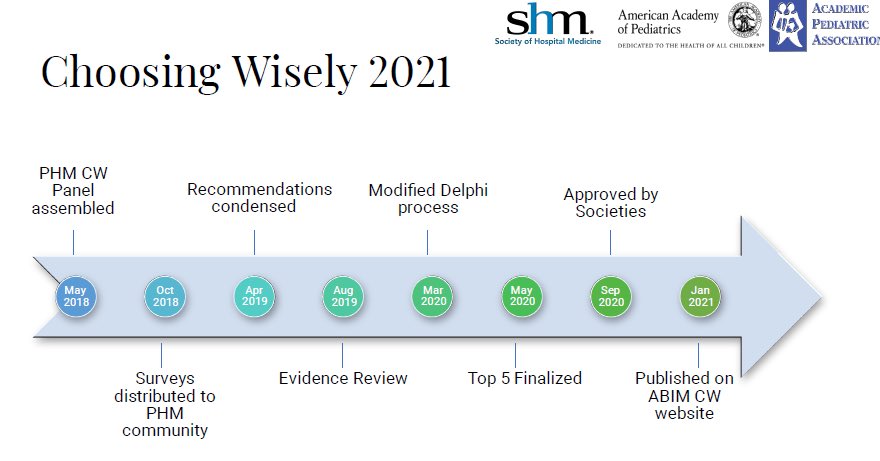
Attending an engaging session at #PHM21 on #ChoosingWisely in Pediatric Hospital Medicine. Dr. Vivian Lee providing the background of how this came to be. 1/thread 
3/ He notes:
- Abx courses with pre-set durations aren’t based on high quality evidence
- Earlier transition to enteral abx can achieve equal outcomes
- Abx courses with pre-set durations aren’t based on high quality evidence
- Earlier transition to enteral abx can achieve equal outcomes
4/ Earlier transition based on individual response can decrease:
-PIV complications
-PICC complications
-Nosocomial infections
-Emotional & Financial Burdens
-Healthcare Costs
-Abx resistance and other adverse effects
-PIV complications
-PICC complications
-Nosocomial infections
-Emotional & Financial Burdens
-Healthcare Costs
-Abx resistance and other adverse effects
6/ The evidence does not support that keeping them longer would really help us catch more positive blood cultures or improve clinical outcomes. 



7/
- Blood culture yield is highest in first 12-36 hours with many studies showing >90% positive by 24 hours
- If adequate outpatient f/u assured, then discharge of well-appearing febrile infants will decrease LOS, abx exposure and iatrogenic complications
- Blood culture yield is highest in first 12-36 hours with many studies showing >90% positive by 24 hours
- If adequate outpatient f/u assured, then discharge of well-appearing febrile infants will decrease LOS, abx exposure and iatrogenic complications
9/ Risk of kernicterus and cerebral palsy is extremely low in otherwise healthy term & late preterm newborns. This slide was very illustrative. In the end, subthreshold phototherapy leads to unnecessary hospitalization (therefore costs and harms). 

11/ She notes that this is consistent with 2011 IDSA guidelines and subsequent studies (see slide) have reaffirmed this practice as no significant difference between cost and length of stay (mostly) 

13/ Use of Sepsis Calculators reduced antibiotic use by 50% or more without increase incidence of early onset sepsis. The following slide showing the initiation of EOS calculator was visually impressive! 

Tagging @vlee_md (sorry I missed a few twitter handles)!
14/ @fcisco1_alvarez was able to do a quick speed run to round off the Top 10 and some other noteworthy pearls: 



Tagging @Alison_HospPeds (Sorry that I missed your twitter handle!)
15/fin
Takeaways:
1) Be a good abx steward. There is evidence for switching from IV to PO. Use narrow coverage if supported by the evidence.
2) Bacterial Cultures are rarely significantly positive >24-36 hours
3) Try to reduce length of stay by being evidence based w/ treatment
Takeaways:
1) Be a good abx steward. There is evidence for switching from IV to PO. Use narrow coverage if supported by the evidence.
2) Bacterial Cultures are rarely significantly positive >24-36 hours
3) Try to reduce length of stay by being evidence based w/ treatment
• • •
Missing some Tweet in this thread? You can try to
force a refresh