1/ Is bandemia with a normal WBC count concerning for a lethal infection?
It's a very interesting concept which I've faced and will explore below :
#MedTwitter #MedStudentTwitter #FOAMed
It's a very interesting concept which I've faced and will explore below :
#MedTwitter #MedStudentTwitter #FOAMed

2/“Left shift” means that a particular population of cells is “shifted” towards more immature precursors
Josef Arneth (1873-1955) described this left-shift term.
% neutrophils is commonly reported as a "left shift" in the Diff which is incorrect
jamanetwork.com/journals/jama/…
Josef Arneth (1873-1955) described this left-shift term.
% neutrophils is commonly reported as a "left shift" in the Diff which is incorrect
jamanetwork.com/journals/jama/…
3/Mechanical hematologic counters were used early on last century which perpetuated the term" left shift" with the manual counting of immature neutrophils which were towards the left side of the mature cells on the counter. 

4/Now comes the question when you're faced with a left shift with a normal WBC. How significant can this be to considering a serious infection ?
5/An interesting case involved such a situation with a 48 year old pt with pancreatitis.
The pt had a benign presentation, elevated bands of 24% with a normal WBC at 9.8K/mm3 and lipase 102 U/L.
The patient improved after a day of observation.
acoep-rso.org/the-fast-track…
The pt had a benign presentation, elevated bands of 24% with a normal WBC at 9.8K/mm3 and lipase 102 U/L.
The patient improved after a day of observation.
acoep-rso.org/the-fast-track…
6/The question came up- Should the patient have been admitted or discharged with close outpatient follow-up?
Ultimately it was decided to discharge the patient with close followup.
Ultimately it was decided to discharge the patient with close followup.
7/The patient returned to the ED less than 12 hours later with hemorrhagic pancreatitis and was intubated during his inpatient stay and eventually recovered.
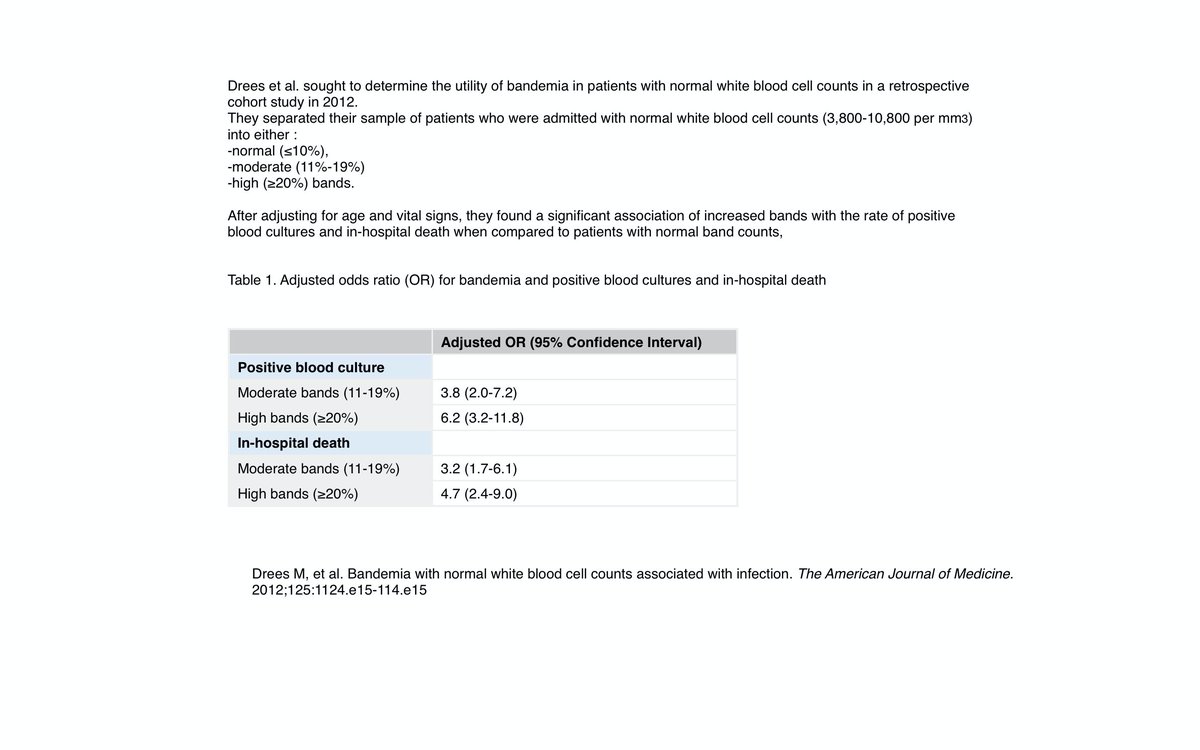
Dress et al determined high bandemia was associated with increasing odds + Blood cx and inpt mortality.
Dress et al determined high bandemia was associated with increasing odds + Blood cx and inpt mortality.
8/Another patient that I encountered with high bands and normal WBC with an suspected infection for weakness. I started pointing alarmingly to the bandemia indicating that it was dangerously high. That patient ended up in the ICU an hour later inspite of our efforts
9/In this paper by Seigel et al:
Bandemia had a sensitivity of 82% for culture proven bacteremia.
jem-journal.com/article/S0736-…
Bandemia had a sensitivity of 82% for culture proven bacteremia.
jem-journal.com/article/S0736-…

11/There are currently no clinical standards by which otherwise healthy-appearing patients with isolated bandemia should be treated with antibiotics and admitted.
Clinicians should understand the value of band counts so they don't delay the Dx or overlook severe infections.
Clinicians should understand the value of band counts so they don't delay the Dx or overlook severe infections.
• • •
Missing some Tweet in this thread? You can try to
force a refresh