1/ Welcome back to #TweetorialTuesday with the #MedEdTwagTeam!
Today we will be summarizing what we have learned throughout the #EffectiveQuestions series.
Thanks for joining us, #MedTwitter, #MedEd, #Tweetatrician, & #MedStudentTwitter Friends!
Today we will be summarizing what we have learned throughout the #EffectiveQuestions series.
Thanks for joining us, #MedTwitter, #MedEd, #Tweetatrician, & #MedStudentTwitter Friends!

2/ I have had an excellent time sharing with you all my approach to #EffectiveQuestions in the clinical setting.
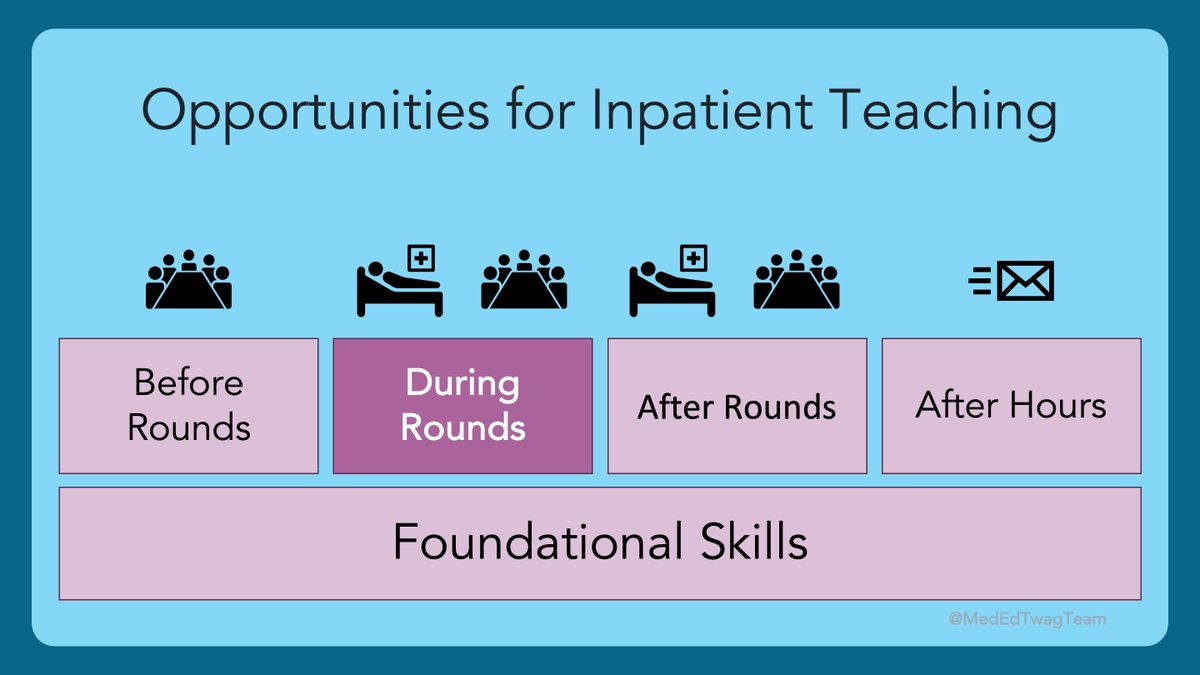
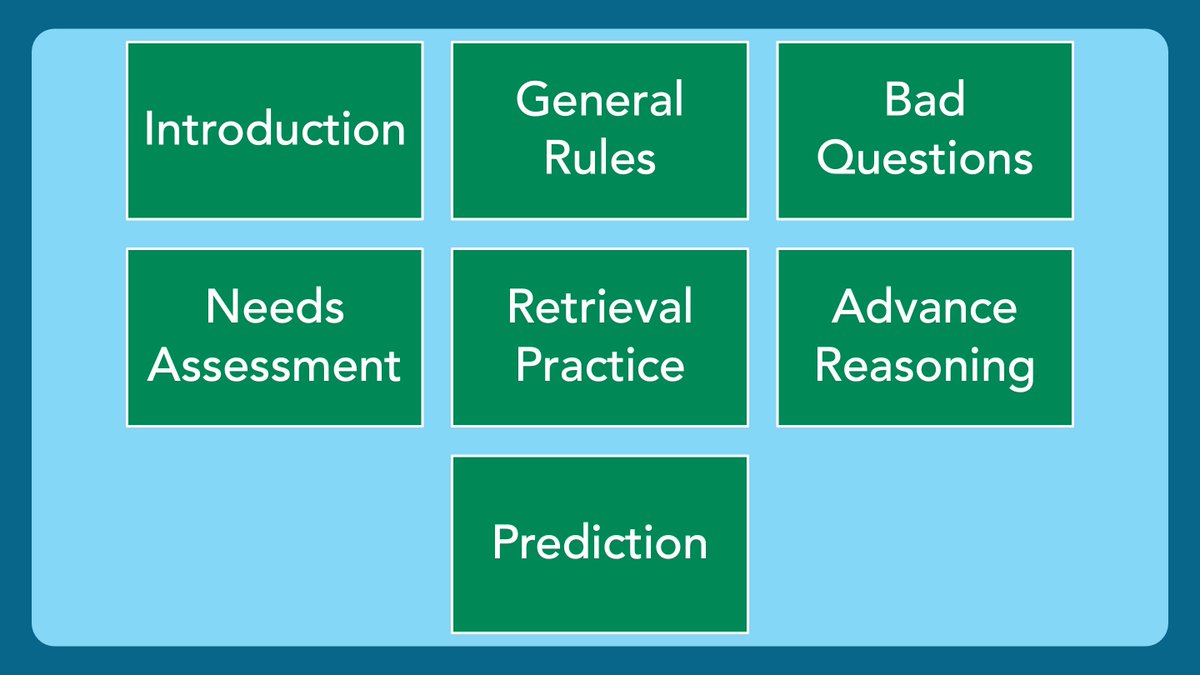
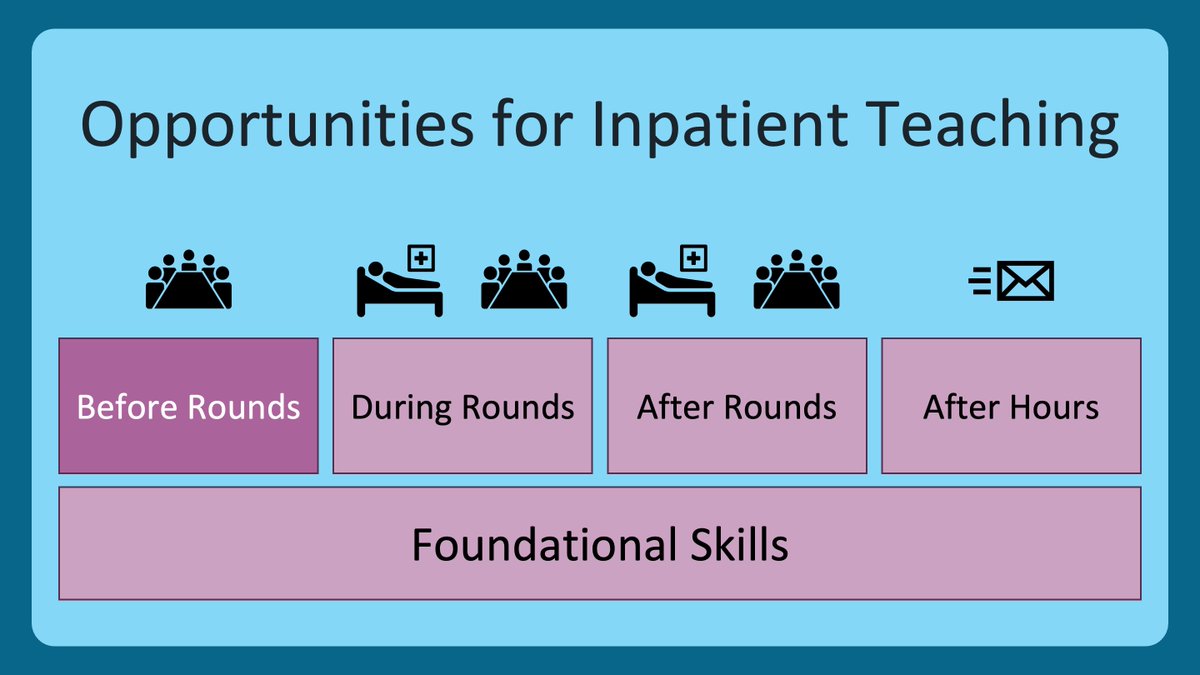
Here is where we have been during this journey.
Here is where we have been during this journey.

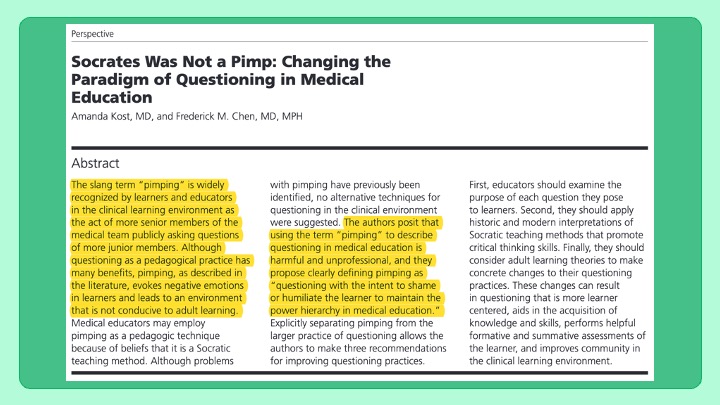
3/ In the intro we talked about ”pimping” and the psychologically dangerous environment it creates, as illustrated by these drawings in this fascinating study:
pubmed.ncbi.nlm.nih.gov/31084222/
pubmed.ncbi.nlm.nih.gov/31084222/

4/ In the @MedEdTwagTeam’s quest to create #PsychologicallySafety in clinical learning environments, we do not condone the practice, nor the term itself.
”Pimping” has got to go!
”Pimping” has got to go!
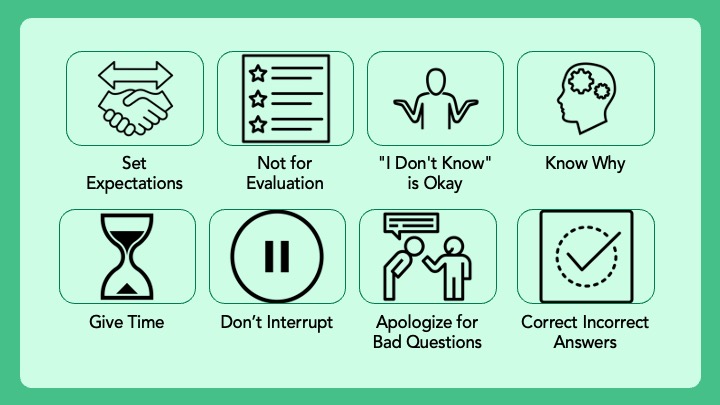
5/ Inquiry, however, is a very valuable tool to promote learning in the clinical setting when used thoughtfully.
These are the 8 general rules I follow when asking questions. Check out the whole thread for details.
These are the 8 general rules I follow when asking questions. Check out the whole thread for details.
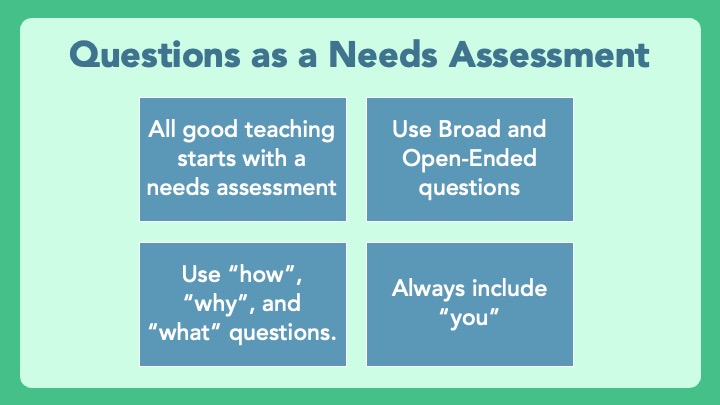
6/ We then detailed how even educators with the best of intentions can make a learning environment uncomfortable when they ask questions that are too specific. 

7/ Our first specific purpose for asking questions was to perform a needs assessment of your learner(s), i.e. finding out what they know and don’t know, so you can fill in the gaps. 
8/ We then cited the book #MakeItStick when discussing retrieval practice. Rather than asking learners to recall what they learned in their preclinical years, I ask them to recall what they learned while we worked together. This way, I know they have been exposed to the material. 

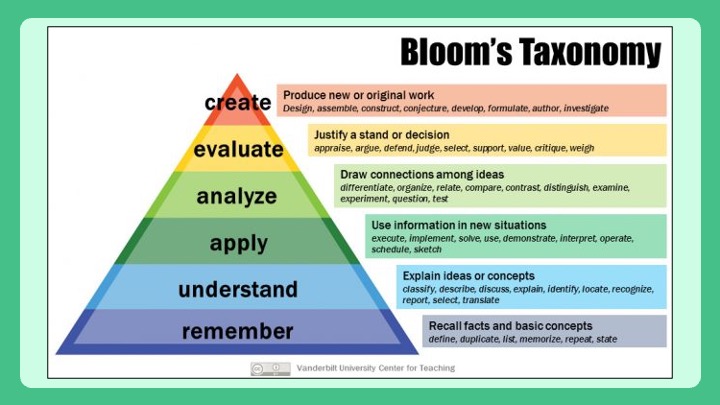
9/ Next, we talked about using #BloomsTaxonomy as a framework for thinking about advancing a learner’s reasoning. Once you feel they have a good grasp of a concept at the remember/understand level, push them into the areas of higher cognitive effort/learning. 
10/ We then overlayed the concept of Vygotsky’s Zone of Proximal Development or #ZPD. Identifying the bounds of a learner’s current abilities and supporting them in the #ZPD is key to promoting growth. 

11/ Lastly, I cited the book #SmallTeaching when discussing prediction as a fun and effective way to prepare a learner’s mind for deeper learning. There are emotional and cognitive reasons why this tool is effective. 

12/ But, prediction alone is not enough. After a prediction, it’s important to determine whether the prediction was accurate or not. Next, reflection is necessary to solidify reasoning that led to an accurate prediction, or correct thought processes that led to a misguided guess. 

13/ Thank you all so much for joining me on this journey!
Hopefully you all picked up something you can use in your practice. Feel free to share any lessons learned.
The full threads can all be found here:
twitter.com/i/events/13982…
Hopefully you all picked up something you can use in your practice. Feel free to share any lessons learned.
The full threads can all be found here:
twitter.com/i/events/13982…
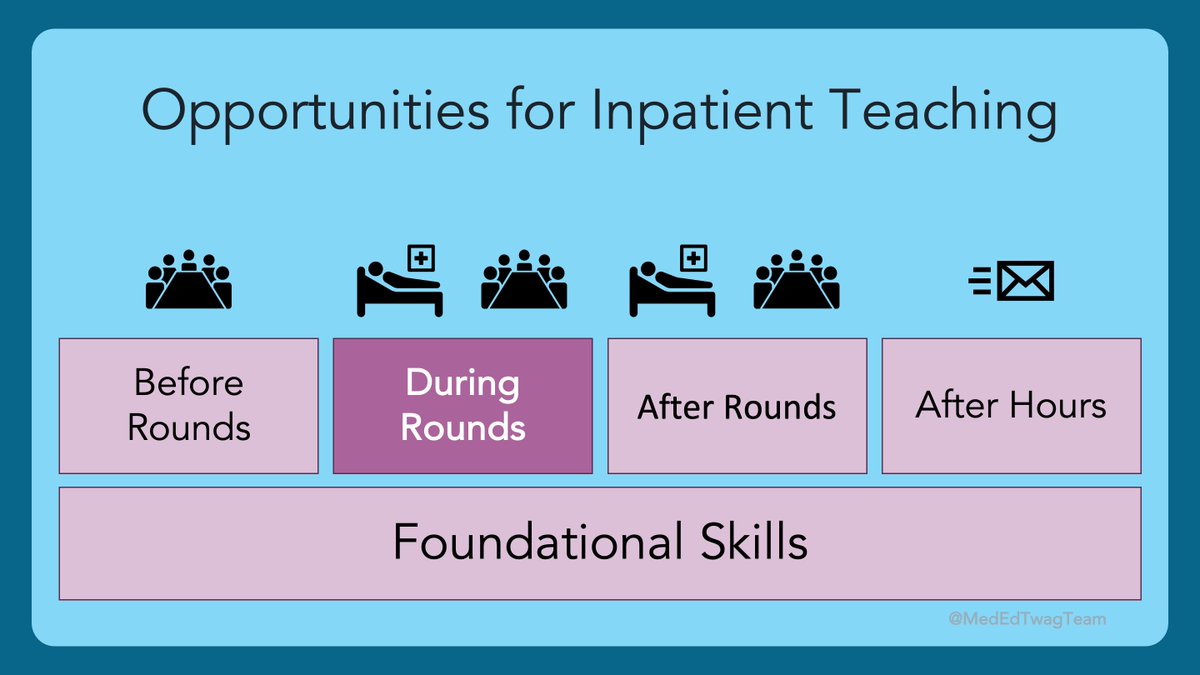
14/ Soon, @JenniferSpicer4 and I are going to introduce more advanced teaching topics. But first, we are going to return to the foundational skills of #PsychologicalSafety, as this is the time of year for foundational skills.
Gotta 🚶 before you can 🏃!
Tweet you next week!
Gotta 🚶 before you can 🏃!
Tweet you next week!

• • •
Missing some Tweet in this thread? You can try to
force a refresh