SARS-CoV-2 routes of transmission & recommendations for preventing acquisition: joint @biainfection, @HIS_infection, @IPS_Infection & @RCPath guidance.
@loveebhc @dr_jas_islam @microlabdoc @trishgreenhalgh @kprather88 @DFisman @zeynep @jljcolorado
journalofhospitalinfection.com/article/S0195-…
@loveebhc @dr_jas_islam @microlabdoc @trishgreenhalgh @kprather88 @DFisman @zeynep @jljcolorado
journalofhospitalinfection.com/article/S0195-…
I am sorry I can only copy two lead authors directly, but I would like to thank all authors for acting on their high sense of responsibility towards improving public health.
I am also sorry I could not reply within the 7-day window you provided for 'stakeholder feedback'.
I am also sorry I could not reply within the 7-day window you provided for 'stakeholder feedback'.

I hope you don't mind a Q?
Given:
- Epidemiological studies support airborne transmission
- Presence of virus RNA in the air, air vents/exhausts/ducts/filters
- Presence of virus RNA in exhaled breath
- Airborne viability up to 16 hours
- Presence of live virus in the air
...

Given:
- Epidemiological studies support airborne transmission
- Presence of virus RNA in the air, air vents/exhausts/ducts/filters
- Presence of virus RNA in exhaled breath
- Airborne viability up to 16 hours
- Presence of live virus in the air
...


I hope you don't mind me suggesting that you are being 'obtuse' in stating:
'Overall decision for likelihood of transmission
Droplet: probable
Airborne: possible (in some circumstances, especially AGPs)'
Surely these data provide proof of airborne SARS-CoV-2 transmission?
'Overall decision for likelihood of transmission
Droplet: probable
Airborne: possible (in some circumstances, especially AGPs)'
Surely these data provide proof of airborne SARS-CoV-2 transmission?

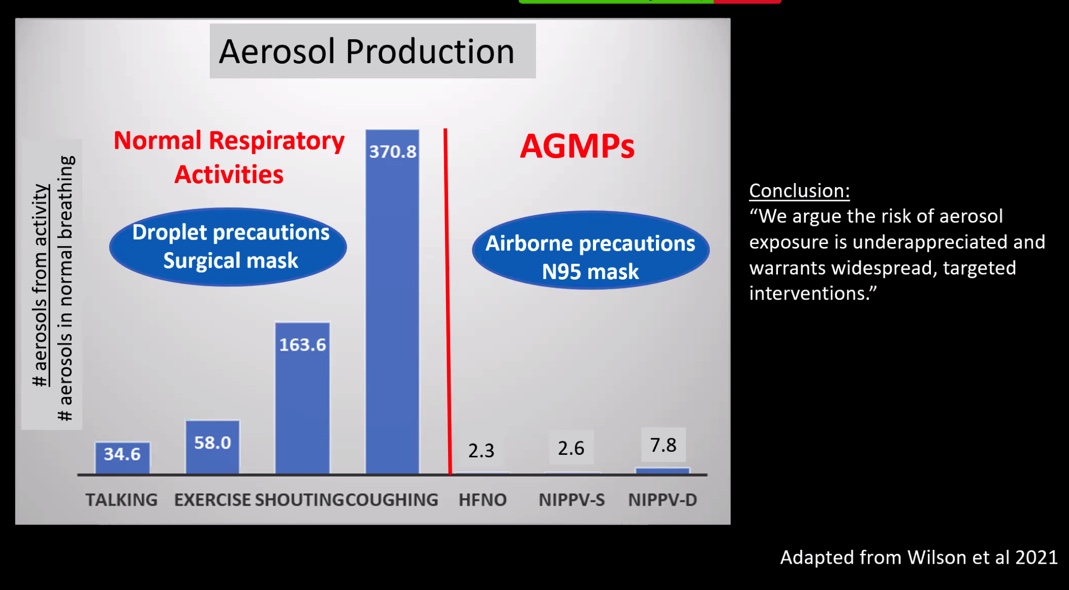
Furthermore, I am staggered that you remain anchored on the preeminent importance of AGPs towards airborne transmission. Have you not seen these data (Oct 2020) indicating far greater aerosol release during coughing? @ShellyMBoulder @linseymarr
https://twitter.com/ShellyMBoulder/status/1326926606263218177?s=20
Lastly, stating that "SARS-CoV-2 appears to spread via the routes commonly implicated in transmission of other respiratory viruses" highlights the success of those with vested interests in suppressing the message that respiratory viral transmission is airborne!
Pic @Don_Milton

Pic @Don_Milton


Last Q: why is it so important for you & other 'experts' to suppress the message that for SARS-CoV-2 (& other respiratory viruses, like influenza), human-to-human transmission occurs *predominantly* via the airborne route?
I hope you can help me understand
I hope you can help me understand
https://twitter.com/DRTomlinsonEP/status/1380218872343756801?s=20
• • •
Missing some Tweet in this thread? You can try to
force a refresh