1/B
The Santa Clara study co-authored by Bendavid, Bhattacharya, Ioannidis, etc. is now out.
Time to once again cover the reasons why it's very wrong.
medrxiv.org/content/10.110…
"COVID-19 antibody seroprevalence in Santa Clara County, California"
academic.oup.com/ije/advance-ar…
The Santa Clara study co-authored by Bendavid, Bhattacharya, Ioannidis, etc. is now out.
Time to once again cover the reasons why it's very wrong.
medrxiv.org/content/10.110…
"COVID-19 antibody seroprevalence in Santa Clara County, California"
academic.oup.com/ije/advance-ar…
2/B
Let's set aside the funding / conflicts of interest underlying the paper, and other such issues. See @stephaniemlee's insightful reporting on that.
This thread will focus more on the scientific points.
buzzfeednews.com/article/stepha…
buzzfeednews.com/article/stepha…
Let's set aside the funding / conflicts of interest underlying the paper, and other such issues. See @stephaniemlee's insightful reporting on that.
This thread will focus more on the scientific points.
buzzfeednews.com/article/stepha…
buzzfeednews.com/article/stepha…

3/B
Background:
When a virus infects u, your body increases production of proteins known as antibodies, which are usually specific to that virus.
So measuring antibodies lets u estimate who was infected, and from that the infection fatality rate (IFR).
institutefordiseasemodeling.github.io/nCoV-public/an…
Background:
When a virus infects u, your body increases production of proteins known as antibodies, which are usually specific to that virus.
So measuring antibodies lets u estimate who was infected, and from that the infection fatality rate (IFR).
institutefordiseasemodeling.github.io/nCoV-public/an…

4/B
The study measured how many people had this antibody increase, to estimate the number of people infected with SARS-CoV-2. They then calculated IFR by dividing the number of COVID-19 deaths by the number of infected people.
Sound familiar?
The study measured how many people had this antibody increase, to estimate the number of people infected with SARS-CoV-2. They then calculated IFR by dividing the number of COVID-19 deaths by the number of infected people.
Sound familiar?
https://twitter.com/AtomsksSanakan/status/1341186303791149058
5/B
There are at least two main ways to screw up on IFR:
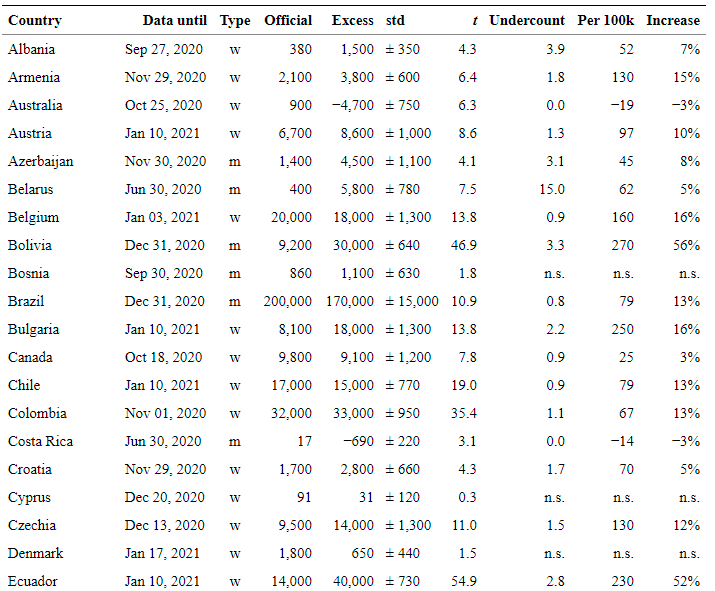
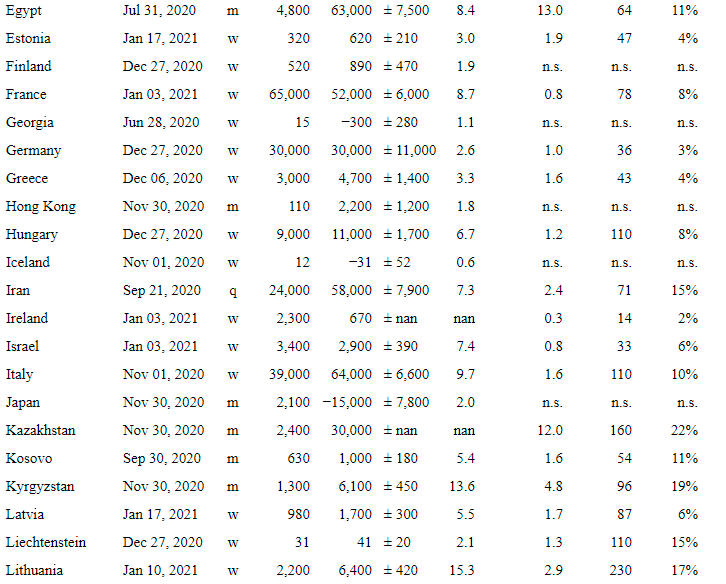
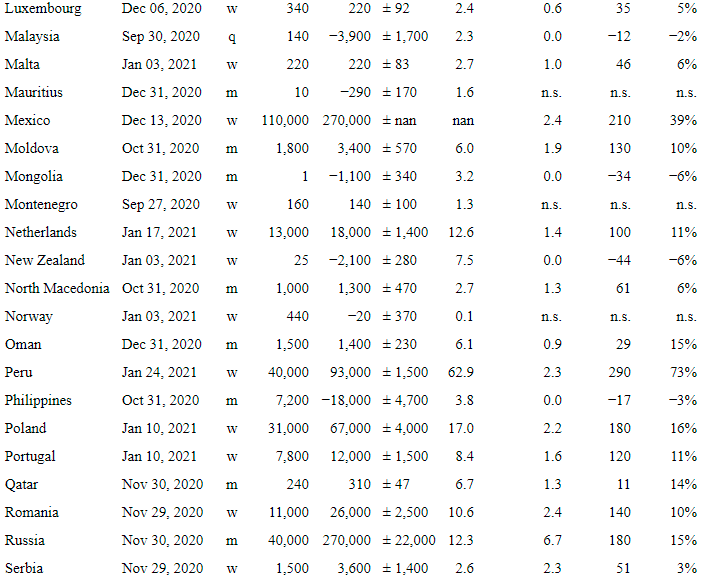
1) get the number of COVID-19 deaths wrong
2) get the number of SARS-CoV-2 infections wrong
The Santa Clara study messes up most badly on point 2.
academic.oup.com/ije/advance-ar…
There are at least two main ways to screw up on IFR:
1) get the number of COVID-19 deaths wrong
2) get the number of SARS-CoV-2 infections wrong
The Santa Clara study messes up most badly on point 2.
https://twitter.com/AtomsksSanakan/status/1336755536294014976
academic.oup.com/ije/advance-ar…

6/B
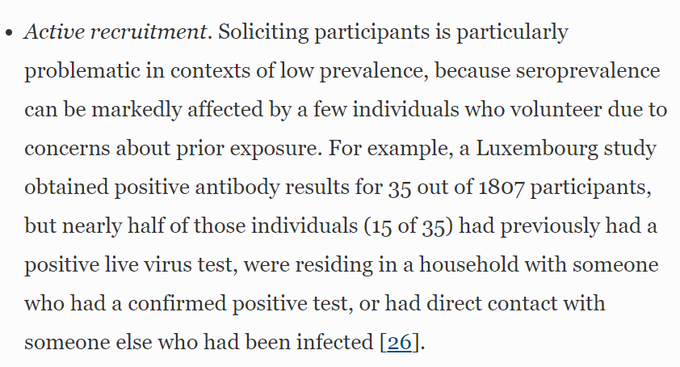
Instead of selecting people at random and focusing on them for testing, they instead use non-randomly-selected volunteers.
That results in a non-representative sample that over-estimates the number of infections.
academic.oup.com/ije/advance-ar…
Instead of selecting people at random and focusing on them for testing, they instead use non-randomly-selected volunteers.
That results in a non-representative sample that over-estimates the number of infections.
https://twitter.com/AtomsksSanakan/status/1341296083767599104
academic.oup.com/ije/advance-ar…

7/B
They did not have to do it this way.
For example, there's another study in Santa Clara that uses randomized sampling (CA-FACTS):
med.stanford.edu/epidemiology-d…
ca-facts.org
link.springer.com/article/10.100…
They did not have to do it this way.
https://twitter.com/GidMK/status/1359705216967315457
For example, there's another study in Santa Clara that uses randomized sampling (CA-FACTS):
med.stanford.edu/epidemiology-d…
ca-facts.org
https://twitter.com/AtomsksSanakan/status/1351992222313574401
link.springer.com/article/10.100…
8/B
They try to adjust (or weight) their sample to make it more representative of the general population in Santa Clara.
That might work if they had randomly selected people. But as we just saw, their sample is non-random.
academic.oup.com/jid/article/22…
They try to adjust (or weight) their sample to make it more representative of the general population in Santa Clara.
That might work if they had randomly selected people. But as we just saw, their sample is non-random.
https://twitter.com/AtomsksSanakan/status/1287615265560309760
academic.oup.com/jid/article/22…

9/B
If @stephaniemlee is correct and misleading information was used to recruit *some* members of the sample, then that should make us even less sure than the sample is randomized.
That is a non-random, unevenly-distributed means of recruiting people.
buzzfeednews.com/article/stepha…
If @stephaniemlee is correct and misleading information was used to recruit *some* members of the sample, then that should make us even less sure than the sample is randomized.
That is a non-random, unevenly-distributed means of recruiting people.
buzzfeednews.com/article/stepha…

10/B
So the Santa Clara study over-estimated the number of infected people by using non-random sampling.
But it also likely did so via the antibody test it uses. @stephaniemlee's shows these complaints from those checking the accuracy of the test:
buzzfeednews.com/article/stepha…
So the Santa Clara study over-estimated the number of infected people by using non-random sampling.
But it also likely did so via the antibody test it uses. @stephaniemlee's shows these complaints from those checking the accuracy of the test:
buzzfeednews.com/article/stepha…

11/B
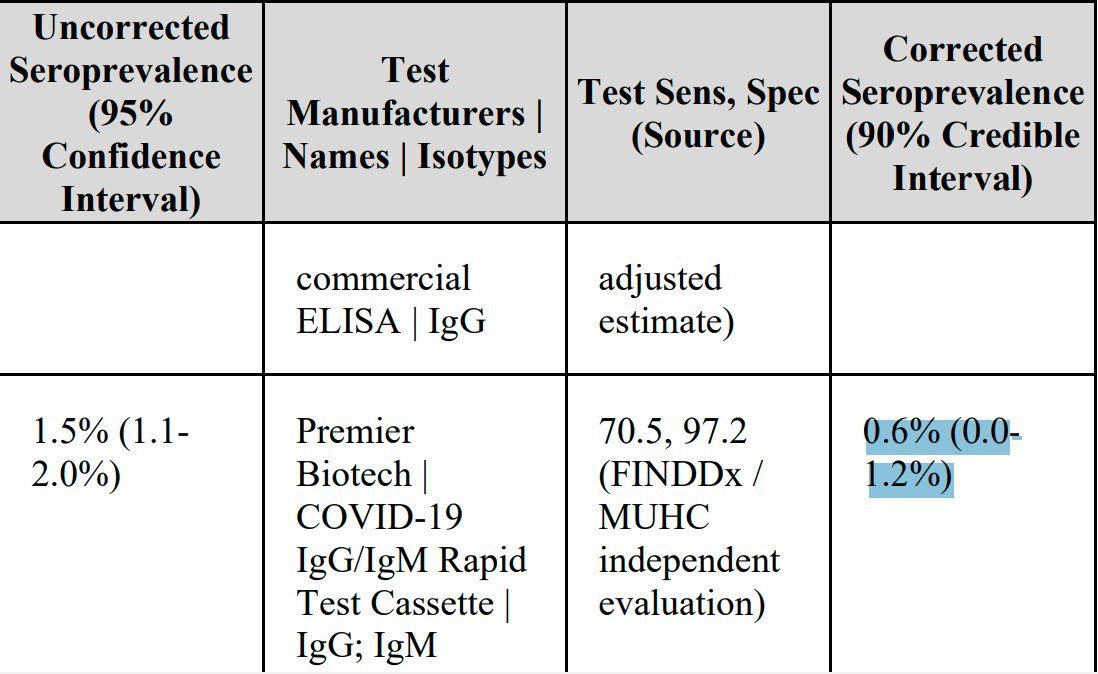
The authors state:
"The raw prevalence of antibodies in our sample was 1.5% [...]. [...] unweighted prevalence adjusted for test-performance characteristics was 1.2% [...]"
academic.oup.com/ije/advance-ar…
Others get lower values:
bfi.uchicago.edu/working-paper/…
medrxiv.org/content/10.110…
The authors state:
"The raw prevalence of antibodies in our sample was 1.5% [...]. [...] unweighted prevalence adjusted for test-performance characteristics was 1.2% [...]"
academic.oup.com/ije/advance-ar…
Others get lower values:
bfi.uchicago.edu/working-paper/…
medrxiv.org/content/10.110…
12/B
Another problem is the authors over-estimating how certain they can be about the accuracy of their antibody test.
medrxiv.org/content/10.110…
Uncertainty may be so large that their results cannot statistically rule out *almost no one being infected.*
rss.onlinelibrary.wiley.com/doi/epdf/10.11…
Another problem is the authors over-estimating how certain they can be about the accuracy of their antibody test.
medrxiv.org/content/10.110…
Uncertainty may be so large that their results cannot statistically rule out *almost no one being infected.*
rss.onlinelibrary.wiley.com/doi/epdf/10.11…

13/B
They defend their case by saying a study on dialysis patients yielded an IFR similar to their's:
academic.oup.com/ije/advance-ar…
That's damning, since dialysis studies over-estimate the number of infections:
link.springer.com/article/10.100…
They defend their case by saying a study on dialysis patients yielded an IFR similar to their's:
academic.oup.com/ije/advance-ar…
That's damning, since dialysis studies over-estimate the number of infections:
https://twitter.com/AtomsksSanakan/status/1309780916311650304
https://twitter.com/AtomsksSanakan/status/1315298454306992128
link.springer.com/article/10.100…

14/B
They defend their results by citing a Los Angeles study (also co-authored by Bendavid + Bhattacharya).
When Ioannidis inferred IFR from that study, it required more people be infected that actually exist.
So it's impossible.
They defend their results by citing a Los Angeles study (also co-authored by Bendavid + Bhattacharya).
When Ioannidis inferred IFR from that study, it required more people be infected that actually exist.
So it's impossible.
https://twitter.com/AtomsksSanakan/status/1335667684361572357
https://twitter.com/AtomsksSanakan/status/1360325606123204608
15/B
There are other problems, but I'll stop here, at least for awhile. It should be clear the study is unreliable.
Interestingly, applying its 0.17% IFR now entails >51% of Santa Clara is infected
coronavirus.jhu.edu/us-map
There goes early herd immunity
There are other problems, but I'll stop here, at least for awhile. It should be clear the study is unreliable.
Interestingly, applying its 0.17% IFR now entails >51% of Santa Clara is infected
coronavirus.jhu.edu/us-map
There goes early herd immunity
https://twitter.com/FoxandtheFlu/status/1334546126880395264
16/B
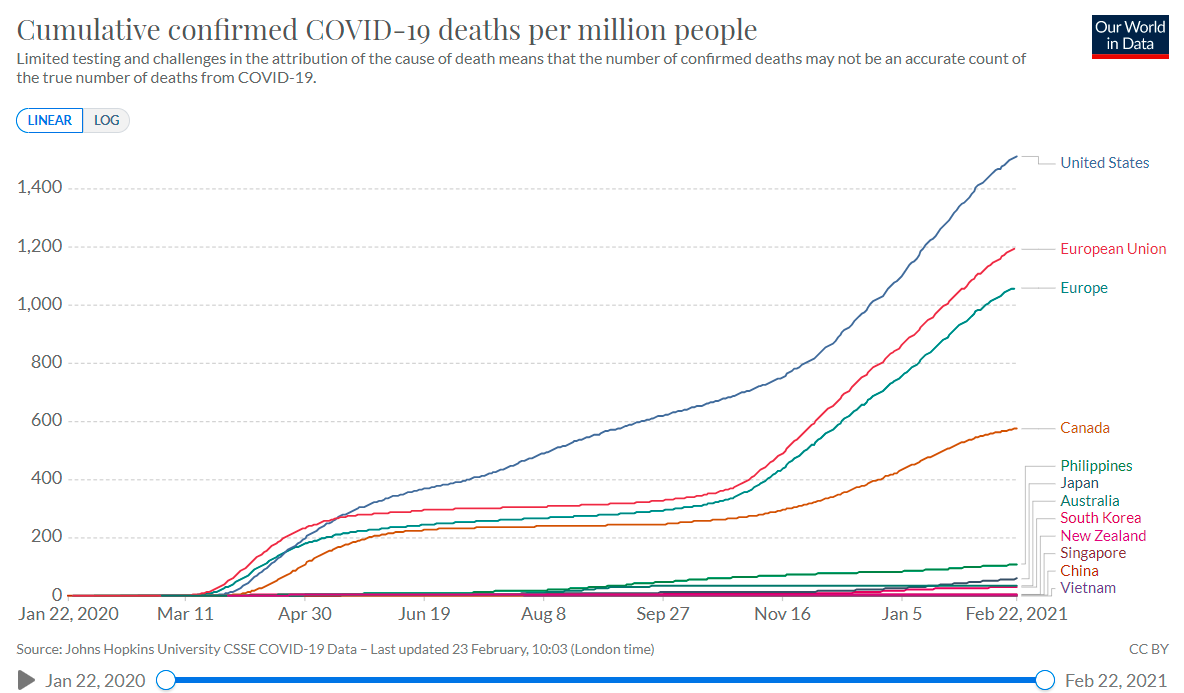
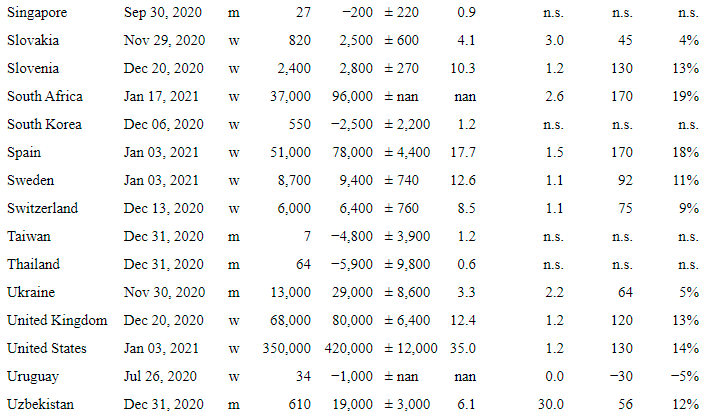
Its IFR is a low outlier, especially in western nations like the USA:
And it was performed during an accelerating outbreak, making it more unreliable:
link.springer.com/article/10.100…
Its IFR is a low outlier, especially in western nations like the USA:
https://twitter.com/AtomsksSanakan/status/1297654625043132416
https://twitter.com/AtomsksSanakan/status/1341189283223384069
https://twitter.com/AtomsksSanakan/status/1343874478670028808
https://twitter.com/AtomsksSanakan/status/1343836703996440577
And it was performed during an accelerating outbreak, making it more unreliable:
link.springer.com/article/10.100…

17/B
Many people are responding by asking how this paper was published.
Context on that below:
Many people are responding by asking how this paper was published.
Context on that below:
https://twitter.com/AtomsksSanakan/status/1362125794848485378
https://twitter.com/siminevazire/status/1364012875950428160
18/B
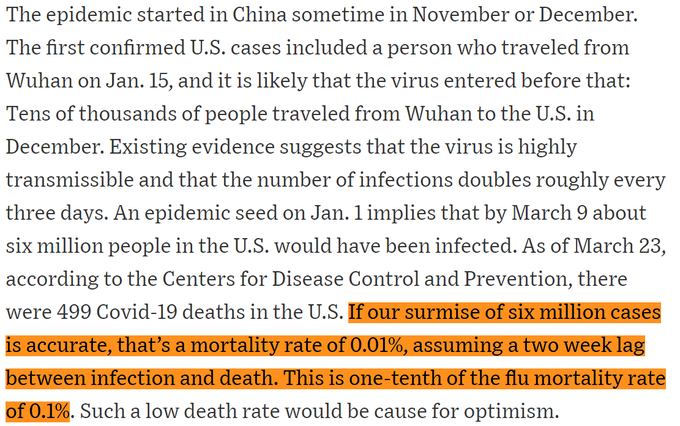
I've been critical of the Santa Clara study, but its IFR estimate of 0.17% represents a substantial improvement over the ~0.01% estimate Bendavid + Bhattacharya gave in late March
~0.01% requires the US population be >14X larger than it actually is
archive.is/QLmJt#selectio…
I've been critical of the Santa Clara study, but its IFR estimate of 0.17% represents a substantial improvement over the ~0.01% estimate Bendavid + Bhattacharya gave in late March
~0.01% requires the US population be >14X larger than it actually is
archive.is/QLmJt#selectio…
19/B
I'd put Santa Clara's IFR between ~0.4% - ~1.0%
@youyanggu's model over-estimates the number of infections
archive.is/eYgGL#selectio…
But even it gives an April IFR of ~0.4% (w/ a 2 week lag for deaths)
web.archive.org/web/2021022318…
coronavirus.jhu.edu/us-map
medrxiv.org/content/10.110…
I'd put Santa Clara's IFR between ~0.4% - ~1.0%
@youyanggu's model over-estimates the number of infections
archive.is/eYgGL#selectio…
But even it gives an April IFR of ~0.4% (w/ a 2 week lag for deaths)
web.archive.org/web/2021022318…
coronavirus.jhu.edu/us-map
medrxiv.org/content/10.110…

• • •
Missing some Tweet in this thread? You can try to
force a refresh