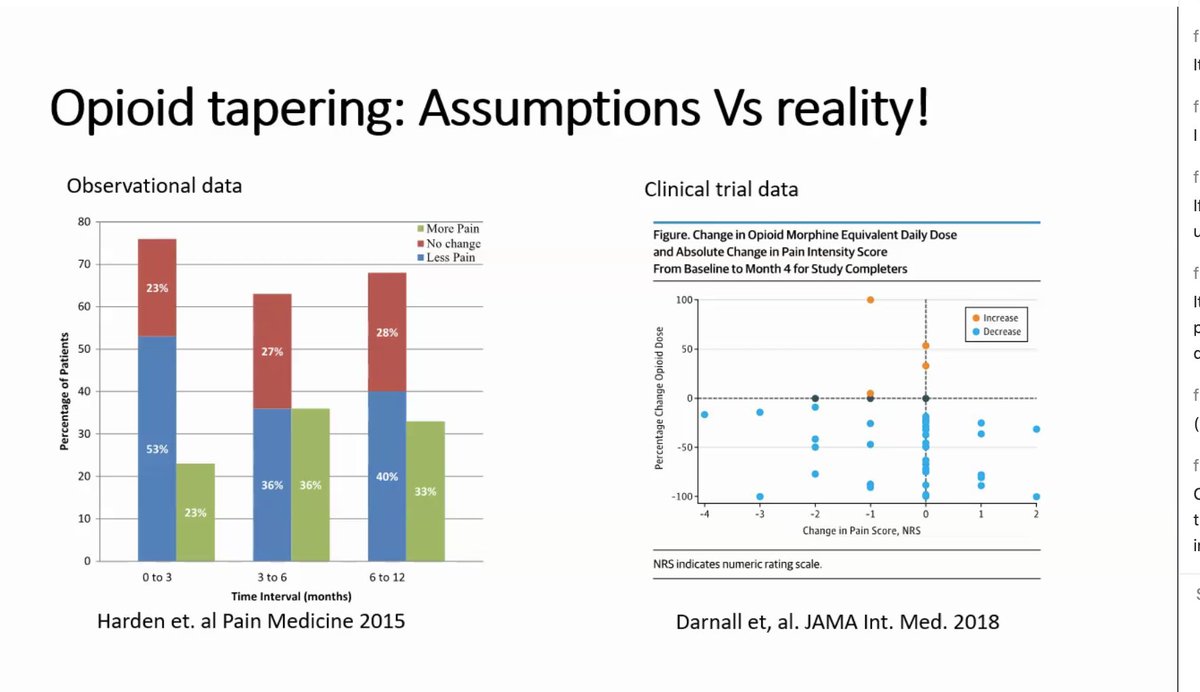
2/He cites @BethDarnall as the best available study, noting that even when one offers the best support system, a significant % of patients do not have a reduction in pain or pain worsens. 
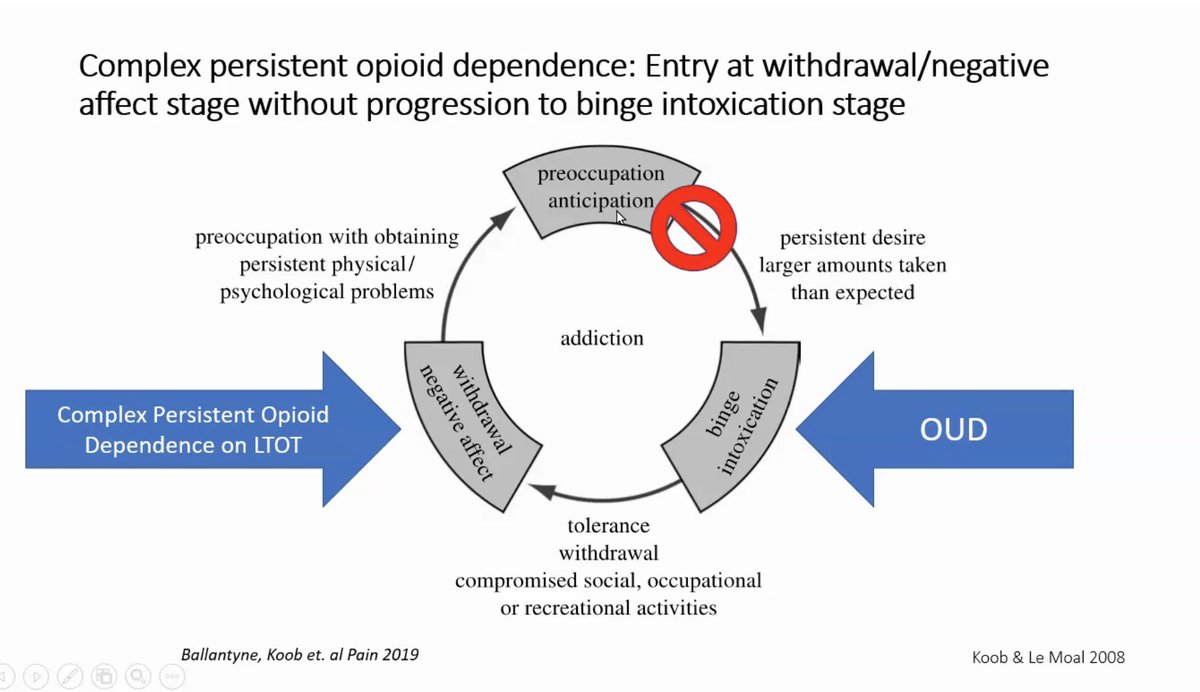
3/In a way that will seem controversial, he proposes that opioid therapy is not exactly an analgesic. This is daily use of an addictive substance that offers relief, where only a minority develop addiction.
4/I should caution that @AjayManhapra is far from a "fan" of opioids for pain. Many people on them do not get benefit, he says. My reading of same data is more favorably disposed, even though we collaborate
5/There is an "opponent effect" so that relief from opioids is also opposed - not in all people and to the same degree - but this is part of the dependence dilemma for some persons at high dose 
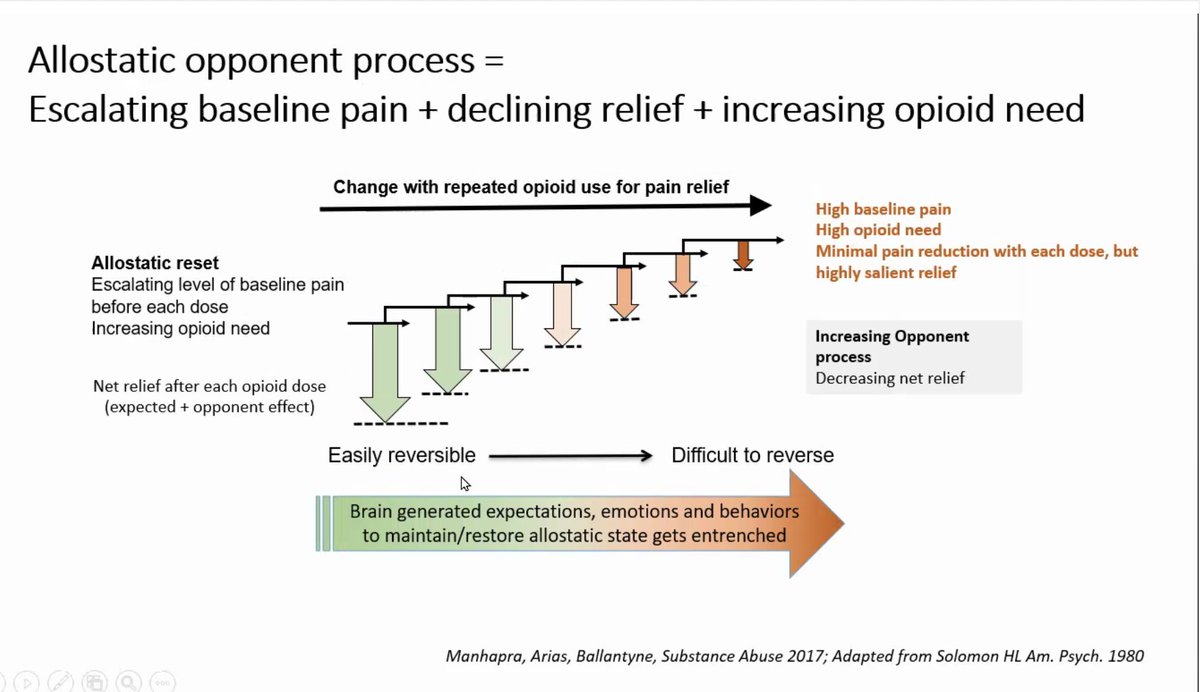
6/Trigger warning: Dr. Manhapra describes a distinct category of Opioid Use Disorder (which most patients do not have at all) from what he and some others call Complex Persistent Opioid Dependence 
6/Opioid tapering is intuitively appealing but the goals of a taper are rarely declared and when they are (see below) they are not regularly achieved 
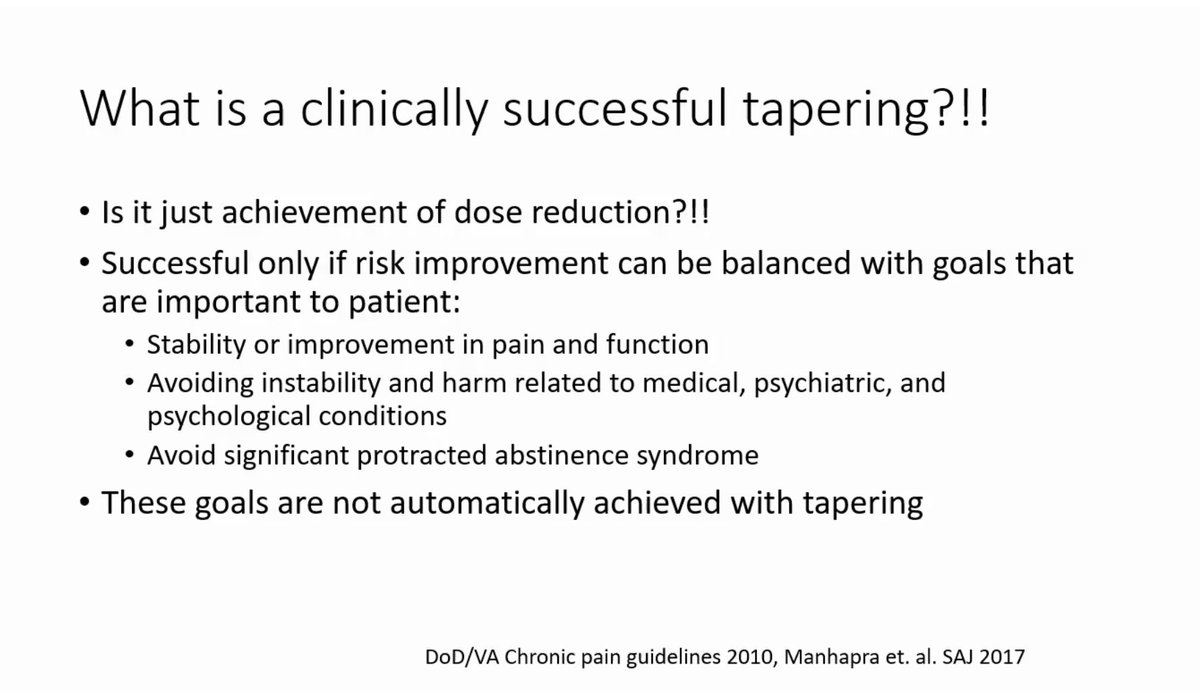
7/The available data on opioid taper suggests (with low confidence) improvement if patients are in "intensive multimodal pain interventions".
And "none of these (tapering) studies showed functional improvement" says @AjayManhapra
And "none of these (tapering) studies showed functional improvement" says @AjayManhapra
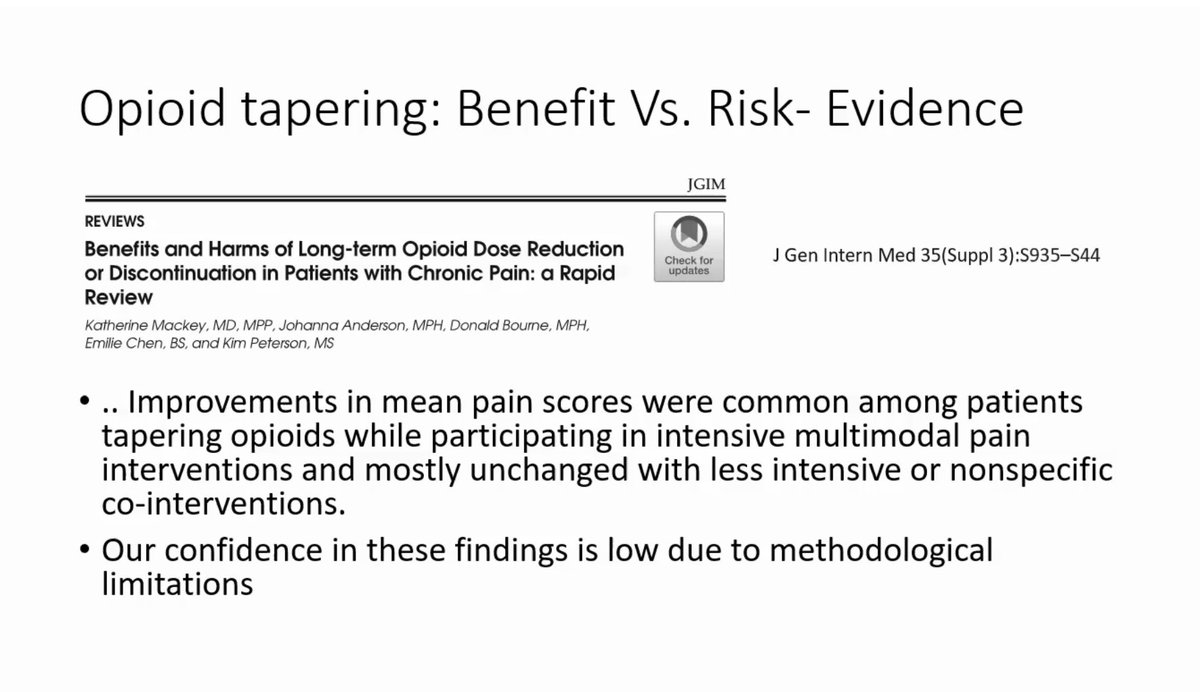
8/As Dr. Manhapra summarizes, regarding opioid taper
"There is no clear benefit but there are reports of harm"
"There is no clear benefit but there are reports of harm"
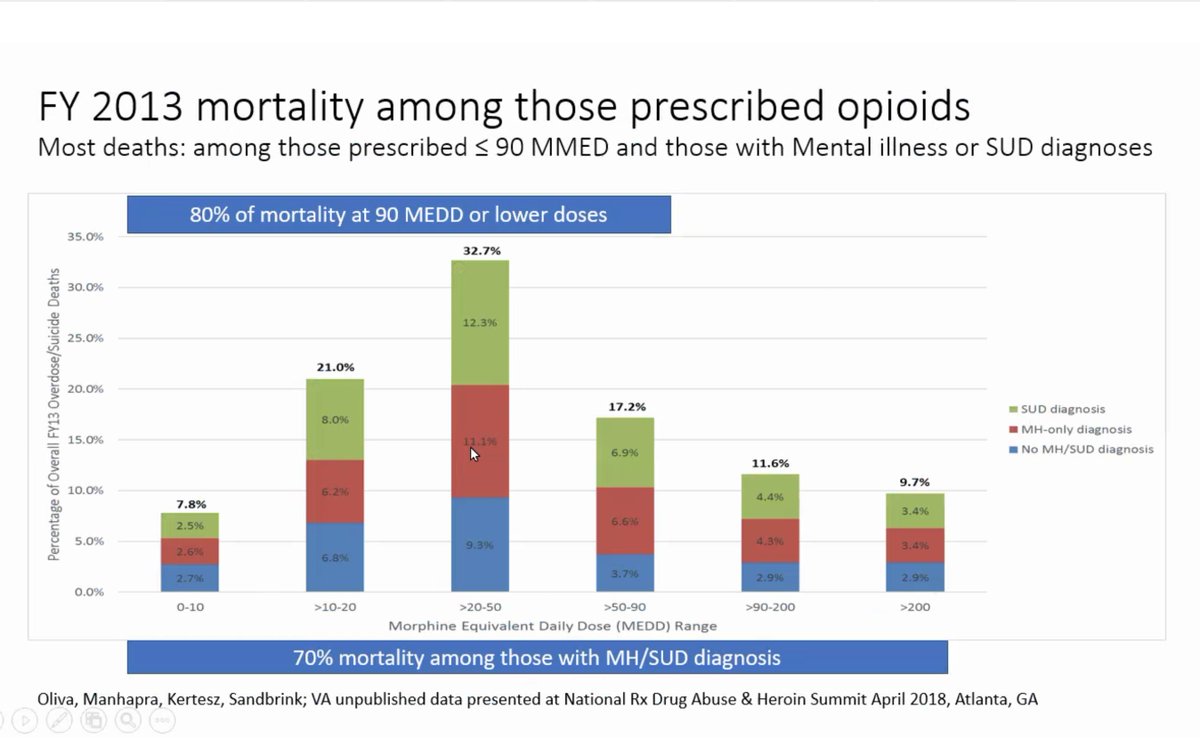
9/Dose and risk of harm are correlated, but it's complicated. "It's not the opioids alone" - the risk is determined by what else is going on in their lives, personal characteristics. Dose is a MINOR factor in the modeled risk in Veterans Administration
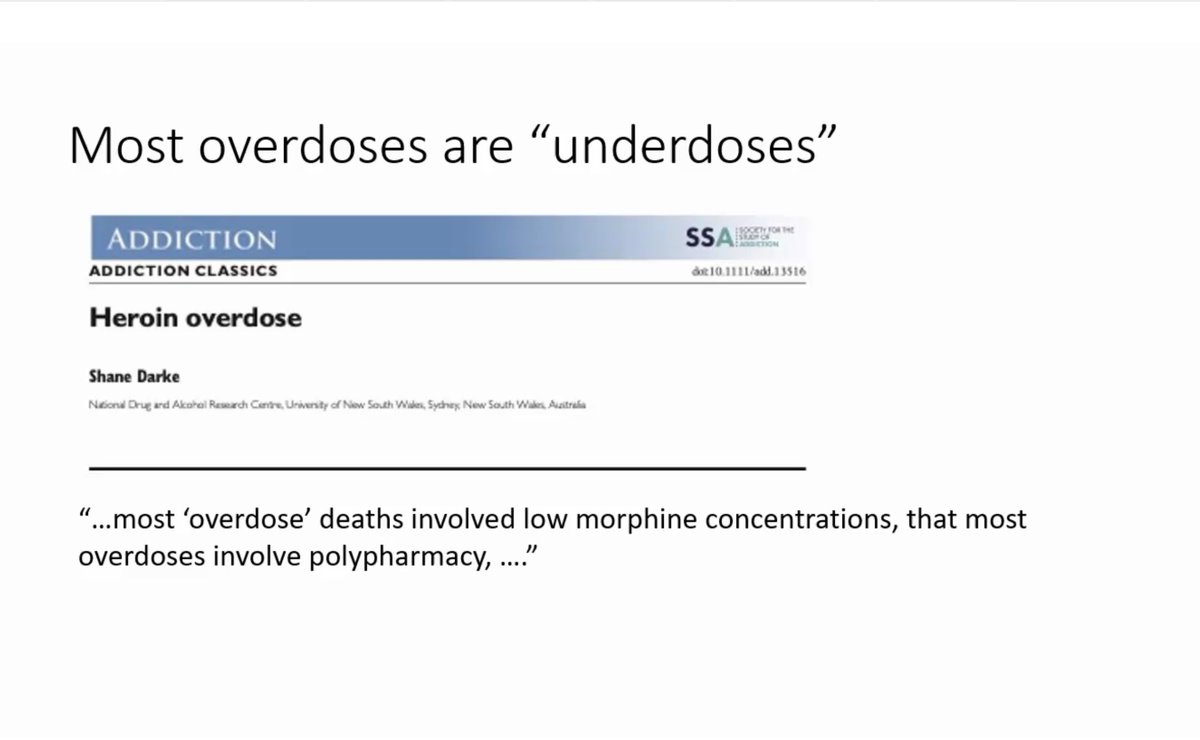
10/Most overdose happens at low dose- so focus on dose is not solid. Veterans Affairs overdose data. 
12/Opioid cessation associated with increased risk of overdose/suicide in Veterans. It's highest in the first month afterward. Then begins to fall. But it never comes down to the level of the persons who were continued on opioids. bmj.com/content/368/bm… 
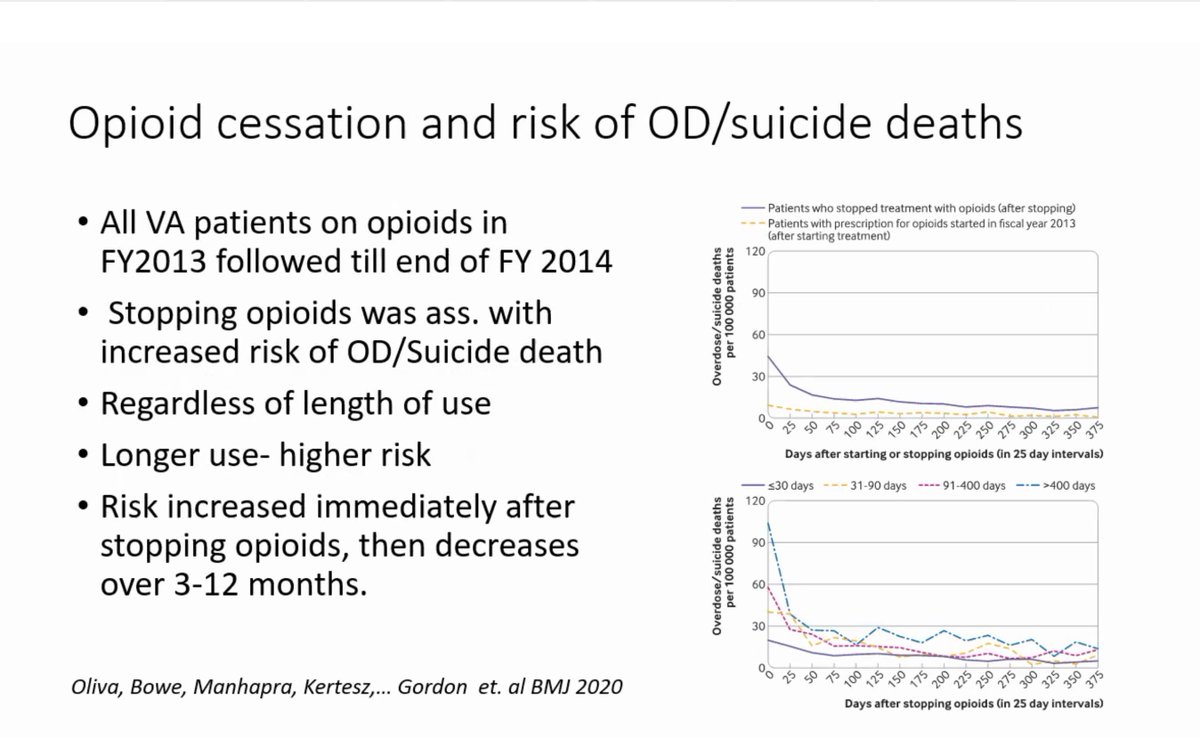
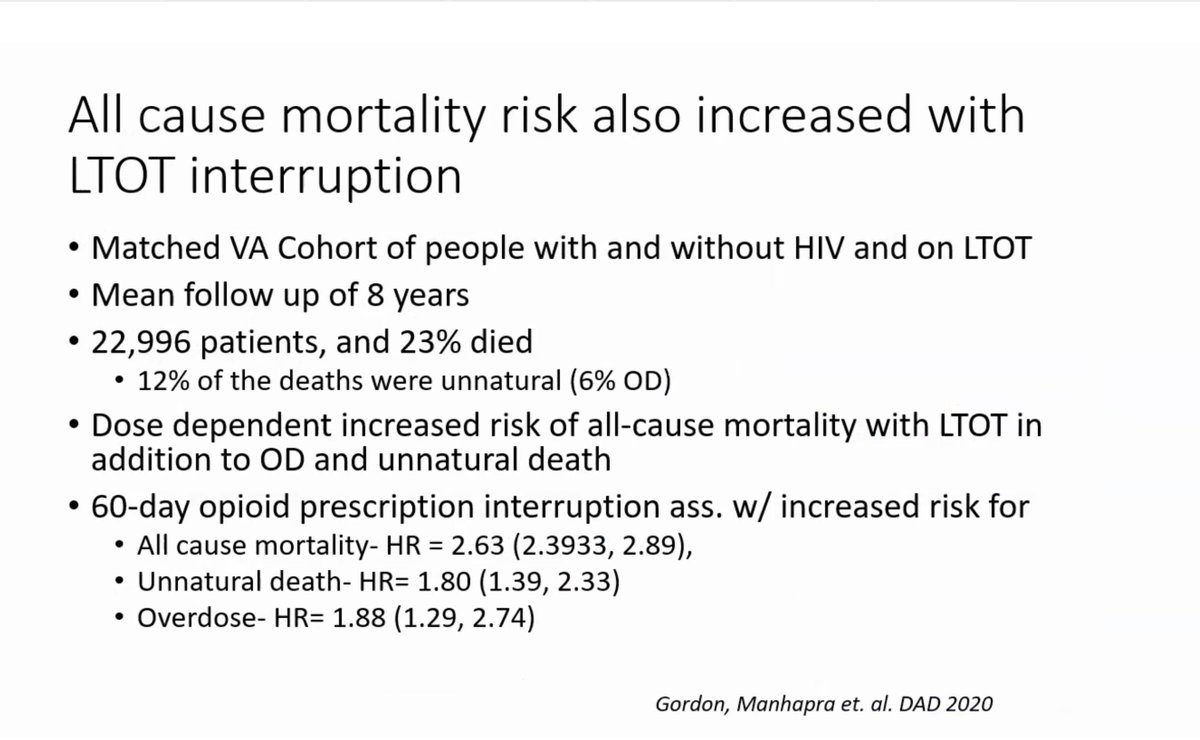
13/Also all cause mortality was elevated after long term opioid therapy interruption in a VA HIV cohort (VACS). Note Dr. Manhapra (like me) is pointing out a fact pattern and NOT arguing every death is Cause and Effect. Humility is called for 
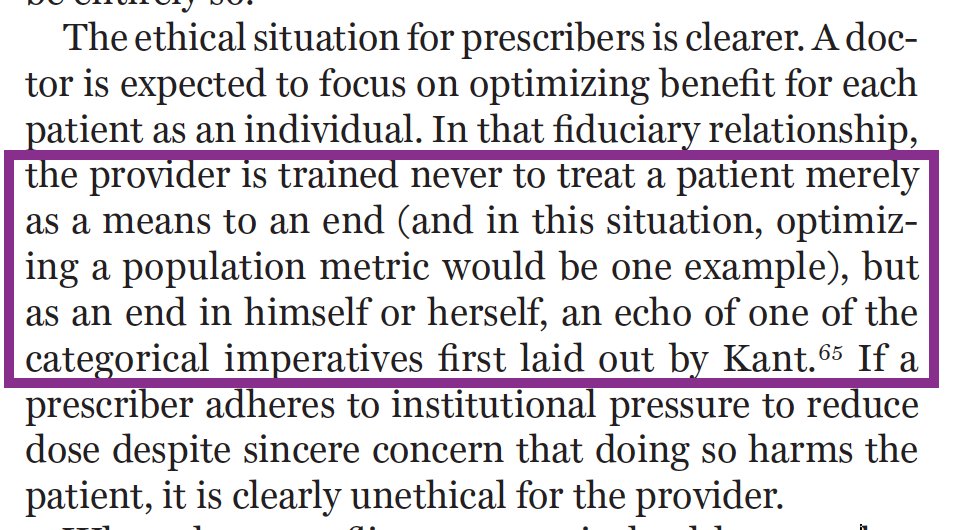
14/In pursuing this discussion I want to highlight issues that we understand are subject to immense dispute because the underlying data are themselves either do not exist or are quite poor
15/If a patient is stable and ostensibly at a higher level of risk for adverse effects from opioids they receive, would reduction of dose make them safer, if they *consented for that personally*? We are aware of *no evidence* although I think it's totally reasonable to discuss
16/If a patient has shown higher-risk problems (like turning up drunk in the ER while also having taken the prescribed opioids, i.e. major overdose risk), do the clinicians make the patient *safer* by switching to buprenorphine as a "safer opioid". FYI: this comes up a lot
17/Please note that honest discussion here has a few limitations. First my friends and I (who discuss these matters with in good faith) often do NOT agree. I am still wrestling with what it would mean to adopt concepts put forward by my friend Ajay. He knows that!
18/Sadly, there are also bad-faith discussants who have slung arrows. Usually, from folks who:
*don't have frontline primary care experience
*don't propose, fund and deliver peer-reviewed research
*are paid by law firms
*discount experiences of people with lived experience
*don't have frontline primary care experience
*don't propose, fund and deliver peer-reviewed research
*are paid by law firms
*discount experiences of people with lived experience
19/The story should be about the people and the families whose care has been upended in part because of poor science, immodesty, and policymakers addiction to "quick fixes"
#Listen (YES: after 19 tweets in a row, that applies to me too)
#Listen (YES: after 19 tweets in a row, that applies to me too)
• • •
Missing some Tweet in this thread? You can try to
force a refresh