
1/
Ever wonder if all #DOACs were created equal? #GITwitter #livertwitter #MedTwitter
Let's start with a poll followed by a #tweetorial on direct oral anticoagulants. First things first, which is your go-to choice of #DOAC ? (COI: none):
Ever wonder if all #DOACs were created equal? #GITwitter #livertwitter #MedTwitter
Let's start with a poll followed by a #tweetorial on direct oral anticoagulants. First things first, which is your go-to choice of #DOAC ? (COI: none):
2/
These agents work "directly" to anti-coagulate and since they are hardly "new' anymore the term #NOAC has become obsolete. Dabigatran is a direct thrombin inhibitor (factor IIa), whereas the others are factor Xa inhibitors (note the Xa in their names)
These agents work "directly" to anti-coagulate and since they are hardly "new' anymore the term #NOAC has become obsolete. Dabigatran is a direct thrombin inhibitor (factor IIa), whereas the others are factor Xa inhibitors (note the Xa in their names)
https://twitter.com/drkeithsiau/status/1372897308921233414?s=20
3/
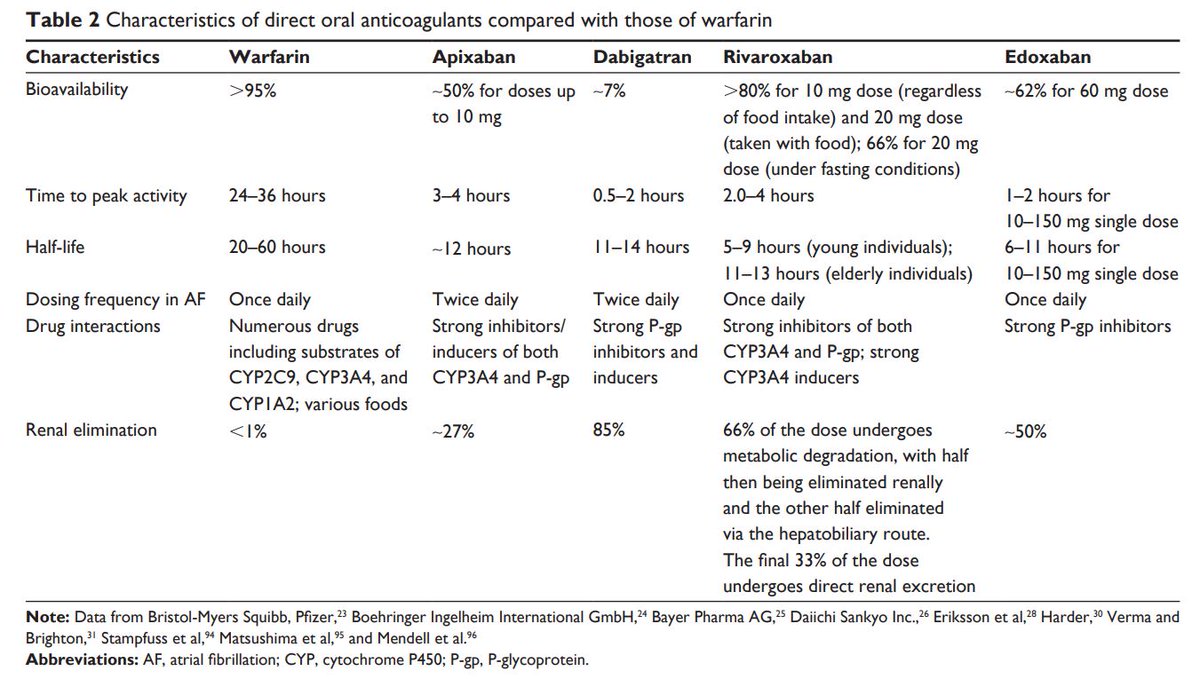
In general they share many characteristics such as a quick onset of action, shorter half-lives, potential for drug-drug interactions (CYP3A4 & P-gp) and renal elimination (except apixaban) when compared with warfarin
ncbi.nlm.nih.gov/pmc/articles/P…
In general they share many characteristics such as a quick onset of action, shorter half-lives, potential for drug-drug interactions (CYP3A4 & P-gp) and renal elimination (except apixaban) when compared with warfarin
ncbi.nlm.nih.gov/pmc/articles/P…
4/
In terms of efficacy many studies have shown that DOACs as a class are equal to or better than warfarin to prevent ischemic stroke and systemic embolism for patients with non-valvular AF, venous thromboembolism (VTE) and even cancer related VTE
In terms of efficacy many studies have shown that DOACs as a class are equal to or better than warfarin to prevent ischemic stroke and systemic embolism for patients with non-valvular AF, venous thromboembolism (VTE) and even cancer related VTE
5/
Another added advantage is the reduction in major bleeding such as intracranial hemorrhage or gastrointestinal bleeding
ahajournals.org/doi/pdf/10.116…
Another added advantage is the reduction in major bleeding such as intracranial hemorrhage or gastrointestinal bleeding
ahajournals.org/doi/pdf/10.116…

6/
How about reversal agents? One drawback initially for #DOACs was a lack of specific antidotes but lately drugs such as idarucizumab for dabigatran reversal, and with andexanet alfa/ciraparantag in the pipeline things will change
How about reversal agents? One drawback initially for #DOACs was a lack of specific antidotes but lately drugs such as idarucizumab for dabigatran reversal, and with andexanet alfa/ciraparantag in the pipeline things will change

8/
At least from the #gitwitter perspective, the latest evidence would suggest that apixaban has the most favourable profile from the #GIB perspective: from an excellent retrospective propensity matched study by @NeenaSAbrahamMD & Co in @AGA_Gastro
gastrojournal.org/article/S0016-…


At least from the #gitwitter perspective, the latest evidence would suggest that apixaban has the most favourable profile from the #GIB perspective: from an excellent retrospective propensity matched study by @NeenaSAbrahamMD & Co in @AGA_Gastro
gastrojournal.org/article/S0016-…



9/
Another piece in @Gut_BMJ showed that apixaban was found to be the safest drug, with reduced risks of major, intracranial, and gastrointestinal bleeding compared with warfarin
bmj.com/content/362/bm…
Another piece in @Gut_BMJ showed that apixaban was found to be the safest drug, with reduced risks of major, intracranial, and gastrointestinal bleeding compared with warfarin
bmj.com/content/362/bm…

10/
Last but not least a paper just out recently by @CUHKMedicine in @Gut_BMJ that explored #DOAC and the risk of post-polypectomy bleeding #PPB showing that apixaban was associated with a ⬇ risk of #PPB and thromboembolism, particularly in the elderly and patients with R polyps
Last but not least a paper just out recently by @CUHKMedicine in @Gut_BMJ that explored #DOAC and the risk of post-polypectomy bleeding #PPB showing that apixaban was associated with a ⬇ risk of #PPB and thromboembolism, particularly in the elderly and patients with R polyps

11/
An additional footnote is that the original trials of apixaban do include a substantial number of patients with moderate renal impairment down to 30 mL/min and they didn't just extrapolate from pre-clinical data
nejm.org/doi/full/10.10…
An additional footnote is that the original trials of apixaban do include a substantial number of patients with moderate renal impairment down to 30 mL/min and they didn't just extrapolate from pre-clinical data
nejm.org/doi/full/10.10…

12/
At the end of the day the best anticoagulant is the one that the patient takes
But the current body of evidence does seem to suggest that apixaban has a more favourable profile when compared with the other #DOACs
At the end of the day the best anticoagulant is the one that the patient takes
But the current body of evidence does seem to suggest that apixaban has a more favourable profile when compared with the other #DOACs
@jalpa_devi @HangVietDao1 @wee_khoon @kin_choon @GianlucaPellino @Qiao_YQ @dr_koko28 @KM_Pawlak @ZorronCTPu @DrMohdZein @PerelmansPearls @RobertoSimonsMD @ShaziaMSiddique @KralJan @allonkahn @Samir_Grover @kdevanimd @shanilkadir @drmoutaz @KMonkemuller
#JGHambassador #gigang
#JGHambassador #gigang
@hanaeboutallaka @sang_hyoung @bverstockt @QueirozNataliaF @KralJan @mjayoushe @IBD_Sir @ibd_afzali @ibdtweets @MarcWong_HK @VWSWong @renumathyd @omar_elshaarawy @DeMadaria @jinendrasatMD @HyeWonLee20 @VivianOrtizMD @TyngYuan @scumaliefe @drmoutaz @drkeithsiau @AtoosaRabiee #GOAL
@gilbenyakov @KapuriaMd @jturnesv @ZarathustrMehta @sconglymd @KralJan @andrewMMoon @LizzieAbyMD @jasmohanbajaj @HenryEChang @rrosenblattmd @ebtapper @SanchezLunaMD @ZaheerNabi8 @ChantaTanya @KM_Pawlak @carolmangas @tomtielleman @CarvalloP_MD @KralJan @AhmadBazarbashi
@hassaanziaMD @vaibhav_manu @BilalMohammadMD @ZachSmithGI @drdalbir @SunilAminMD @anatoliiBorodin @SighPichamol @PopovVioleta @Samir_Grover @tberzin @Alxmd @shanilkadir @ealjahdli @ScopingSundays @EndoCollabcom @LiverFellow @BSGTrainees @TomTielleman @ASGEendoscopy @SAGES_Updates
@drwong_martin @enrrikke @doctornikkid @Mister_trip @Kh_Saidani @jaumebosch9 @GI_Guy @KellyHathornMD @DrBuHayee @NEndoscopy @ChahalPrabhleen @EndoscopyCampus @endoscopyworks @EndoscopyNow @BritSocGastro @SEEDendoscopia @EndoCollabcom @maangelchokan @OncoViews @drabbyphilips
easter eggs: notable mention for dabigatran. As a pro-drug with low bioavailability the unabsorbed drug may be converted to active dabigatran in the distal bowel and then excreted in the feces. ?cause of GIB and the mucosal injuries per @lean_stein
https://twitter.com/lean_stein/status/1373039028803620865?s=20
• • •
Missing some Tweet in this thread? You can try to
force a refresh



