This is very true. The best way to do research for #LongCOVID is to learn from people who have been working in post-viral illness for literal decades.
Here is a list of these researchers to get you started:
docs.google.com/document/d/17q… 1/
Here is a list of these researchers to get you started:
docs.google.com/document/d/17q… 1/
https://twitter.com/Sabrina_Poirier/status/1399760859161825280
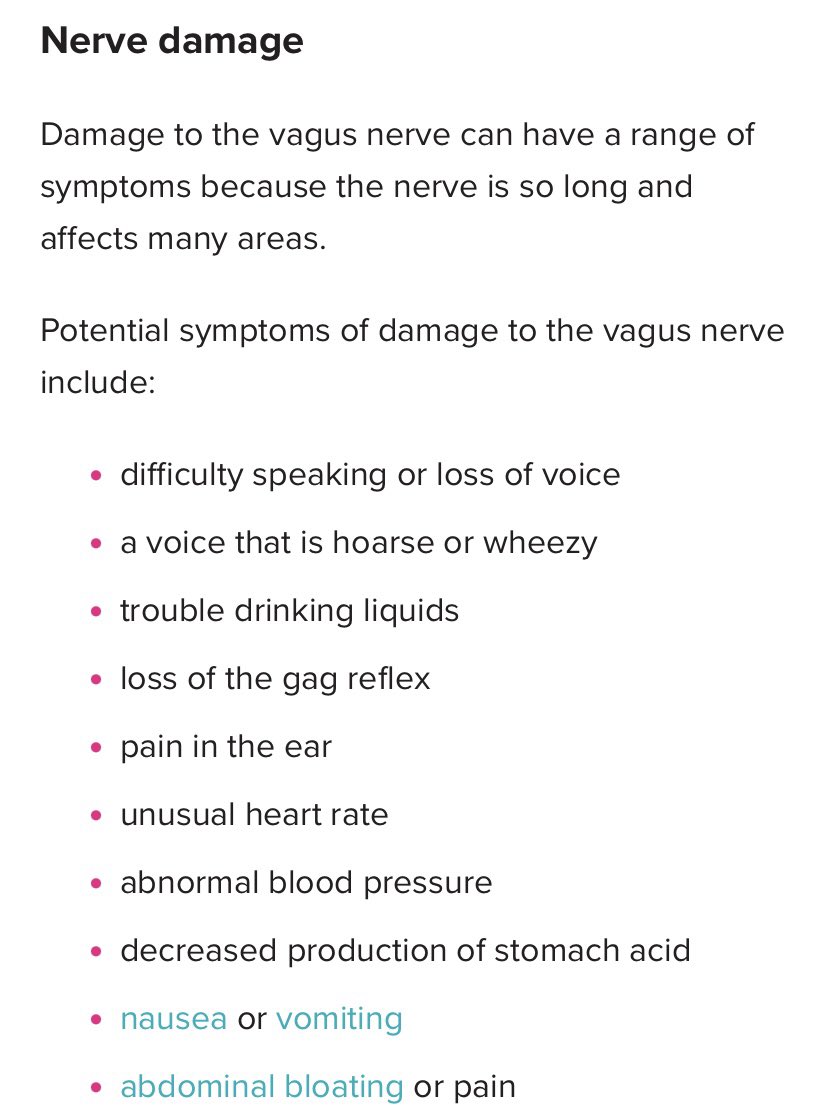
These areas of research are less known, including metabolic profiling, antiviral response phenotypes, neuroimmunology, cerebral blood flow, mitochondrial fragmentation, viral persistence, hypermobility, craniocervical issues, altered T&B cells, metabolomics & proteomics, etc. 2/
These researchers have made astounding post-viral findings in the above areas. Everyone interested in #LongCOVID should stop treating this as an illness unlike any other and instead dive into the massive amount of research that has already been done. 3/
And #pwME and others who have been suffering with post-viral illness for literal decades are owned the same care, as well as justice for decades of truly horrific mistreatment. 4/
• • •
Missing some Tweet in this thread? You can try to
force a refresh