Join here tomorrow for the launch of a new accredited tweetorial on DAPT in patients with stable CAD+diabetes who have not (yet!) had an MI or stroke! Earn 0.5 CE/CME credits: physicians, nurses, pharmacists! Expert faculty @gabrielsteg. #medtwitter @academiccme #CardioTwitter
1) Welcome to a #tweetorial on #DAPT in patients with stable CAD+#diabetes who have not had an MI or stroke. Accredited for 0.5h by @academiccme: #physicians, #nurses, #pharmacists! I am @gabrielsteg . . .
. . . This educational activity is intended for healthcare providers and is supported by grants from Abbott, AstraZeneca, Bayer, Chiesi, and NovoNordisk.
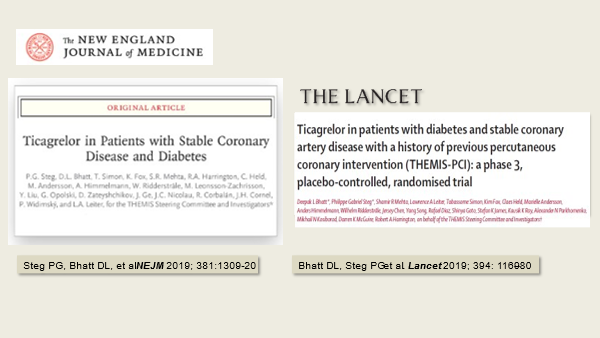
2) This is a Journal Club on The Effect of Ticagrelor on Health Outcomes in Diabetes Mellitus Patients Intervention Study (THEMIS) primary pub, found at nejm.org/doi/full/10.10…. (We also discuss elements of THEMIS-PCI (Lancet 2019 394(10204):1169-1180)). 
3) This DBRCT eval'd efficacy and safety of #DAPT with ticagrelor+ASA vs ASA alone in pts 50y/o+ who had stable #CAD and #T2D, who had not had MI or stroke. These pts are at known high risk for CV events, but whether adding ticag to ASA improves outcomes in these pts is unclear.
4) First, a poll: in which of these populations has ticagrelor+ASA been shown to provide a net clinical benefit over ASA alone?
5) It's all of the above! The relative benefit of ticagrelor in these patients has been consistent regardless of the presence of #T2D, but the benefit from the addition of ticagrelor to ASA is especially large, because diabetics are at such high CV risk
6) Part of that risk derives from increased #platelet activation in diabetics (Circulation 2011;123:798-813).
7) In addition, diabetics have accelerated platelet turnover which may contribute to a reduced antithrombotic effect of aspirin given once daily (Circ Cardiovasc Interv 2011;4:180-7) 

8) Therefore, ASA alone, the standard therapy in patients who have not yet had a primary event, may not provide fully effective antithrombotic protection.
9) Compared to patients with diabetes alone, patients having diabetes and established atherothrombosis almost doubles the risk of major adverse cardiac event (MACE) Circulation 2015;132:923–931 

10) And so in THEMIS we tested whether patients with diabetes and stable coronary artery disease without a history of prior MI or stroke derived benefit from dual antiplatelet therapy with aspirin and ticagrelor
11) THEMIS was a double-blind placebo-controlled randomized trial comparing ticagrelor vs placebo in addition to aspirin in patients with diabetes and established CAD (see Clinical Cardiology 2019;42:498- 505). The primary outcome was the composite of CV death, MI and stroke. 

12) THEMIS eventually randomized 19220 patients, median age 66, 31% female, 62% had a history of MVD, 80% a history of coronary revascularization (58% PCI, 22% CABG), mean duration of diabetes was 10 years, and >99% were on aspirin.
13) Let’s do another poll: The 3-year event rate (Kaplan-Meier estimate) in the placebo arm of the trial (receiving ASA alone) was
14) The correct answer is 7.6% at 3 years. Ticagrelor reduced the primary outcome by 10% (95% CI 0.81–0.99) P=0.038 (N Engl J Med 2019; 381:1309-1320). 

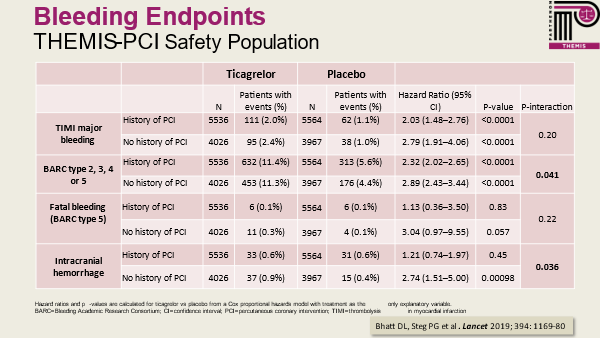
15) In the subgroup of 58% of patients with previous history of PCI, the relative risk reduction was 15% (Lancet 2019;394:1169-80). 

16) Safety outcomes showed ticagrelor increased the risk of bleeding, with a greater increase in patients without a history of PCI 
17) Net clinical benefit (defined as a composite of irreversible harm events: death, MI, stroke, fatal bleed or ICH) was favorable in patients with a history of PCI but not without a history of PCI (interaction p value = 0.012). 

18) Before we leave, let’s review today’s data. In THEMIS, the net clinical benefit (defined as the composite of death, MI, stroke, fatal bleed or ICH) of ticagrelor in patients with a history of PCI was reduced by
19) Mark your answer and return tomorrow for more on DAPT in this high-risk cohort! Come back, #FOAMed @PharmacyUpdates @DocSavageTJU @GreggWStone @DLBHATTMD @DrMauricioCohen @SVRaoMD @SCAI @DFCapodanno @cpgale3 @AtulPathak31 @fjpinto1960 @djc795 @fischman_david @DavidLBrownMD
20) Welcome back to this Journal Club on the #THEMIS study! I am @gabrielsteg and I am happy you found the ONLY source for serialized accredited #tweetorials in #cardiometabolic care! @HeartBobH @GruentzigG @AnkurKalraMD @cpgale3 @AtulPathak31 @fjpinto1960 @pamelasdouglas 

21) Follow this thread for credit! The answer to yesterday's poll is 15%. There was a 15% relative reduction in net clinical benefit with ticagrelor in patients with a history of PCI. Note that there was no benefit in patients without a history of PCI (interaction p value=0.012).
22) In patients with a history of PCI, the benefit of ticagrelor over placebo on reduction of CV death, MI or stroke, appeared to be present for several years after the index PCI 

23) In the entire THEMIS trial population, treatment discontinuation rates were higher with ticagrelor than placebo by approximately 10%, of which 2/3 were related to dyspnea, and 1/3 to bleeding. 

24) Because of the high d/c rates, on-treatment analyses can be informative (but can overestimate treatment efficacy)
The on-treatment analysis of THEMIS suggested a more marked reduction of the primary outcome in excess of 25% in the subgroup of patients with history of PCI.
The on-treatment analysis of THEMIS suggested a more marked reduction of the primary outcome in excess of 25% in the subgroup of patients with history of PCI.

25) So, to summarize the main THEMIS findings
- In patients with stable CAD and diabetes, but without prior MI or stroke, ticagrelor+ASA reduced CV death, MI or stroke, compared to ASA alone
- this benefit was achieved at the expense of increased major bleeding
- In patients with stable CAD and diabetes, but without prior MI or stroke, ticagrelor+ASA reduced CV death, MI or stroke, compared to ASA alone
- this benefit was achieved at the expense of increased major bleeding
26) The main THEMIS PCI findings can be summarized as follows: in patients with prior history of PCI, ticagrelor was as effective as in the overall trial, but safety was better and therefore ticagrelor+ASA produced a 15% net clinical benefit
27) Let’s find out what is your current antiplatelet management of patients with stable CAD and diabetes (no prior MI or stroke)
28) State your position and return tomorrow for a wrap-up and a link to FREE CE/#CME ! Poke @DavidLBrownMD @radcliffeCARDIO @BorregaardBritt @AgewallStefan @DrM_ODonoghue @aayshacader @mirvatalasnag @cardio73 @biljana_parapid @DrMarthaGulati @ShrillaB @Ortega_Paz @SripalBangalore
• • •
Missing some Tweet in this thread? You can try to
force a refresh