1/How can #POCUS #echofirst help in the evaluation of #hyponatremia?
#Nephrology consulted for low sodium. Pt received diuretic for shortness of breath (which was possibly due to hiatal hernia as shown on CXR).
2 physicians FELT patient was EUVOLEMIC
Small 🧵below 👇 #MedEd
#Nephrology consulted for low sodium. Pt received diuretic for shortness of breath (which was possibly due to hiatal hernia as shown on CXR).
2 physicians FELT patient was EUVOLEMIC
Small 🧵below 👇 #MedEd

2/Based on the above labs, it does look like euvolemic hyponatremia (Urine Na is high, Uosm >100 but not too high, BUN not high). BP was 150s systolic.
That's it? Give some salt tablets or UreNa etc.?
No; perform PHYSICAL EXAM (= #POCUS)
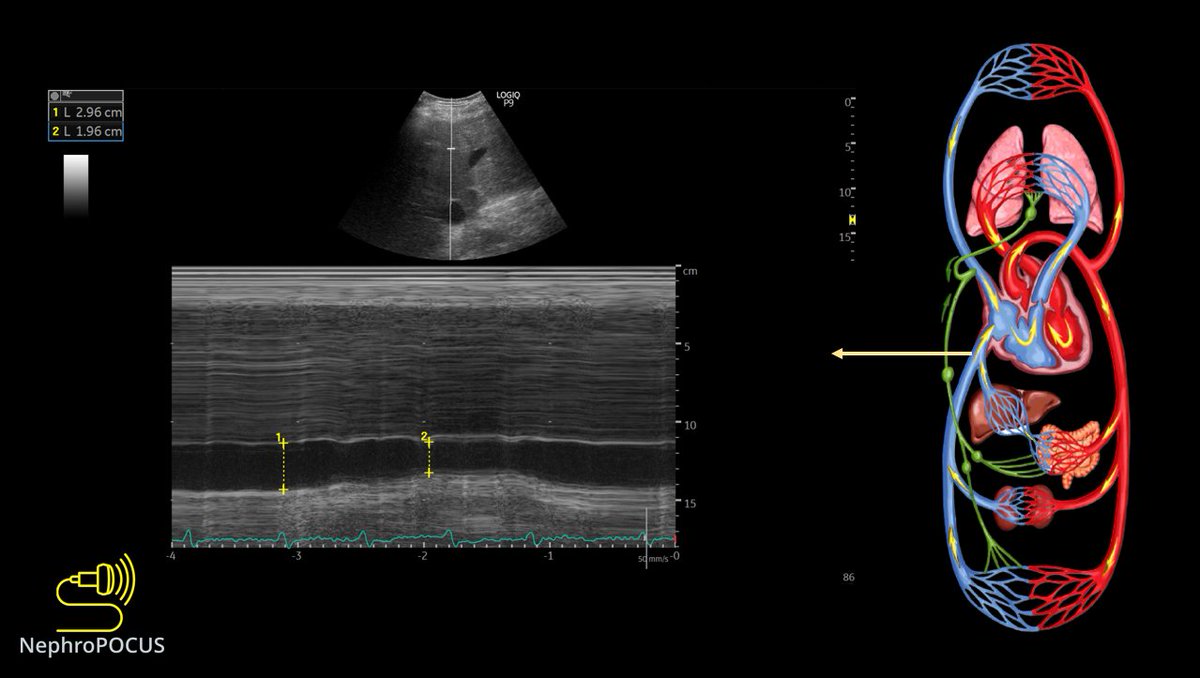
IVC was small - doesn't tell much 😬
That's it? Give some salt tablets or UreNa etc.?
No; perform PHYSICAL EXAM (= #POCUS)
IVC was small - doesn't tell much 😬
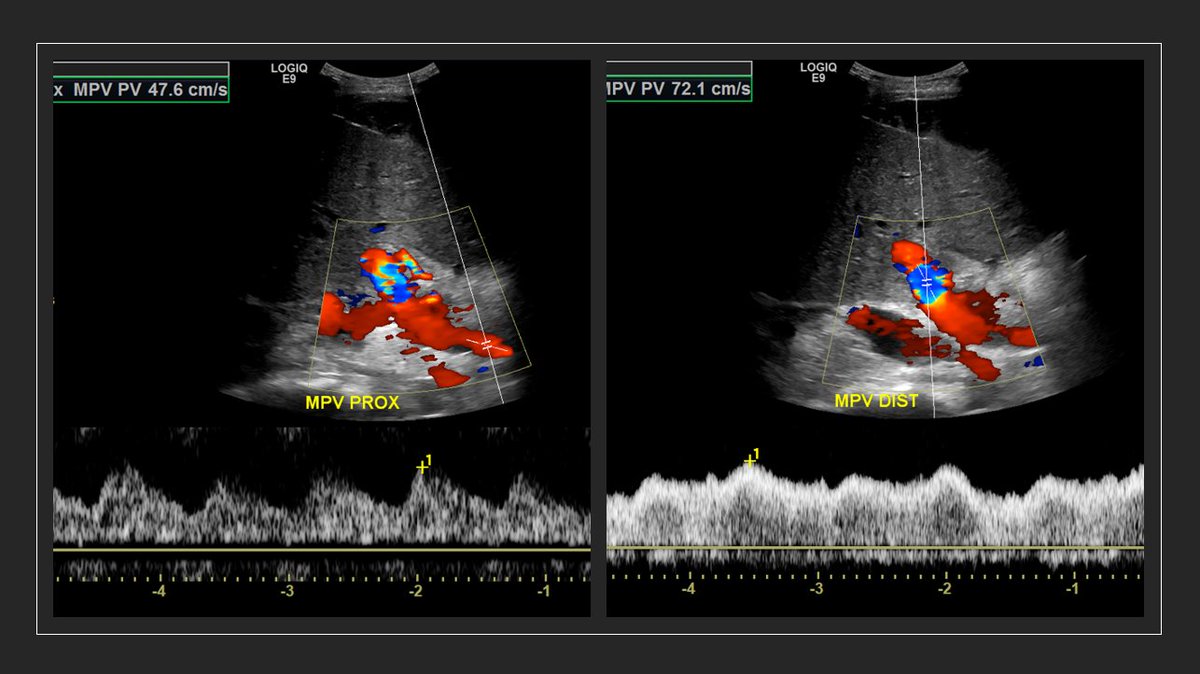
3/ Next step? Look at the heart, assess stoke volume.
Recent echo LVEF>50%
LV contraction looks good visually
We measured LVOT VTI (couldn't measure LVOT diameter due to chest deformity precluding good PLAX view but its not a problem; VTI is generally enough)
#POCUS
Recent echo LVEF>50%
LV contraction looks good visually
We measured LVOT VTI (couldn't measure LVOT diameter due to chest deformity precluding good PLAX view but its not a problem; VTI is generally enough)
#POCUS

4/ #POCUS 👆 shows low VTI unexpected for normal EF.
BP is fine but flow changes precede ⬇️ in BP. Cannot rely.
Patient is likely hypovolemic. Lets recommend fluids but after making sure pt is fluid responsive. So, performed passive leg raise. 👇
BP is fine but flow changes precede ⬇️ in BP. Cannot rely.
Patient is likely hypovolemic. Lets recommend fluids but after making sure pt is fluid responsive. So, performed passive leg raise. 👇
5/ Repeat VTI improved by >15% without significant change in HR. That means the patient is volume responsive.
I took average of at least 3 readings to account for error.
#POCUS #echofirst
I took average of at least 3 readings to account for error.
#POCUS #echofirst

6/ Next step: Recommended Normal Saline administration. Na improved to 130 in 2 days. True euvolemic hypoNa would not have improved as U osm was less than that of saline.
Repeat #POCUS performed - If VTI improves, it proves our diagnosis. Here it is 👇
Repeat #POCUS performed - If VTI improves, it proves our diagnosis. Here it is 👇

7/ Average VTI ~21 (I performed 6 readings to be sure) - Normalized!
The diagnosis of hypovolemic hyponatremia is accurate!!
There could be underlying chronic hypoNa, poor protein intake etc. but that's not the primary driving force here.
The diagnosis of hypovolemic hyponatremia is accurate!!
There could be underlying chronic hypoNa, poor protein intake etc. but that's not the primary driving force here.
8/ Take home points:
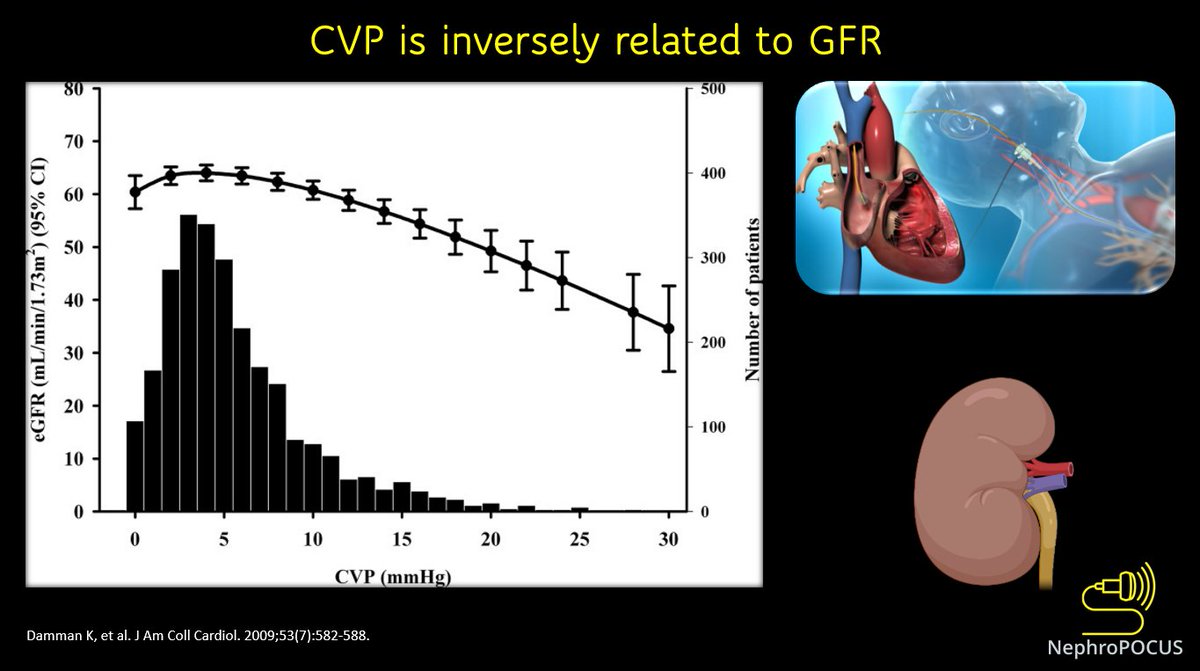
1/ Appropriate management of #hyponatremia depends on accurate assessment of volume status
2/ Conventional exam is not always reliable for fluid assessment
3/ Don't trust anybody's FEELINGS about volume. Examine (#POCUS) the patient.
1/ Appropriate management of #hyponatremia depends on accurate assessment of volume status
2/ Conventional exam is not always reliable for fluid assessment
3/ Don't trust anybody's FEELINGS about volume. Examine (#POCUS) the patient.
9/ A slideshow of my old lecture on hyponatremia. May help if read at low speed (0.5 or 0.25x) #Nephrology #MedEd
Cc hemodynamic friends @khaycock2 @ArgaizR @ThinkingCC @KalagaraHari @khaledsidiya @RJonesSonoEM @Thind888 et al. for further discussion.
• • •
Missing some Tweet in this thread? You can try to
force a refresh