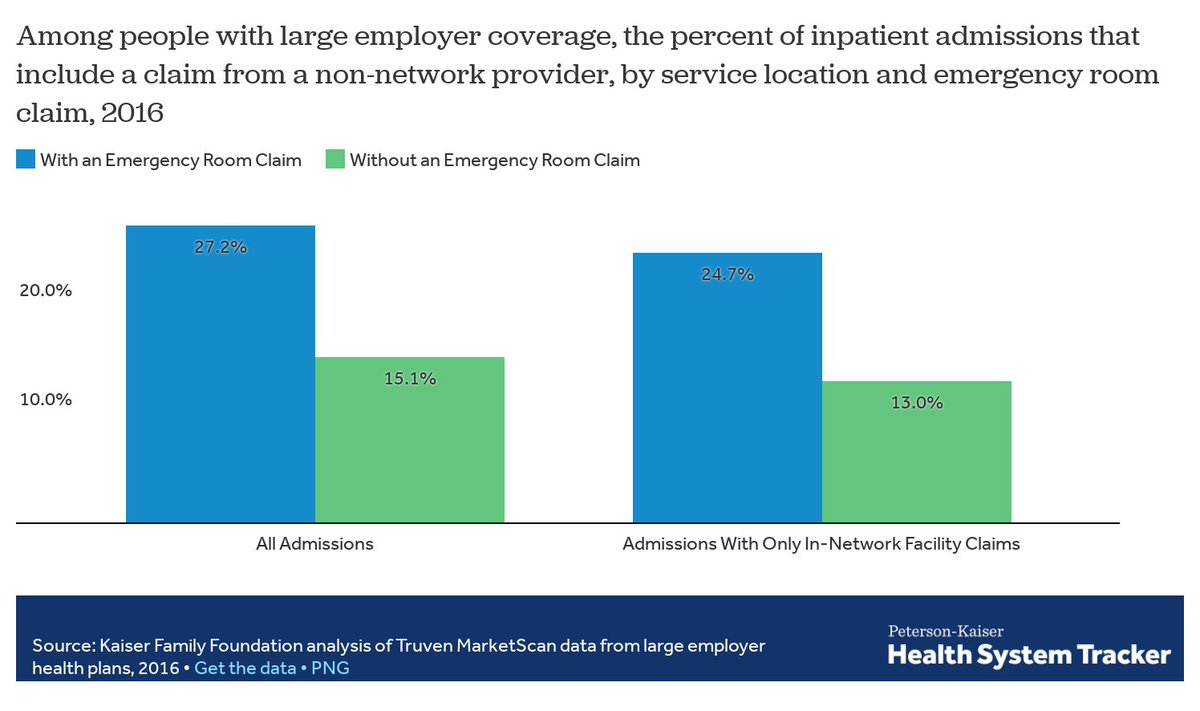
With new regulations on #SurpriseBills expected to drop momentarily, a reminder that about 1 in 5 emergency visits results in an out-of-network charge, putting patients at risk of surprise bills healthsystemtracker.org/brief/an-exami… 

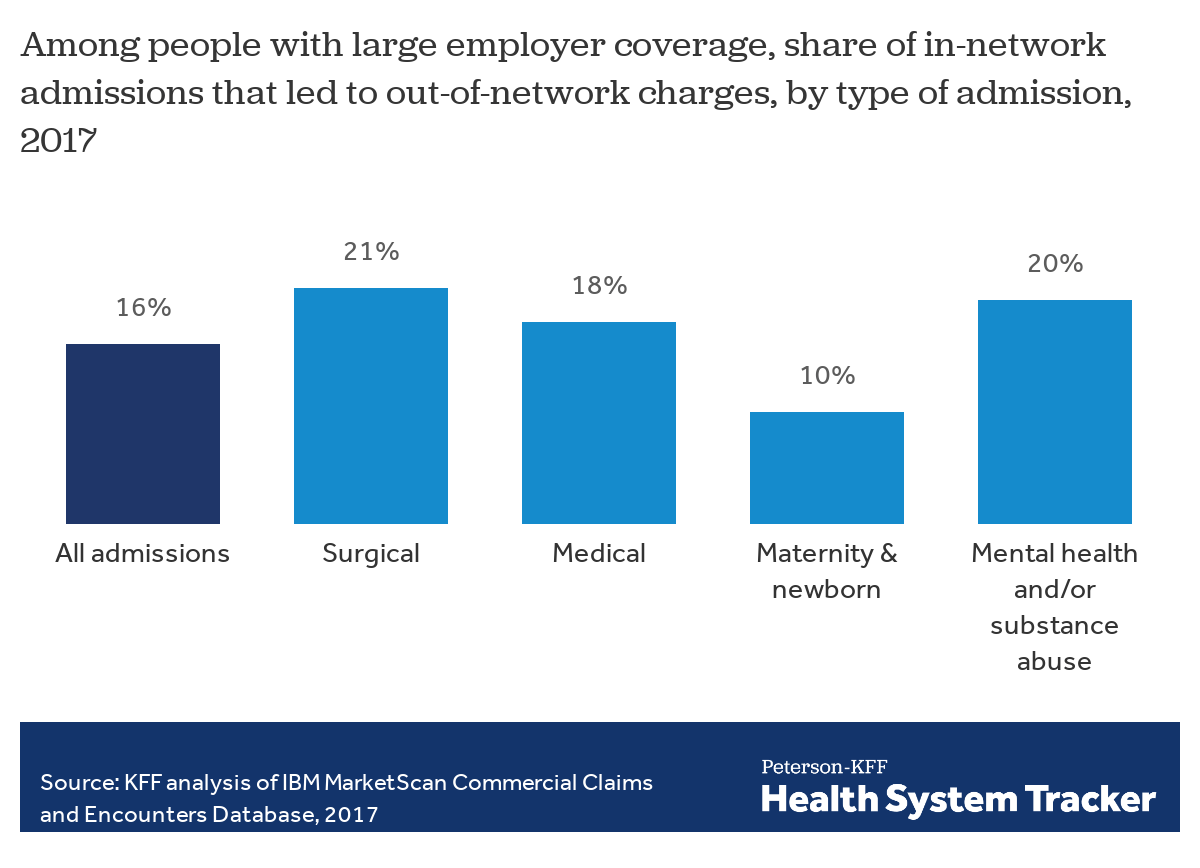
Even for childbirth -- something patients have months to prepare for, and it's common for new parents to even go on TOURS of hospitals in preparation for -- 1 in 10 in-network hospitalizations comes with an out-of-network charge healthsystemtracker.org/brief/surprise… 
Soon, most surprise billing practice should stop with implementation of the No Surprises Act.
But there are holes in these protections, particularly for ground ambulance rides (which are exactly the sort of situations patients feel powerless in). healthsystemtracker.org/brief/ground-a…
But there are holes in these protections, particularly for ground ambulance rides (which are exactly the sort of situations patients feel powerless in). healthsystemtracker.org/brief/ground-a…
And, ICYMI, Krutika pulled together a helpful list of key questions to look out for in the #NoSurprisesAct rules. Some of these questions may be answered today, others in future rulemaking.
https://twitter.com/KrutikaAmin/status/1410277715098279936?s=20
Some info in trickling in: Here are model disclosure notices for surprise billing patient protections and standard notice & consent documents under the No Surprises Act cms.gov/httpswwwcmsgov… 

Hopefully patients read before they sign: "You shouldn’t sign this form if you didn’t have a choice of providers when receiving care. For example, if a doctor was assigned to you with no opportunity to make a change."
And here's the rule: cms.gov/files/document…
The interim final rule for the No Surprises Act includes ways for patients to opt out of these protections, but importantly says that providers cannot prompt patients to waive protections in circumstances where surprise bills are likely to occur 

The rule also calls out insurers that deny emergency coverage based on final diagnosis as being in violation of the No Surprises Act and the ACA 

There's still a question of whether and how these surprise bill protections will apply to urgent care facilities. The Biden Admin is seeking comment on whether patients tend to use urgent care in the same way they do free-standing ERs 

For now, there isn't a timeline of when complaintants must file a complaint about a #SurpriseBill violation, but the Biden Administration is seeking comments on whether the complaining party should have to act within 90 or 180 days 

Still making my way through the rule, but there is some good and bad news for patients in here:
The good includes that emergencies are defined broadly & retroactive ER coverage denial is no longer allowed.
The bad is that some patients might inadvertently sign away their rights
The good includes that emergencies are defined broadly & retroactive ER coverage denial is no longer allowed.
The bad is that some patients might inadvertently sign away their rights
• • •
Missing some Tweet in this thread? You can try to
force a refresh