
When a new drug is approved in your field, it is a good practice to go through the prescribing information in detail. There is a *lot* to unpack in the #Ozanimod PI. Let's take a tour (THREAD) 

First, *before prescribing*, there are 7 required assessments in section 2.1.
1⃣ recent CBC with lymphocyte count
2⃣ recent LFTs
3⃣ EKG to rule out long QT, heart block, sick sinus
4⃣ Eye exam if prior uveitis, macular edema
5⃣ Washout of prior immunosuppressive drugs...
1⃣ recent CBC with lymphocyte count
2⃣ recent LFTs
3⃣ EKG to rule out long QT, heart block, sick sinus
4⃣ Eye exam if prior uveitis, macular edema
5⃣ Washout of prior immunosuppressive drugs...

6⃣ Washout of drugs that slow heart rate and/or AV conduction
7⃣ Test patients for antibodies to VZV - vaccinate if negative *before* starting drug
7⃣ Test patients for antibodies to VZV - vaccinate if negative *before* starting drug

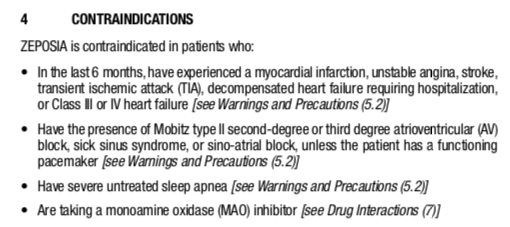
#Ozanimod is contraindicated in people who
- have had MI, unstable angina, stroke, TIA, hospitalization for CHF, class 3-4 CHF
- Mobitz T2 or 3rd deg AV block, sick sinus, or sinoatrial block (unless pacemaker in place)
- have severe untreated sleep apnea (screen)
- on MAO-I
- have had MI, unstable angina, stroke, TIA, hospitalization for CHF, class 3-4 CHF
- Mobitz T2 or 3rd deg AV block, sick sinus, or sinoatrial block (unless pacemaker in place)
- have severe untreated sleep apnea (screen)
- on MAO-I
You have to start ozanimod as a slow titration over 7 days, and keep an eye out for symptomatic changes in heart rate or blood pressure. 

Now on to the Warnings and Precautions (5 columns in the PI).
1⃣ Infections - don't start during infection. Increased URIs, UTIs, herpes (zoster and simplex) infections. Consider stopping for serious infection. Risk can continue for 3 months after discontinuation of drug.
1⃣ Infections - don't start during infection. Increased URIs, UTIs, herpes (zoster and simplex) infections. Consider stopping for serious infection. Risk can continue for 3 months after discontinuation of drug.
- Also watch for fatal cryptococcal meningitis, disseminated crypto.
- Also watch for PML caused by JC virus
- avoid combining with any other immunosuppression (including 3m after discontinuation)
- be sure immune to VZV - confirm antibody +, complete vaccination before starting
- Also watch for PML caused by JC virus
- avoid combining with any other immunosuppression (including 3m after discontinuation)
- be sure immune to VZV - confirm antibody +, complete vaccination before starting

2⃣ Watch for Bradyarrhythmias and cardiac conduction delays
*No safety data* on people with
- CVD events in past 6m
- class 3-4 CHF
- QT >450M/>470F
- severe sleep apnea
- baseline resting HR < 55
- people on drugs for arrhythmia
- people with heart block
*No safety data* on people with
- CVD events in past 6m
- class 3-4 CHF
- QT >450M/>470F
- severe sleep apnea
- baseline resting HR < 55
- people on drugs for arrhythmia
- people with heart block

3⃣ Liver injury - get baseline LFTs, repeat any time unexplained N/V, abd pain, fatigue, anorexia, jaundice, or dark urine occur. That is a lot of LFT checks unless UC patients are doing very well. 



4⃣ Birth Control - effective birth control for fertile women during therapy and for 3 months after discontinuation (slow elimination). This will make #OZ unattractive for a lot of young women. 

5⃣ Blood pressure elevation monitoring - monitored during treatment and managed. How often?? Not specified. 

6⃣ Avoid tyramine-containing foods. These can cause severe hypertension when on #OZ
- aged cheeses
- cured or processed meats (sausage)
- pickled or fermented vegetables (sauerkraut, kimchi, tofu, miso, soy sauce)
- citrus and tropical fruits
- fermented alcohol - beer, wine
- aged cheeses
- cured or processed meats (sausage)
- pickled or fermented vegetables (sauerkraut, kimchi, tofu, miso, soy sauce)
- citrus and tropical fruits
- fermented alcohol - beer, wine

8⃣ Macular edema - a full eye exam is recommended any time there is a change in vision. People with prior uveitis or diabetes are at increased risk.
Regular follow-up full eye exams required for patients with prior uveitis or DM. How regular? q6m? Not specified.
Regular follow-up full eye exams required for patients with prior uveitis or DM. How regular? q6m? Not specified.

9⃣ PRES - Posterior Reversible Encephalopathy Syndrome - get MRI and full neuro exam for any unexpected neurological or psychological symptoms or signs. Have to explain how this is different from PML. 

🔟 Unintended additive immune suppression - avoid starting #OZ while other IS drugs in system, avoid starting new drugs for 3m after stopping #OZ.
And watch for *rebound* autoimmune flares after stopping #OZ - a known but rare occurrence in MS.
And watch for *rebound* autoimmune flares after stopping #OZ - a known but rare occurrence in MS.

- Also watch out for drug interactions with CYP2C8 drugs like rifampin, gemfibrozil, clopidogrel, mometasone, salmeterol, candesartan, phenyoin, phenobarbital.
- Avoid MAO-I drugs
- Avoid combo of beta blocker and CCB
- Avoid MAO-I drugs
- Avoid combo of beta blocker and CCB
Avoid drugs that increase norepinephrine or serotonin, including
- opioids
- SSRIs
- SNRIs
- TCAs
(good thing no one with UC takes those 😉)
- opioids
- SSRIs
- SNRIs
- TCAs
(good thing no one with UC takes those 😉)

In summary, there is a whole lot to know about before using #ozanimod. I am hoping the manufacturer will provide pre-start checklists and monitoring checklists.
You can find the full prescribing information here:
packageinserts.bms.com/pi/pi_zeposia.…
You can find the full prescribing information here:
packageinserts.bms.com/pi/pi_zeposia.…
And a list of foods and drugs to avoid for *patients*. Because *some* UC patients do actually eat sausages, tofu, soy sauce, or kimchi, and drink
beer and/or wine
🍺🍷
And drug interactions happen if you don't know about them.
beer and/or wine
🍺🍷
And drug interactions happen if you don't know about them.
• • •
Missing some Tweet in this thread? You can try to
force a refresh











