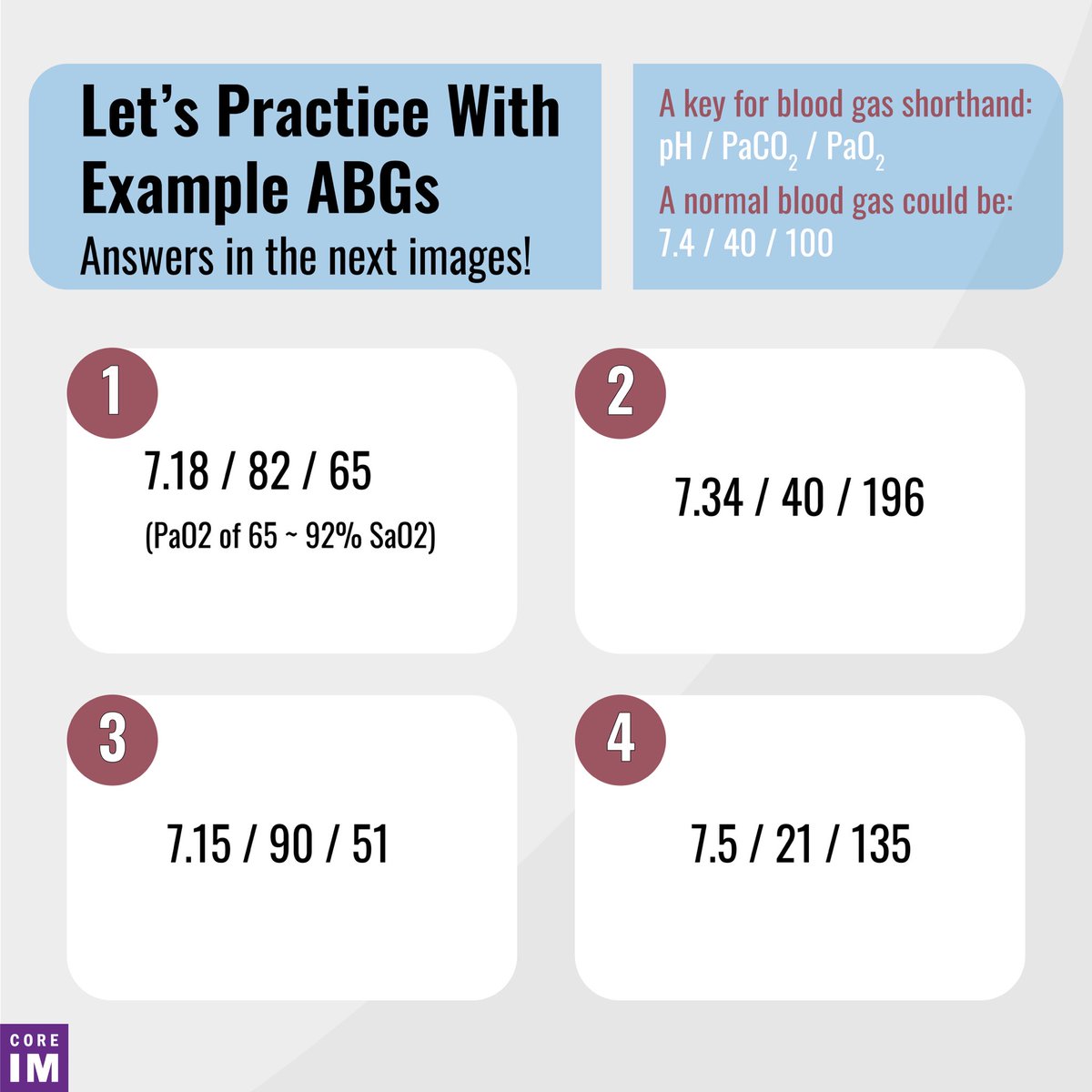
1/ Good morning, #MedTwitter, and happy Tuesday! We’re excited to bring you our latest installment of #ReadingRoom today. Dim the lights; it’s time to clinically correlate!
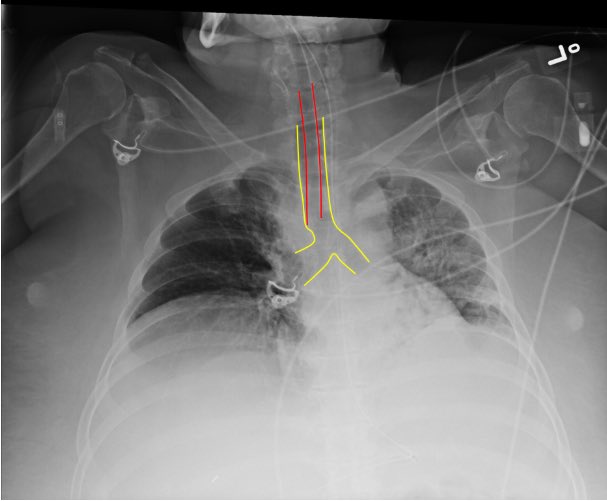
What object is labeled in the CXR below? What is it used for?
What object is labeled in the CXR below? What is it used for?

2/ That, friends, is our dear friend: the NG tube. It is our portal for tube feeds and PO meds (technically Per Nasus?), or if you put the thing down flip it and reverse it you can use the NGT to decompress the stomach. 

3/ Next question: should you place that order that says “OK to use NG tube”?
The graphic below shows a systematic approach to ensure correct placement. This one is good to go!
The graphic below shows a systematic approach to ensure correct placement. This one is good to go!

5/ This one is distinctive because of its thick, weighted tip - a Dobhoff.
Drs. Dobbie & Hoffmeister invented the smaller, more flexible tube, and added a metal tip wrapped in silicone in an attempt to increase the chances of successful placement.
Drs. Dobbie & Hoffmeister invented the smaller, more flexible tube, and added a metal tip wrapped in silicone in an attempt to increase the chances of successful placement.

6/ And that’s it for this week’s #ReadingRoom! You can find this post and more on our website: coreimpodcast.com/2021/04/13/wha…
Credits
Graphics: @SalimNNajjar Content: @TomMulveyMD
Credits
Graphics: @SalimNNajjar Content: @TomMulveyMD
• • •
Missing some Tweet in this thread? You can try to
force a refresh