There are a lot of #LongCOVID gems in this webinar from HCA Healthcare UK. I'm going to try to tweet them succinctly:
1. Non-hospitalized COVID patients had a slower recovery than hospitalized patients.

1. Non-hospitalized COVID patients had a slower recovery than hospitalized patients.
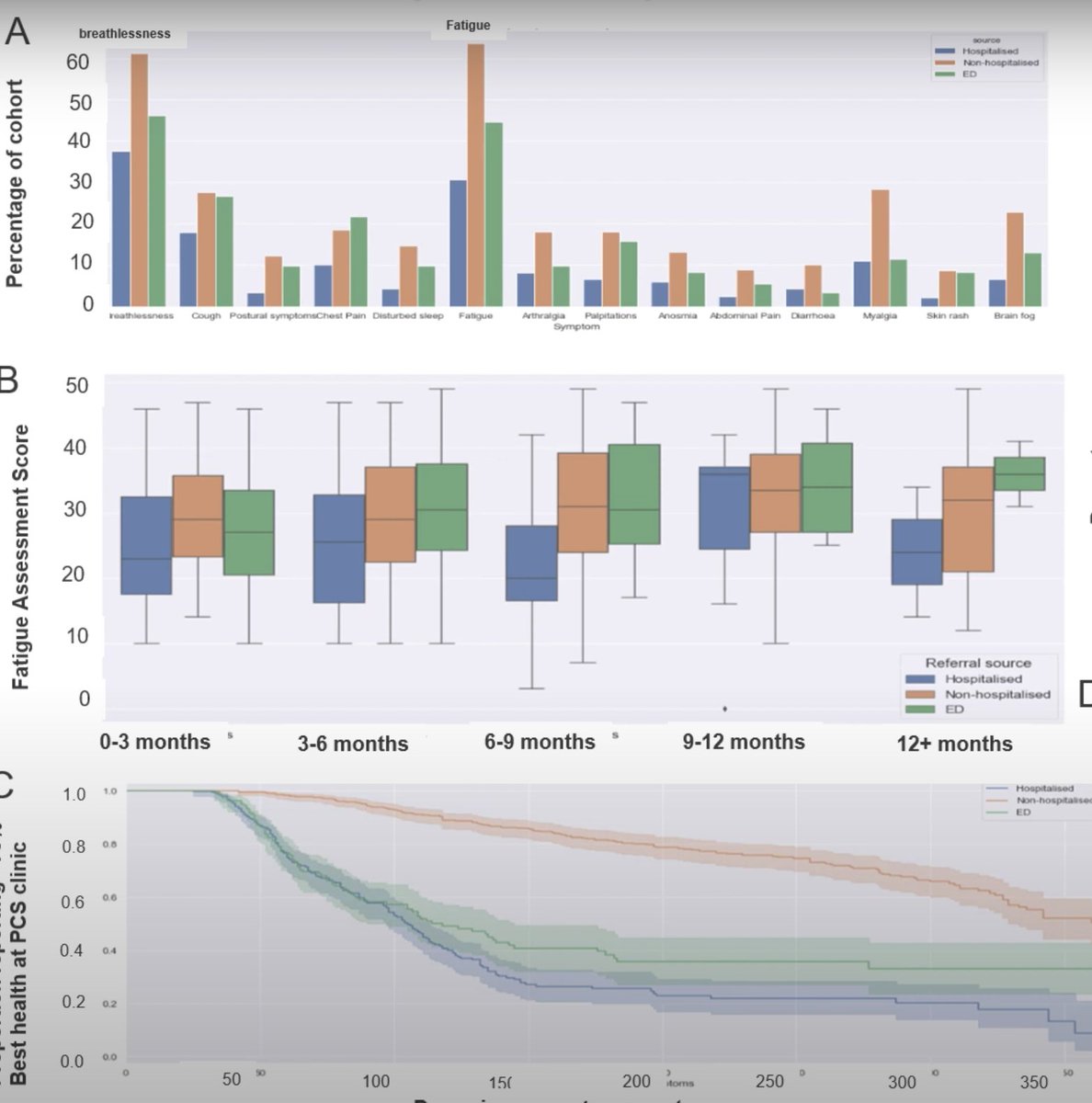
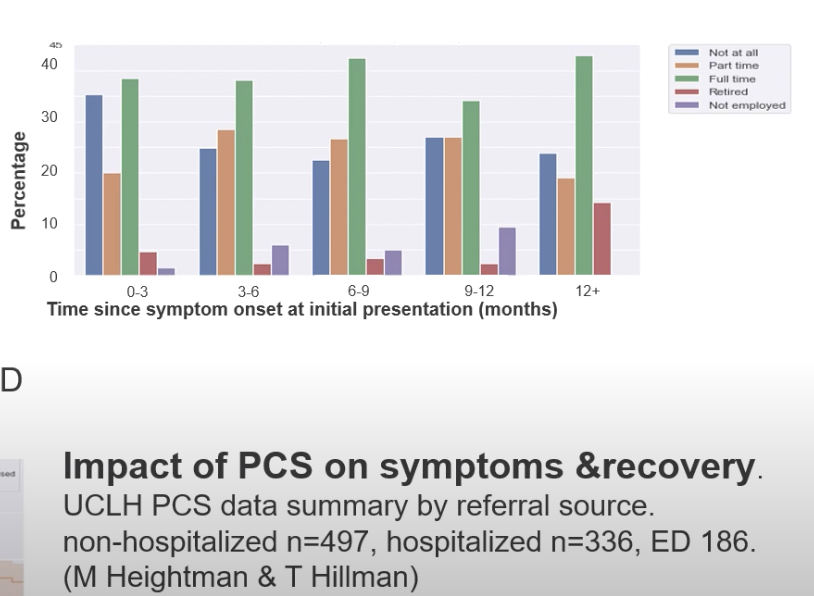
2. At 12 months out, the majority of non-hospitalized #LongCOVID patients are still not back to work full time. 
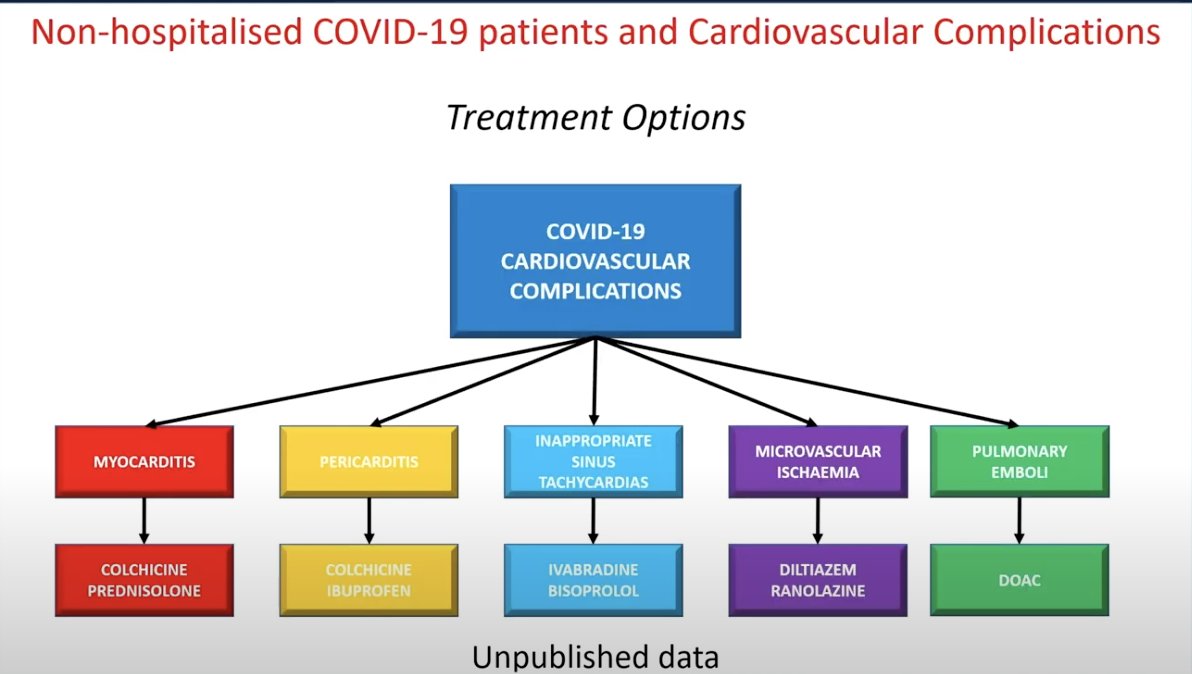
Next speaker is a cardiologist.
3. Cardiac MRIs are helpful. Even when they look normal from a functioning standpoint, supepicardial late gadolinium enhancement can be identified, showing post-viral myocarditis. (Screenshotted case was in a patient 200+ days out from onset).
3. Cardiac MRIs are helpful. Even when they look normal from a functioning standpoint, supepicardial late gadolinium enhancement can be identified, showing post-viral myocarditis. (Screenshotted case was in a patient 200+ days out from onset).
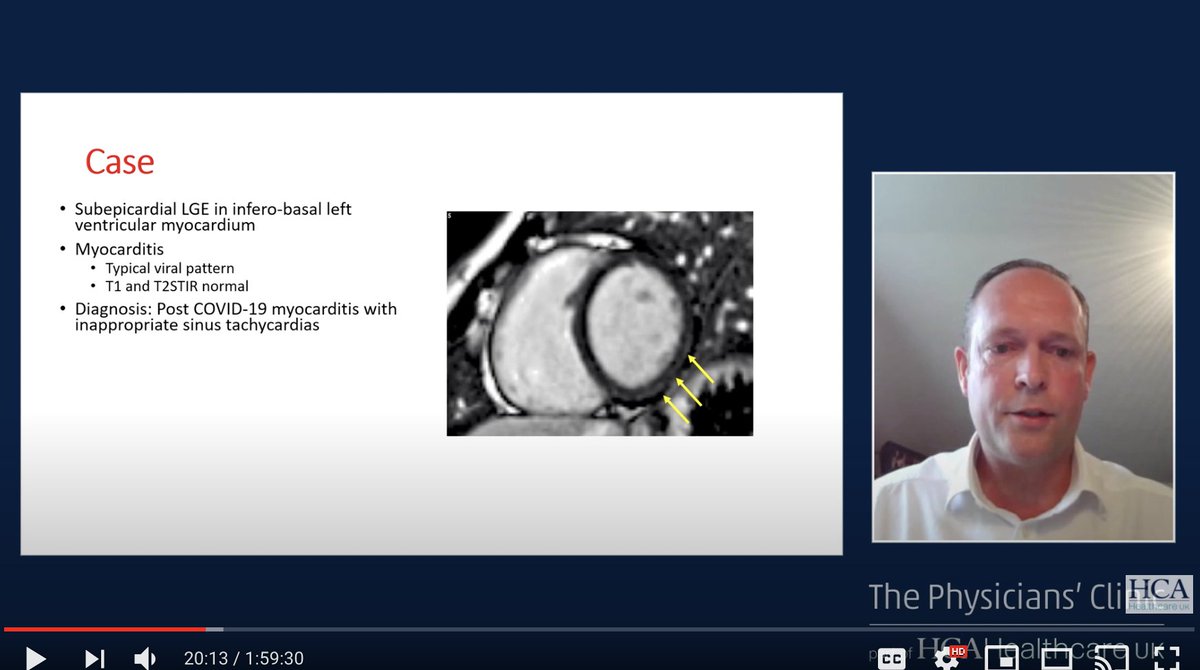
4. The case above had normal X-ray and normal echo. Treatment here included colchicine (3 month course) and ivabradine. Some fatigue and brain fog improved!
#LongCOVID
#LongCOVID
5. A list of blood tests and cardiac imaging to do in #LongCOVID patients (though all of these can come back normal as well). 
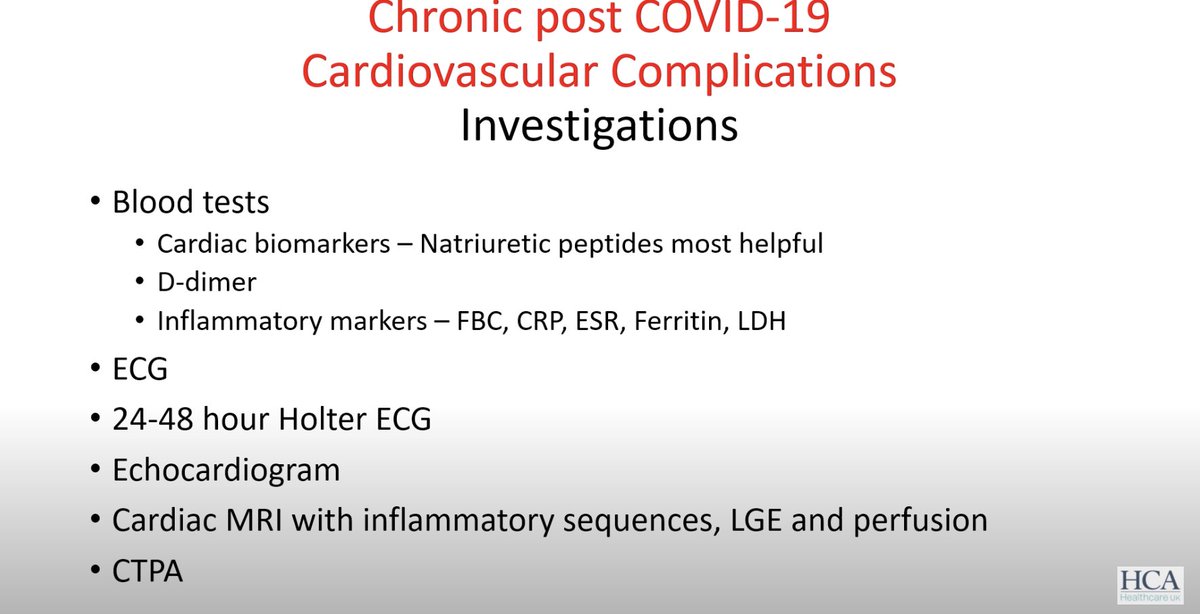
7. In summary, "cardiac MRIs are what I've found most helpful". #LongCOVID
8. He has seen patients with these same cardiac symptoms after the vaccine. He expected that they'd had COVID and not known, but 5 of the patients had never had COVID.
Next up is a neurologist.
9. Endotheliitis of the brain vessels is possible, a likely cause of neurologic sequelae, though there may other be factors.
9. Endotheliitis of the brain vessels is possible, a likely cause of neurologic sequelae, though there may other be factors.
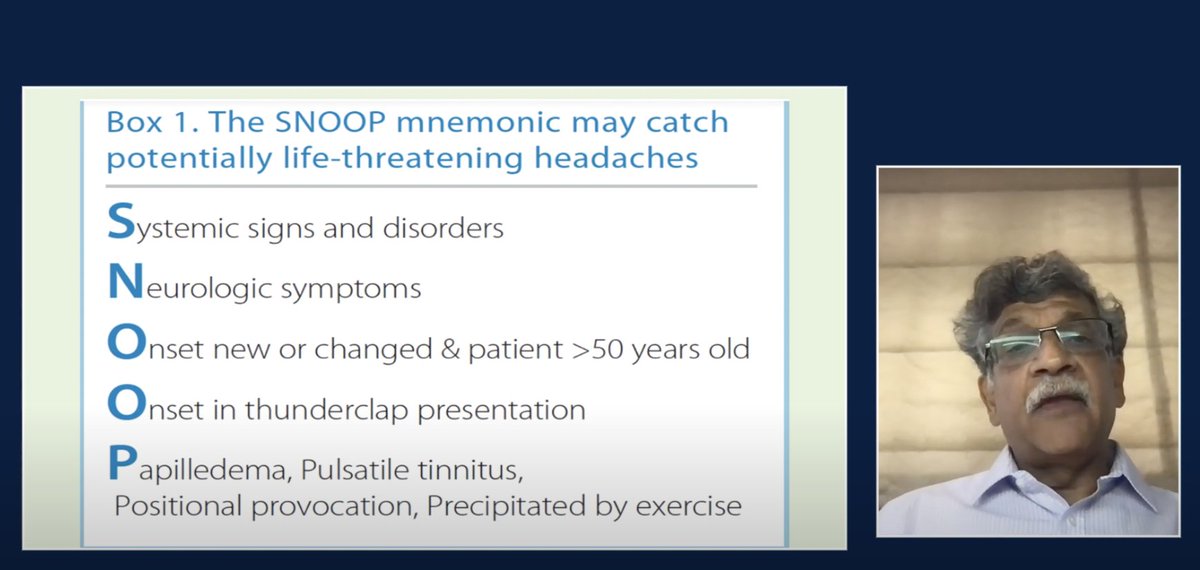
10. Here are a list of warning signs in headaches to look out for. I particularly find the pulsatile tinnitus symptom interesting since that's a common symptom (he mentions it as a sign of intracranial pressure). 
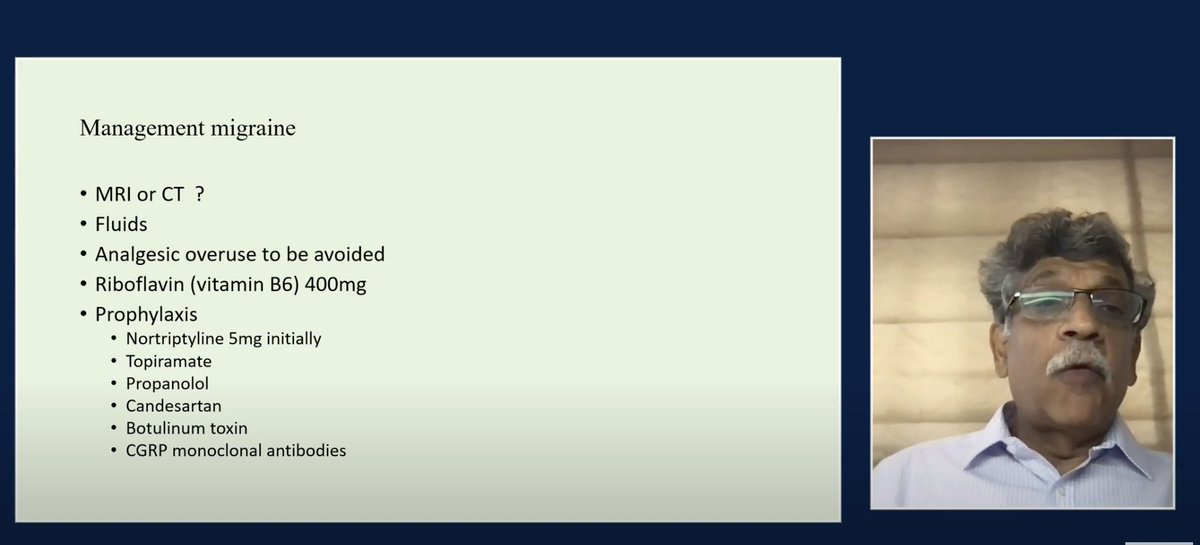
11. #LongCOVID migraine management (~46:30) - some of these are contraindicated with cardio symptoms: 
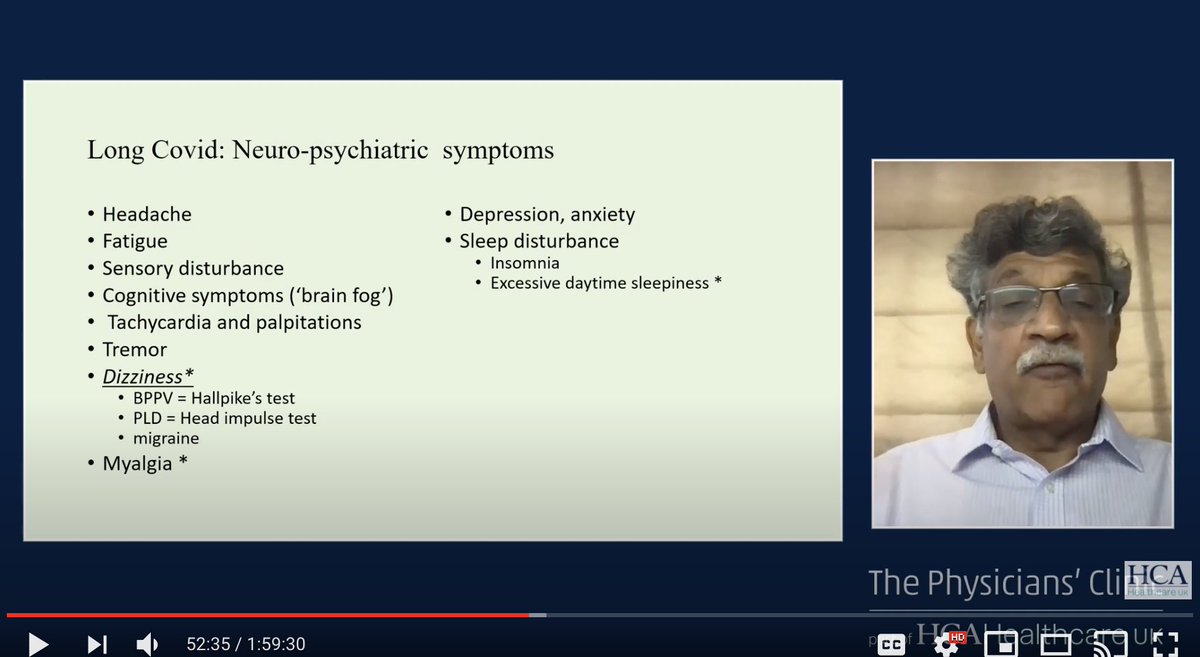
12. He mentions there are 3 types of #LongCOVID dizziness which can be identified.
He also mentions that patients with brain fog need to do cognitive pacing!
He also mentions that patients with brain fog need to do cognitive pacing!
Next up: hematological complications of #LongCOVID:
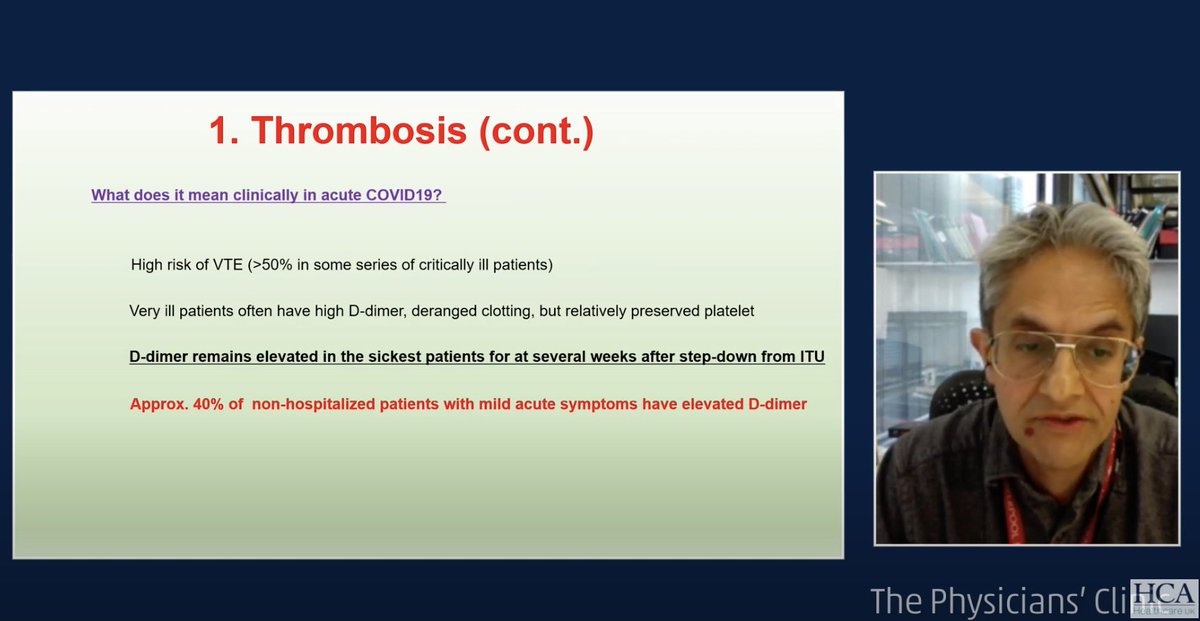
13. About 40% of non-hospitalized patients with mild symptoms have elevated D-Dimer:
13. About 40% of non-hospitalized patients with mild symptoms have elevated D-Dimer:
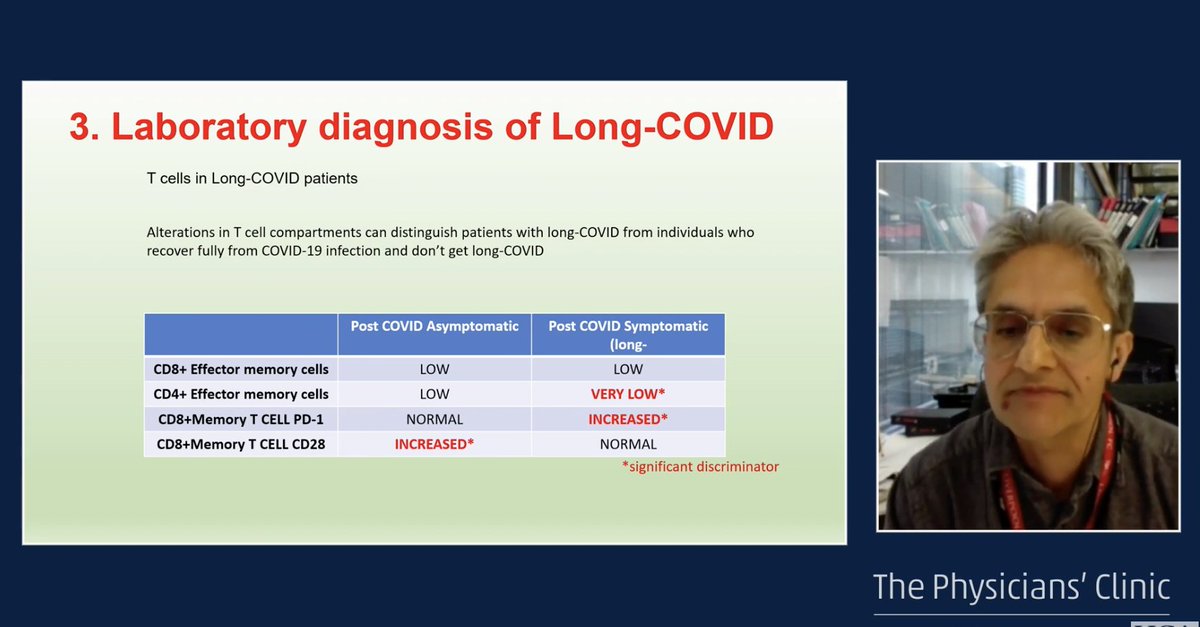
14. There are obvious T-cell differences in patients with #LongCOVID (these are all mild, non-hospitalized patients), particularly having low CD4+ effector memory cells: 
Next up is a talk on treatment strategies, though he starts by saying there are very few.
15. Four key barriers to recovery include 1) poor gut health, 2) overexertion, 3) overworking, and 4) sleep disruption.
From what he sees, patients with any of these don't recover quickly.
15. Four key barriers to recovery include 1) poor gut health, 2) overexertion, 3) overworking, and 4) sleep disruption.
From what he sees, patients with any of these don't recover quickly.
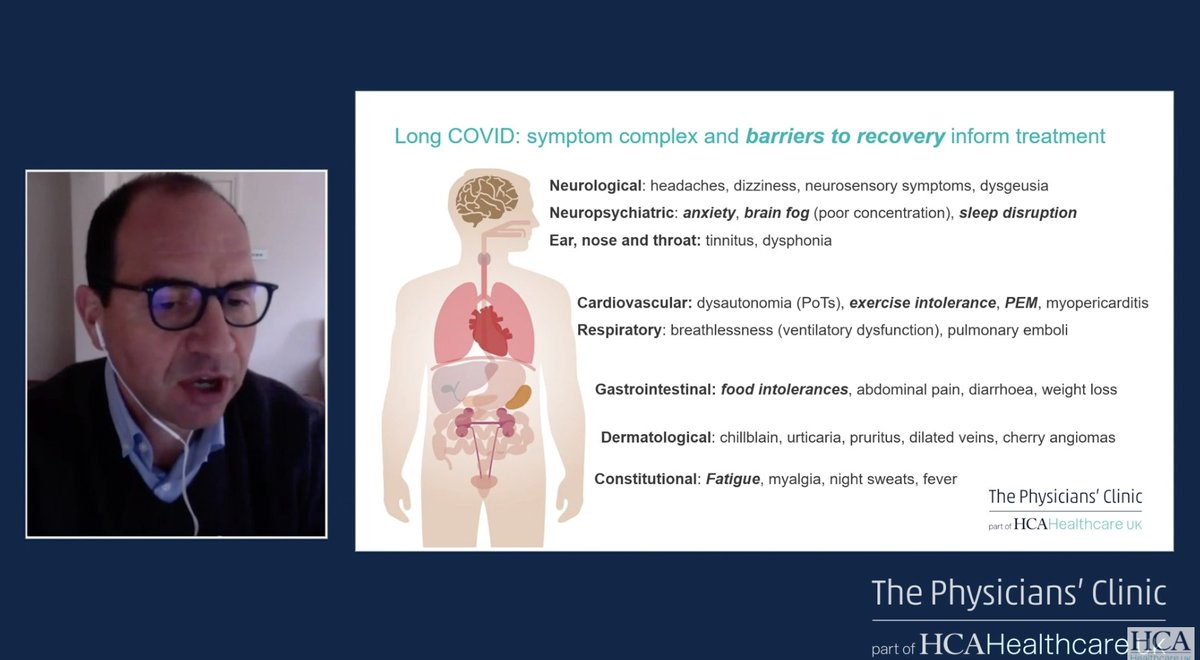
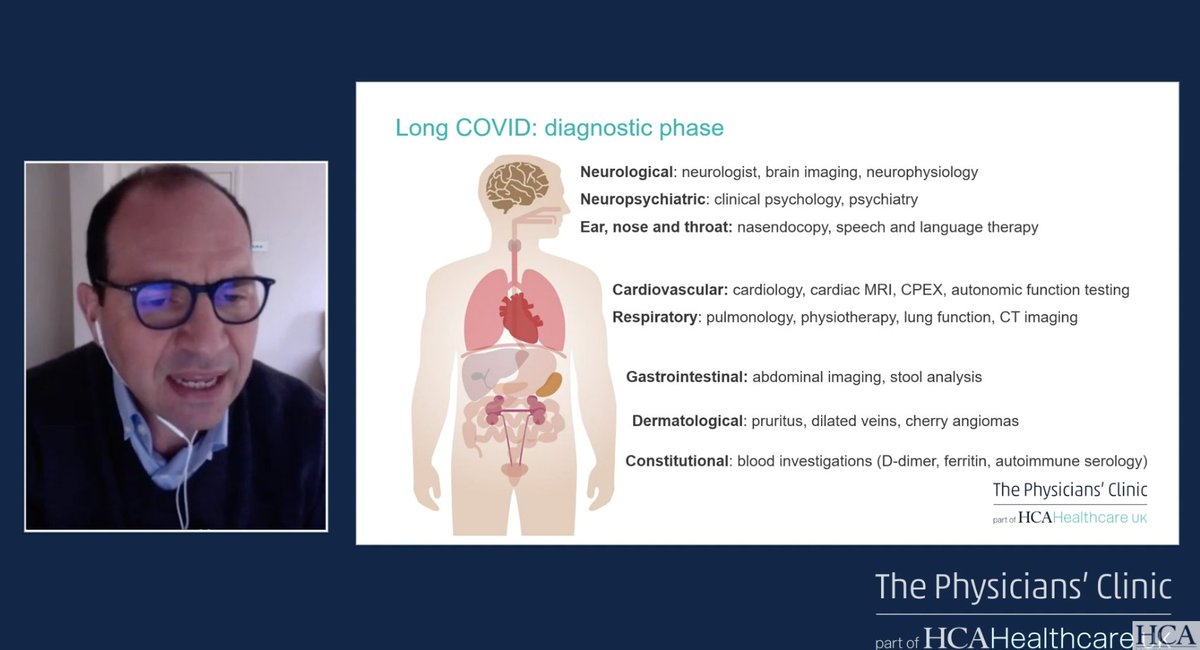
16. Ear/Nose/Throat deserves a specific mention. Speech & language, vocal therapy are important. Autonomic function testing is important. Respiratory therapy for those with breathing issues. Some need GI imaging. Some do develop autoimmune issues, even a year later. #LongCOVID 
17. Interestingly, he mentions that of patients who have PTSD, they have "health-related/long combat PTSD", which does NOT get treated with CBT or other forms of psychotherapy. #LongCOVID
18. He recommends probiotics like Symprove (side note - I strongly agree with this provided it's a good probiotic like Align or ABX Support). #LongCOVID
19. "The strategy of physical and psychological therapy does not work for these patients." #LongCOVID
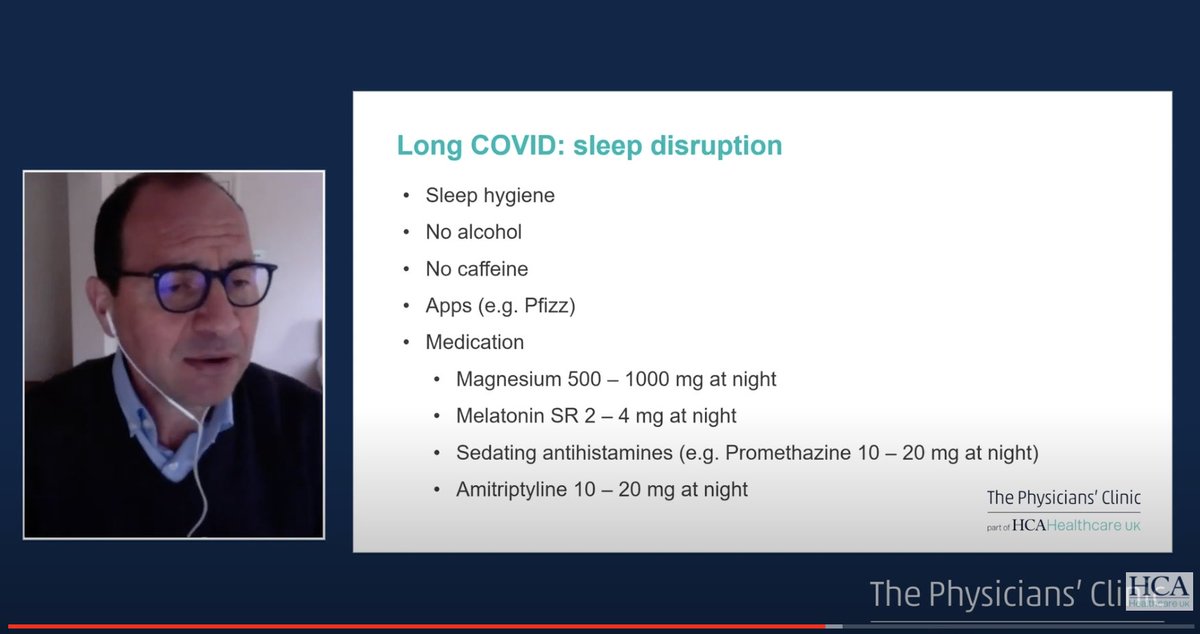
20. Addressing sleep is crucial (I also agree with this - take meds until you can sleep on your own again.) "If patients do not sleep, they do not recover. (side note - this might be related to the brain's glymphatic drainage symptom, which happens most during sleep!)
#LongCovid
#LongCovid
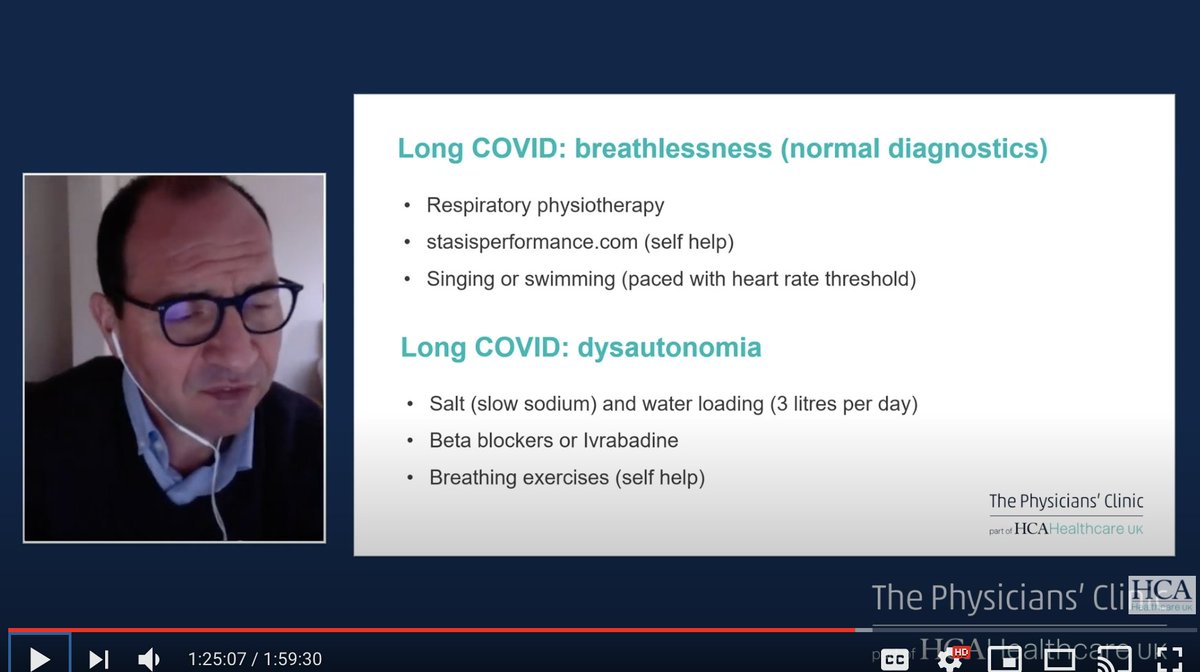
21. Specific suggestions for dysfunctional breathing and dysautonomia. "Dysautonomia (esp POTS) is a common component of #LongCOVID, and it's particularly severe in younger patients." 
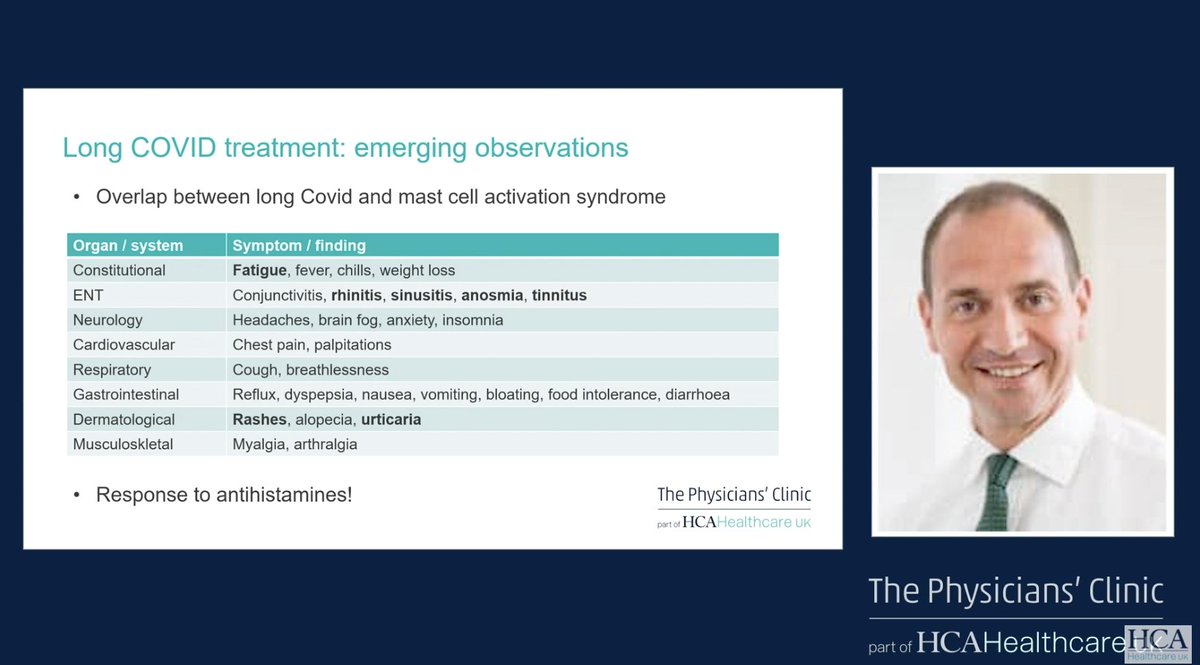
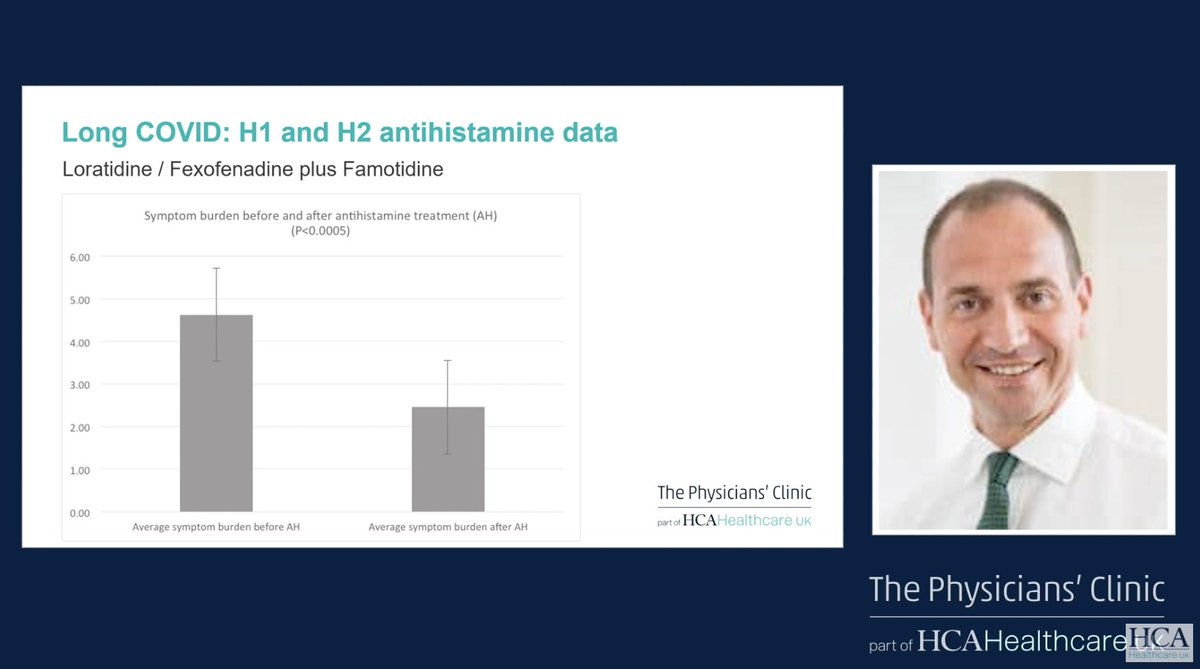
23. Here's a chart on Loratidine/Feofenadine plus Famotidine (Pepcid). (I've written about it elsewhere, but Pepcid has also been shown to alleviate even some breathing and neurological symptoms).
These are safe, well-tolerated treatments.
These are safe, well-tolerated treatments.
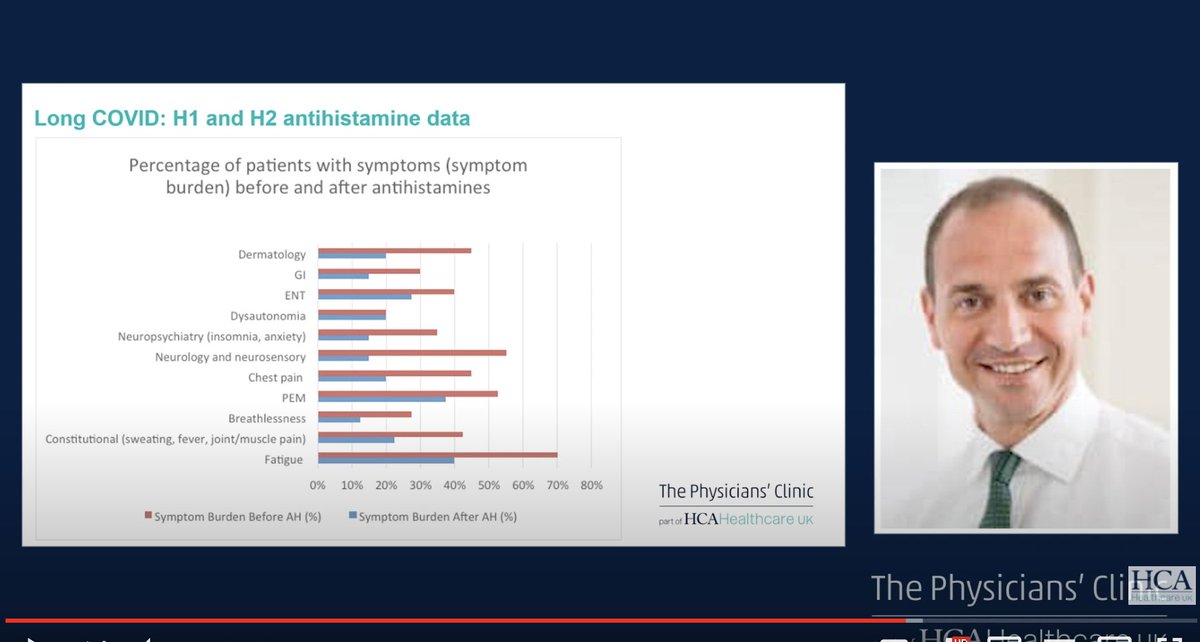
24: A chart showing a wide range of symptoms, including neurological and respiratory symptoms, responding to anti-histamine treatments:
(side note - some patients with SIBO, dysbiosis, or other GI issues should be careful/take good probiotics alongside this). #LongCOVID
(side note - some patients with SIBO, dysbiosis, or other GI issues should be careful/take good probiotics alongside this). #LongCOVID
25. He reports that patients see an improvement between 1-12 weeks after starting this regiment. This implies the pathophysiology is more complicated than just histamine, because histamine responses are over the course of hours, not weeks. #LongCOVID
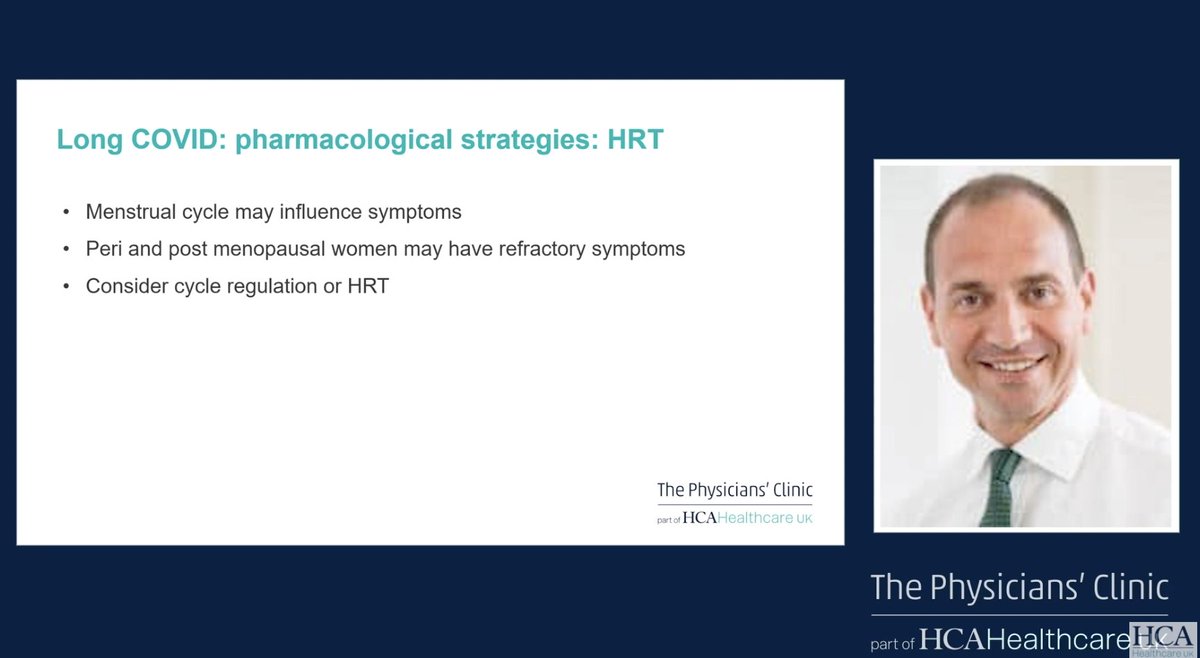
26. About 70% of people who menstruate have worsening symptoms leading up to menstruation #LongCovid
Cycle regulation drugs or HRT can alleviate symptoms:
Cycle regulation drugs or HRT can alleviate symptoms:
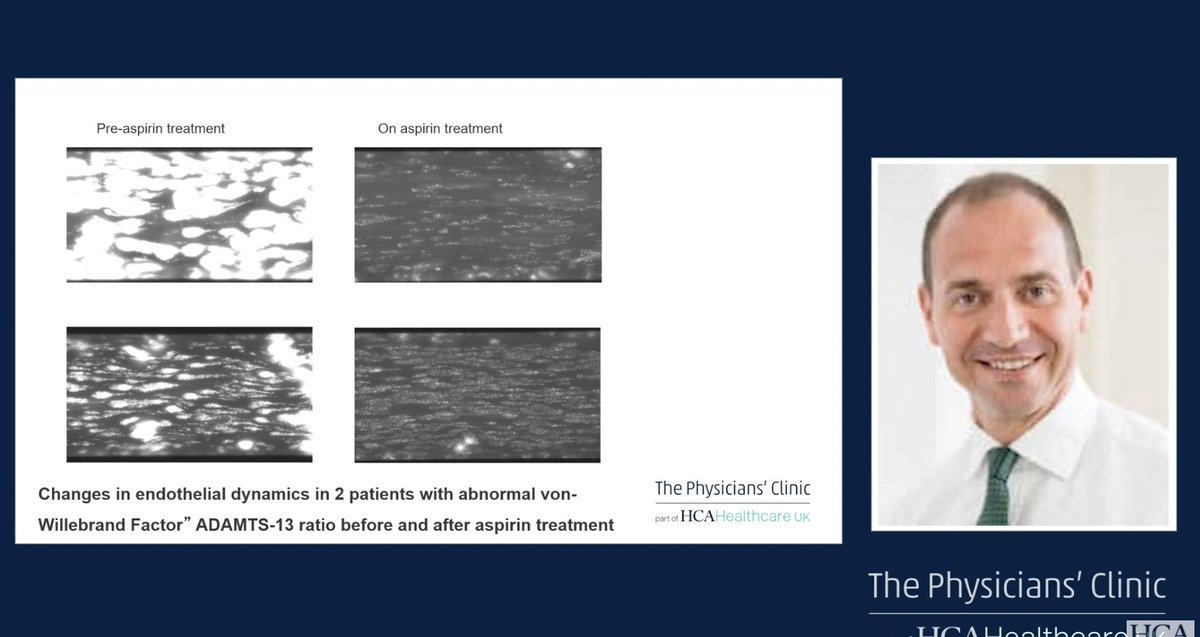
27. "Microvascular clotting is a feature of #LongCOVID."
Patients have headaches, poor exercise tolerance, extreme lethargy. Elevated VWF in many of these patients.
Patients have headaches, poor exercise tolerance, extreme lethargy. Elevated VWF in many of these patients.
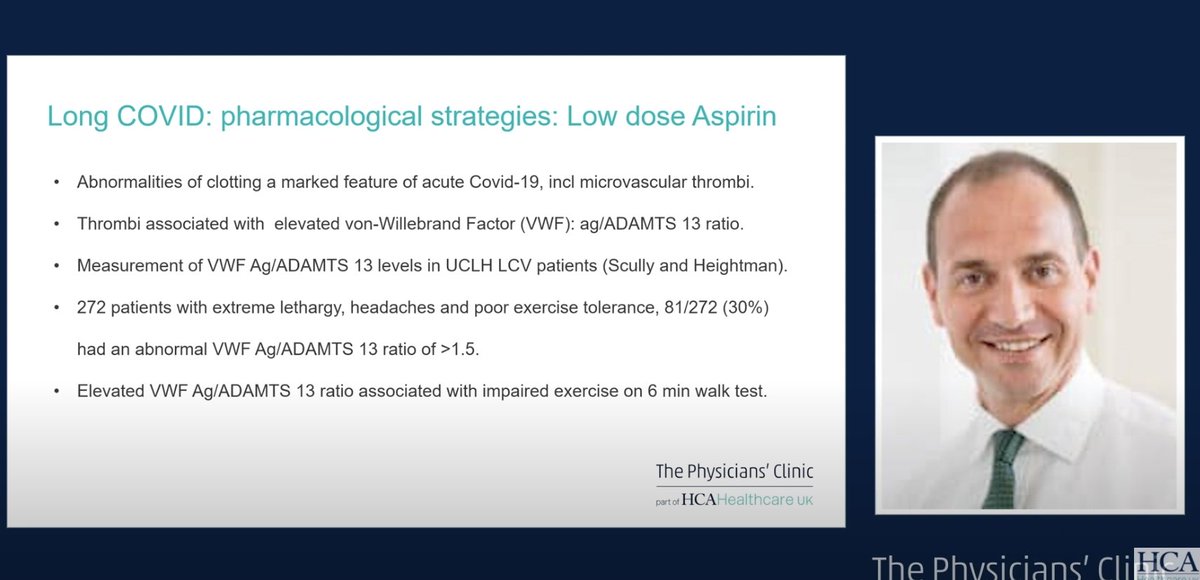
28. He did a test which essentially subjected their blood to shear stress. 29% clotted within 5 minutes 🤯
Low dose aspirin significantly reduces this. #LongCOVID
Low dose aspirin significantly reduces this. #LongCOVID
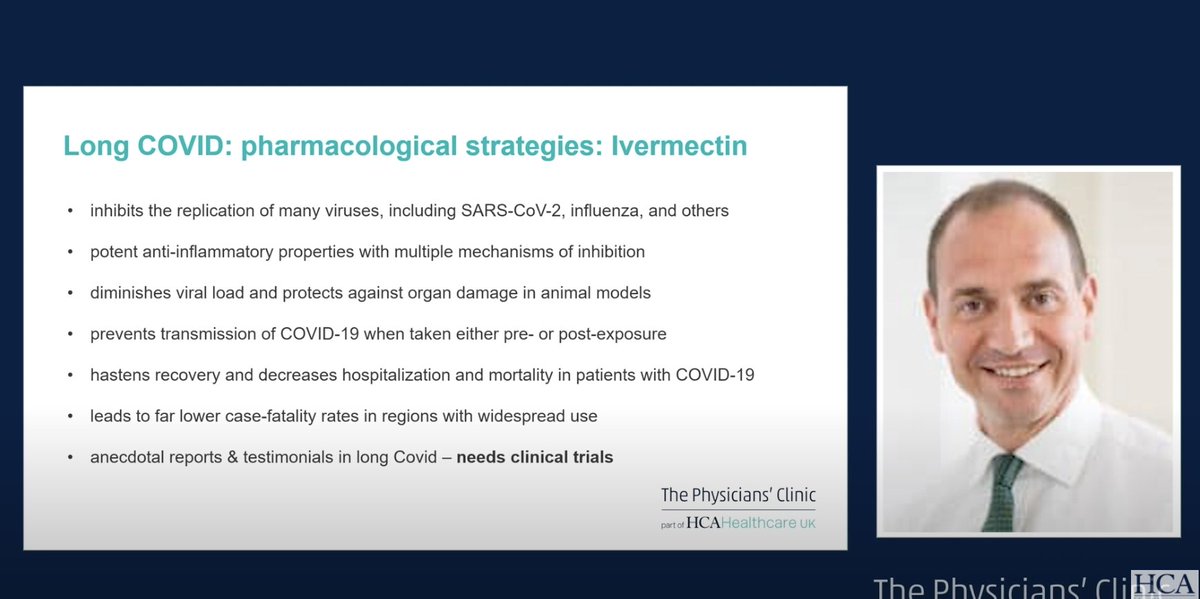
29. Jury is out on ivermectin, but it might work, should be considered in a clinical trial. Main problem is that major regulators have stated ivermectin should not be used outside of clinical trials. #LongCOVID 
30. On vaccines - "we've all heard anecdotes that #LongCOVID patients get better after vaccination - my experience is that those patients are few and far between. In fact, most patients seem to get worse after the vaccine - usually transiently so, but sometimes not."
31.
3 anecdotal treatments that might help #LongCOVID in some cases:
1. Fluvoxamine
2. Statins
3. Anti-coagulants
3 anecdotal treatments that might help #LongCOVID in some cases:
1. Fluvoxamine
2. Statins
3. Anti-coagulants
Next up is a 20 min Q&A
32.
Q: When patients prevent with migraine headaches, what imaging is more helpful, CT or MRI?
A: MRI, if possible, though we don't know mechanisms of the brain disease, but MRI may show more subtleties. #LongCOVID
32.
Q: When patients prevent with migraine headaches, what imaging is more helpful, CT or MRI?
A: MRI, if possible, though we don't know mechanisms of the brain disease, but MRI may show more subtleties. #LongCOVID
33.
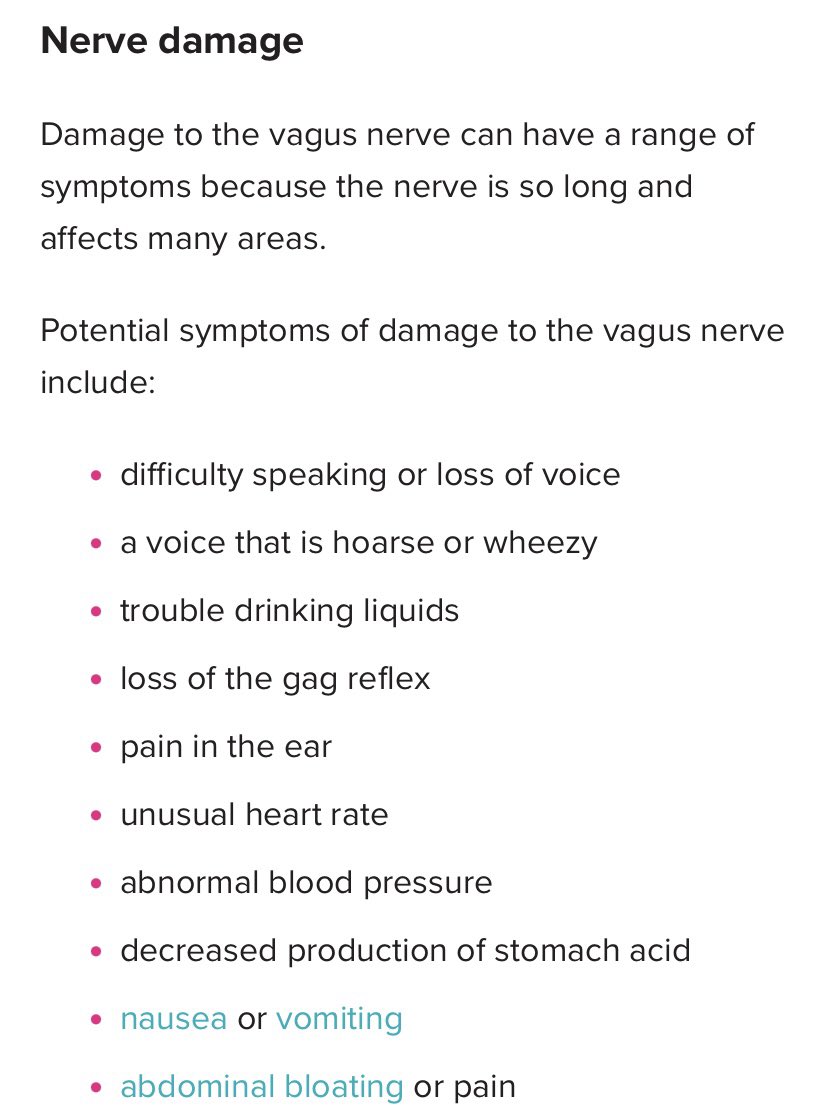
Q: Could there be a post-viral imbalance between the sympathetic and parasympthetic nervous system and perturbed hypothalamic pituitary axis?
A: Yes, we're hearing about vagal nerve disturbance, esp tachycardias, the POTS
Q: Could there be a post-viral imbalance between the sympathetic and parasympthetic nervous system and perturbed hypothalamic pituitary axis?
A: Yes, we're hearing about vagal nerve disturbance, esp tachycardias, the POTS
34.
A continued: Some autopsy studies have showed virus in the brainstem (cc @microbeminded2). So I think the answer is yes, there is some data supporting that.
Different doctor: this is akin to a vagal neuropathy with sympathetic hyperactivity
(
A continued: Some autopsy studies have showed virus in the brainstem (cc @microbeminded2). So I think the answer is yes, there is some data supporting that.
Different doctor: this is akin to a vagal neuropathy with sympathetic hyperactivity
(
https://twitter.com/ahandvanish/status/1391488899365670912)
35. continued: causing POTS, sleep dysfunction. Blocking sympathetic responses can help.
⭐️Important: the one symptom that was *not affected* by antihistamine treatment is dysautonomia.⭐️ #LongCOVID
"There was absolutely no effect in any patient on dysautonomia symptoms."
⭐️Important: the one symptom that was *not affected* by antihistamine treatment is dysautonomia.⭐️ #LongCOVID
"There was absolutely no effect in any patient on dysautonomia symptoms."
36. Q: what doses of H1 and H2 antihistamines are used? #LongCOVID
A: "I start patients with over the counter loratadine, 10mg 2x daily, in combination with famotidine, 40mg, at night. I assess patients every 2 weeks - if they don't respond, I change Loratidine to Fexofenadine +
A: "I start patients with over the counter loratadine, 10mg 2x daily, in combination with famotidine, 40mg, at night. I assess patients every 2 weeks - if they don't respond, I change Loratidine to Fexofenadine +
37 cont'd: sometimes increase dose of famotidine for a period of time. In patients who respond and then stagnate, I consider the introduction of ketotifen at night, which is sedating (good for sleep dysfunction patients) and is also considered a mast cell stabilizer." #LongCOVID
38: cont'd "In some patients with mild gut symptoms, can consider sodium cromoglicate; in patients with airway symptoms you can consider montelukast." #LongCOVID
39. Q: Does oxygen desaturation on exercise help distinguish between cardiac & respiratory causes?
A: Yes, bc cardiac causes of breathlessness *do not* lead to oxygen desaturation, implies respiratory causes. He does recommend a physiological stress echo if no resp issues found.
A: Yes, bc cardiac causes of breathlessness *do not* lead to oxygen desaturation, implies respiratory causes. He does recommend a physiological stress echo if no resp issues found.
40. The above answer got cut off so may want to listen, around 1:49:00.
41. Q: Cardiac MRIs are often not available; what other options?
A: Pericarditis can sometimes be diagnosed with ECG or echo, but these tests are often normal, it requires specialist review as well. Natriuretic peptide tests help, are usually but not always elevated. #LongCOVID
A: Pericarditis can sometimes be diagnosed with ECG or echo, but these tests are often normal, it requires specialist review as well. Natriuretic peptide tests help, are usually but not always elevated. #LongCOVID
42.
Q: Have a patient with high D-Dimer, discharged from ER, LC clinic appnt is 6 months away. What to do?
A: Hard decision, some options include risk-assessed prophylaxis, referral to thrombosis specialist
Q: Have a patient with high D-Dimer, discharged from ER, LC clinic appnt is 6 months away. What to do?
A: Hard decision, some options include risk-assessed prophylaxis, referral to thrombosis specialist
43. One more answer: there's no real risk to offer patients antihistamine regime.
44. Back to the oxygen desaturation: we see this often, patients with normal cardiac/respiratory tests but low oxygen saturation. It seems reasonable to assume microvascular disease is responsible, in which cases low dose aspirin or anticoagulation seems reasonable #LongCOVID
45. Q: What's causing adverse vaccine reactions in #LongCOVID patients?
A: Probably abnormal immune reaction. Probably *not* the antibody response to spike protein, since we would've seen this happen when people make antibodies naturally.
A: Probably abnormal immune reaction. Probably *not* the antibody response to spike protein, since we would've seen this happen when people make antibodies naturally.
46. That concludes the webinar! Hope this was helpful for the #LongCOVID community. ❤️
For #17, I meant to say "should not" get treated with CBT - it requires a different type of treatment.
• • •
Missing some Tweet in this thread? You can try to
force a refresh