This was an MI of the RV + inferior LV, with complete heart block, caused by a thrombotic occlusion of the proximal RCA.
Thanks all for commenting. 🧵 below has some basic stuff + nerdy stuff, hopefully something helpful for everyone.
1/
Thanks all for commenting. 🧵 below has some basic stuff + nerdy stuff, hopefully something helpful for everyone.
1/
https://twitter.com/sargsyanz/status/1394646332116189185
Most people quickly noticed the marked ST elevations and jumbo T-waves in the inferior leads. Some inferior STEMIs can be very subtle. This one isn’t.
You're right to want to page the interventional cardiologist the minute you see this.
2/
You're right to want to page the interventional cardiologist the minute you see this.
2/
But several folks also pointed out that this ECG exemplifies the importance of a systematic approach.
My system is Rhythm-QI-ACS.
Rhythm and rate
QRS
Intervals
Axis
Chambers
ST/TW/Q aka ischemia
3/
My system is Rhythm-QI-ACS.
Rhythm and rate
QRS
Intervals
Axis
Chambers
ST/TW/Q aka ischemia
3/
https://twitter.com/sargsyanz/status/1219116142213718016?s=20
The rate is 50s, but the rhythm is complete heart block. Sinus-looking P-waves (+ in II) march out at a rate of ~150 (quite the hypersympathetic state), but have no relation with the QRSs. It may look like some precede the QRS, but others are buried in the T-waves, QRSs, etc.
4/
4/

This is a critical finding, because the escape rhythm may not last forever, and the bradyarrhythmia may quickly become an additional life-threatening problem you may need to manage before (and less likely after) reperfusion.
5/
5/
Moving on. The QRSs are variable. Beats 1 & 6 are narrow (proximal His bundle escape beats), but others' morphology is LBBB or incomplete RBBB / delayed RV. This is important, because ischemic changes are best assessed with normal depolarization (narrow QRSs).
6/
6/

The axis is normal. QT is normal. Chambers - there may be LVH based on precordial voltage in non-LBBB pattern beats. Meh.
Finally, let’s take a closer look at those ischemic changes that jumped out…
7/
Finally, let’s take a closer look at those ischemic changes that jumped out…
7/
We'll avoid complexes #2 and 3, since LBBB distorts things (but doesn't hide STEMI here).
Based on the other complexes, we see an inferior MI:
~5mm STE in III and F
~2mm STE in II
The STD in I, L, V4-V6 are likely of this injury current (reciprocal changes).
V1-V3 later.
8/
Based on the other complexes, we see an inferior MI:
~5mm STE in III and F
~2mm STE in II
The STD in I, L, V4-V6 are likely of this injury current (reciprocal changes).
V1-V3 later.
8/

The inferior LV wall is usually fed by the PDA.
The PDA usually comes off the RCA, less commonly LCx.
As such, the most clinically relevant question with IMI is whether it’s caused by a PROXIMAL RCA lesion.
9/
The PDA usually comes off the RCA, less commonly LCx.
As such, the most clinically relevant question with IMI is whether it’s caused by a PROXIMAL RCA lesion.
9/

If the occlusion is in the RCA proximal to the acute marginal branch, then the RV is involved meaning different prognosis and considerations in management (e.g. not dropping preload).
There could be hints of this on exam. But how do you mediate this suspicion on ECG?
10/
There could be hints of this on exam. But how do you mediate this suspicion on ECG?
10/
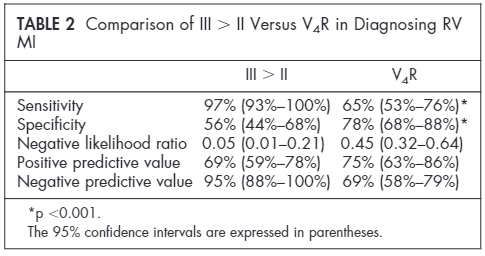
The quickest screen is to look at the relative magnitude of STE in lead III vs. II.
STE in III > II is a sensitive finding for RVMI (see table from PMID 11179532).
If present, PPV is high enough (and sensitivity of STE in V4R low enough), that you can act on it.
11/
STE in III > II is a sensitive finding for RVMI (see table from PMID 11179532).
If present, PPV is high enough (and sensitivity of STE in V4R low enough), that you can act on it.
11/
BTW, mechanistically, this makes sense – an additional injury current involving the RV will contribute to more STE In III (a right-and-downward pointing lead) than II (a left-and-downward pointing lead).
12/
12/
Finally, let’s talk about V1-V2. In most IMIs, V1-V2 have ST depressions, reciprocal to the inferoposterior STE.
But V1-V2, esp V1, also overlie the RV - the anterior ventricle.
V1 STE > 0.5mm in setting of IMI is predictive of RV involvement.
13/
pubmed.ncbi.nlm.nih.gov/30497759/
But V1-V2, esp V1, also overlie the RV - the anterior ventricle.
V1 STE > 0.5mm in setting of IMI is predictive of RV involvement.
13/
pubmed.ncbi.nlm.nih.gov/30497759/

One nerdy thing:
The above study by @SmithECGBlog and co also found that the sensitivity of STE in V1 for RVMI was only 35% if there WAS STD in V2, but higher at 69% if there was NO STD in V2.
14/
The above study by @SmithECGBlog and co also found that the sensitivity of STE in V1 for RVMI was only 35% if there WAS STD in V2, but higher at 69% if there was NO STD in V2.
14/
Basically, the injury currents from the inferior LV and the RV are competing in V1/V2, and can cancel each other out.
If there’s less inferioposterior wall current, it allows the RV injury current to be seen better.
15/
If there’s less inferioposterior wall current, it allows the RV injury current to be seen better.
15/
Another nerdy thing:
I think V2 and V3 may have been reversed in this ECG based on the QRS and ST segment progression/continuity.
16/
I think V2 and V3 may have been reversed in this ECG based on the QRS and ST segment progression/continuity.
16/
Take-home points:
- Always be systematic even if an overt abnormality jumps out at you
- In IMI, STE in III > II is a sensitive screen for RVMI
- Its PPV is enough too, but STE in V1 or STE in V4R are even more specific
- If RVMI, don't drop preload, watch for brady rhythms
- Always be systematic even if an overt abnormality jumps out at you
- In IMI, STE in III > II is a sensitive screen for RVMI
- Its PPV is enough too, but STE in V1 or STE in V4R are even more specific
- If RVMI, don't drop preload, watch for brady rhythms
Please share more pearls or corrections!
And sorry for delay @JHahnMD @DrJayPatel @jackkur59171979 @ShitalOli @muzamil_amin @elwakeel11 @saahilaj @DrAmjadNazeer @Hamdisinsight @vijaybramhan @JHourmozdi @ED_Ultrasounder @WKayaniMD @redswarm90 @RosenelliEM
And sorry for delay @JHahnMD @DrJayPatel @jackkur59171979 @ShitalOli @muzamil_amin @elwakeel11 @saahilaj @DrAmjadNazeer @Hamdisinsight @vijaybramhan @JHourmozdi @ED_Ultrasounder @WKayaniMD @redswarm90 @RosenelliEM
• • •
Missing some Tweet in this thread? You can try to
force a refresh