Q: Did your nation’s pandemic flu plan require N95/FFP3, or FRSM for HCW protection?
TOP SECRET: AEROSOL TRANSMISSION MESSAGE TO BE SUPPRESSED AT ALL COSTS
#COVIDisAirborne
/1
TOP SECRET: AEROSOL TRANSMISSION MESSAGE TO BE SUPPRESSED AT ALL COSTS
#COVIDisAirborne
/1

‘There is considerable support in the scientific literature for a contribution of aerosol transmission to the spread of influenza A, which has been reviewed elsewhere (Tellier 2006).’
/2
/2

‘Briefly, supportive evidences include the prolonged persistence of infectivity in aerosolized influenza A virus at low humidity, the transmission to volunteers of influenza by aerosols, reproducing the full spectrum of disease, at doses much smaller than the doses required..’
.. by intranasal drop inoculation (which mimics large droplet trans- mission), and the interruption of transmission of influenza by blocking the aerosol route through UV irradiation of upper room air’
/4
/4
‘Generation of a large number of aerosol particles by coughing or sneezing has been documented for a long time (reviewed in Nicas et al. 2005).’
@doctimcook @microlabdoc
/5
@doctimcook @microlabdoc
/5

‘It is often less appreciated that exhalation during normal breathing also produces aerosol particles. A recent study has confirmed the production of aerosol size particles by normal breathing, & confirmed..the size of the majority of the particles exhaled by mouth is </=1micron’ 

‘Fabian and colleagues (2008) have recently directly detected influenza virus RNA [using RT-PCR] in aerosol particles generated by normal breathing in patients with influenza and collected through an oronasal facemask.’
/7
/7

Not that you need to be told but:
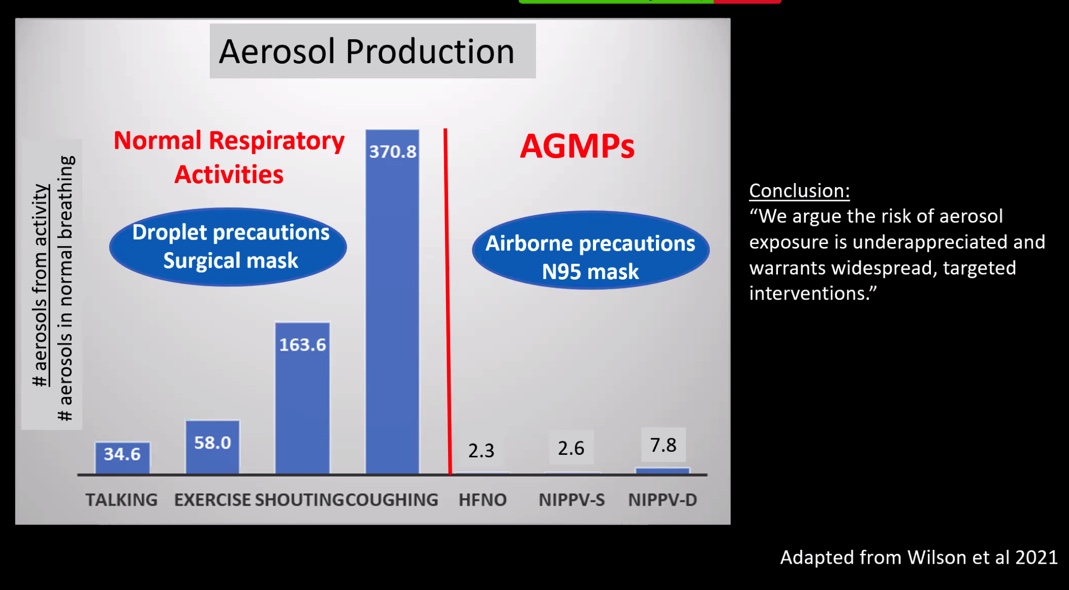
‘Particles of 5 microns or less have a significant penetration into the respiratory tract all the way to the alveolar region (30% penetration for <5 micron particles); penetration into the alveolar region rapidly diminishes beyond 5 microns’
/8
‘Particles of 5 microns or less have a significant penetration into the respiratory tract all the way to the alveolar region (30% penetration for <5 micron particles); penetration into the alveolar region rapidly diminishes beyond 5 microns’
/8

Aside: SARS-CoV-2 target *alveolar* type II pneumocytes, binding via ACE2 assisted by TMPRSS2.
/9
sciencedirect.com/science/articl…
/9
sciencedirect.com/science/articl…
Back to flu:
‘Increasing evidences point towards a role for aerosol transmission in the spread of influenza, at least over short distance where exposure to both aerosol and large droplets occurs.’
/10
‘Increasing evidences point towards a role for aerosol transmission in the spread of influenza, at least over short distance where exposure to both aerosol and large droplets occurs.’
/10

Implications (2009):
‘Precautions should include the use of an N95 respirator (or better) when appropriate, including in close proximity of an infected patient’
/11
‘Precautions should include the use of an N95 respirator (or better) when appropriate, including in close proximity of an infected patient’
/11

Q: Did your nation’s pandemic flu plan require N95/FFP3, or FRSM for HCW protection?
#COVIDisAirborne
#COVIDisAirborne
• • •
Missing some Tweet in this thread? You can try to
force a refresh