1/In 2007, after a wave of >1000 fentanyl overdose deaths, I wrote that the fundamental barrier to saving lives was a reluctance to “speak with outrage, and with love, about the lives that have been lost”
Nobody would publish it! I wonder “was I wrong?”
stefankertesz.medium.com/flashback-2007…
Nobody would publish it! I wonder “was I wrong?”
stefankertesz.medium.com/flashback-2007…

2/I am asking seriously. My thought had been “if we speak now and say these lives matter to us, we will do everything in our power to save them”.
What is the lesson of the last five years? Have our actions been insufficient? Many state policies: jamanetwork.com/journals/jaman…
What is the lesson of the last five years? Have our actions been insufficient? Many state policies: jamanetwork.com/journals/jaman…
3/That last paper suggests the success of prescription opioid control just pushed the number of deaths ⬆️ as people with opioid use disorder shifted toward more lethal product. But such state level models are never free of fault. 

4/Actual expansion of addiction treatment has happened with poor penetration to many communities and the gap (Need vs Availability) is either not being closed or not closed enough jamanetwork.com/journals/jama/…
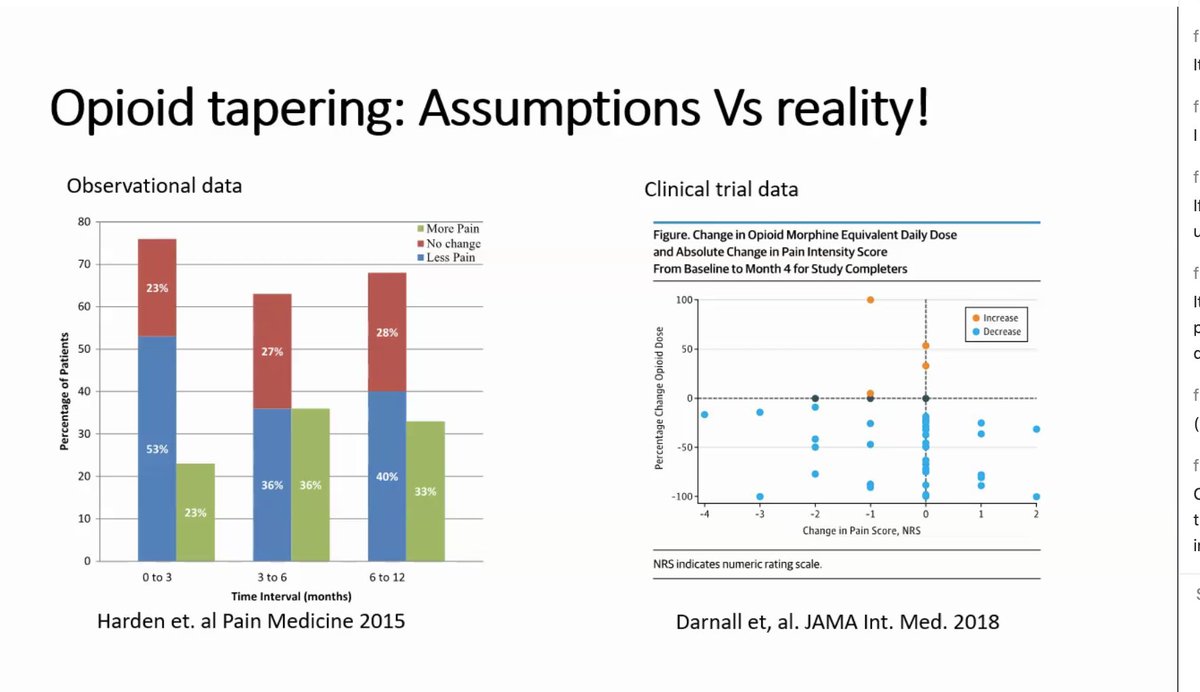
5/From the frontlines I see an enormous number of new clinicians across professions who are *taking up the call* of service for addiction, at least in regard to buprenorphine prescribing - but we are starting from a depleted baseline sciencedirect.com/science/articl…
6/At least 4 gaps remain: First addiction care is still not a mainstream requirement in training of licensed clinicians. This could have been fixed by the boards that credential & certify schools and training programs, years ago. Addiction kills 100s of thousands a year.
7/The 2nd issue is that we often approach addiction treatment and “opioid crisis” without reference to a web of needs that can alter or undermine recovery -trauma, disability, racial or ethnic bias, poverty, inability to get work due to justice involvement, loneliness
8/3rd gap is: sustaining the professionals who seek to work with highly vulnerable & challenging populations depends on supporting them, paying them & celebrating their work.
Our sad tradition has been this:
to marginalize the professionals who care for the marginalized
Our sad tradition has been this:
to marginalize the professionals who care for the marginalized
9/the 4th gap is our society is not in agreement about what is okay to do in the name of safety for people who might use drugs, and either do not have addiction (the majority),
or who have addiction but are not at this moment seeking treatment.
That is a safety issue
or who have addiction but are not at this moment seeking treatment.
That is a safety issue
10/I also note that a component of our policy responses involved changing opioid prescriptions- without a shared notion as to what it would mean to change people’s care and without including the people affected by those changes in the planning or action phases
11/To answer the question i started with. I wasn’t wrong to declare that our absence of outrage was a discouraging sign in 2007. Shared commitments would have been a necessary (but far from sufficient) step toward saving lives. /fin
• • •
Missing some Tweet in this thread? You can try to
force a refresh