1/ #Tweetorial Part 2- Now its time to talk about….
CHRONIC
C-L-O-T
#VTE #DVT #Thrombectomy #Lytics #Cardiotwitter #IRAD #Medthread #Clot @CardioBot @RadialFirstBot @BotPci @EPeeps_Bot @TAVRBot @MedTweetorials @UjjwalRastogiMD @Umair2017 @Umair2017 @VenuVadlamudiMD
CHRONIC
C-L-O-T
#VTE #DVT #Thrombectomy #Lytics #Cardiotwitter #IRAD #Medthread #Clot @CardioBot @RadialFirstBot @BotPci @EPeeps_Bot @TAVRBot @MedTweetorials @UjjwalRastogiMD @Umair2017 @Umair2017 @VenuVadlamudiMD

2/ How much time does it take for #ChronicClot to START to form?
#Fellowstwitter #fellows #fellowtwitter #medtwitter #Clottwitter #VTE @MedTweetorials @CardioBot #Tweetorial #Meded @GAEscobarMD @ekgpdx @HeartOTXHeartMD @EM_RESUS @Pooh_Velagapudi @Vascupedia_com @Dr_Bowser
#Fellowstwitter #fellows #fellowtwitter #medtwitter #Clottwitter #VTE @MedTweetorials @CardioBot #Tweetorial #Meded @GAEscobarMD @ekgpdx @HeartOTXHeartMD @EM_RESUS @Pooh_Velagapudi @Vascupedia_com @Dr_Bowser
3/ Clot is in a constant state of evolution. #Fibrin—> #Collagen.
Unfortunately many patients present in the subacute or late phase of #clot development which hinders many of our treatment approaches.
7️⃣days- 20% collagen
1️⃣5️⃣ days- 50% collagen
2️⃣1️⃣days- 80% (!!) collagen
Unfortunately many patients present in the subacute or late phase of #clot development which hinders many of our treatment approaches.
7️⃣days- 20% collagen
1️⃣5️⃣ days- 50% collagen
2️⃣1️⃣days- 80% (!!) collagen

5/ Pathophysiology of chronic clot formation.
It’s important to recognize the lesions that can form after a clot:
Spurs/Webs
Rokitansky/NIVL/fibrosis
Your pts CEAP >5 always consider for non thrombotic obstructions!
It’s important to recognize the lesions that can form after a clot:
Spurs/Webs
Rokitansky/NIVL/fibrosis
Your pts CEAP >5 always consider for non thrombotic obstructions!

6/ How about a patient case scenario to show some important concepts we will be covering today?
Middle age gentleman with no past medical hx presents to the hospital with 7 days of LLE swelling and 3 days of significant calf and knee pain. Labs normal, DDI elevated. LE duplex:
Middle age gentleman with no past medical hx presents to the hospital with 7 days of LLE swelling and 3 days of significant calf and knee pain. Labs normal, DDI elevated. LE duplex:
7/ Patient is placed on IV heparin. Due to significant pain and swelling as well as presence of unprovoked ilofemoral #DVT we decided to escalate therapy to #MechanicalThrombectomy (with #IVUS)
8/ How important is #IVUS in the diagnosis and treatment of #DVT
@HadyLichaaMD @VladLakhter @ESHLOF @agtruesdell @JayMathewsMD @raddrduke @SDhandMD @CHICKVIR @austinbourgeois @ajgunnmd @abrandismd @IR_doctor @LessneVIR @VIR_li @_Backtable @drochohan @keithppereira @IRkhalsa
@HadyLichaaMD @VladLakhter @ESHLOF @agtruesdell @JayMathewsMD @raddrduke @SDhandMD @CHICKVIR @austinbourgeois @ajgunnmd @abrandismd @IR_doctor @LessneVIR @VIR_li @_Backtable @drochohan @keithppereira @IRkhalsa
9/ So because of the extensive ilofemoral DVT I decided to go left popliteal for access. KEY- make sure you know vascular #ultrasound! Don’t get fooled and stick the superficial system. Look for the saphenous sheath/eye vs the deep veins running with corresponding artery! 

10/ 8F sheath for 0.035 #IVUS, confirm you are in deep system
✅artery with vein all the way up
✅check for compression
✅check for signs of chronic changes
✅check for caval thrombus.
#DVT #Thrombectomy #irad #cardiotwitter #medtwitter #medthread #tweetorial
✅artery with vein all the way up
✅check for compression
✅check for signs of chronic changes
✅check for caval thrombus.
#DVT #Thrombectomy #irad #cardiotwitter #medtwitter #medthread #tweetorial
11/ Chronic changes come in all shapes and sizes. What are two terms that describe lesions related to chronic #DVT
@raddrduke @SDhandMD @CHICKVIR @austinbourgeois @ajgunnmd @abrandismd @IR_doctor @LessneVIR @VIR_li @VladLakhter @drochohan @keithppereira @IRkhalsa @HadyLichaaMD
@raddrduke @SDhandMD @CHICKVIR @austinbourgeois @ajgunnmd @abrandismd @IR_doctor @LessneVIR @VIR_li @VladLakhter @drochohan @keithppereira @IRkhalsa @HadyLichaaMD
12/ So we have compression and signs of venous web/spur with extensive ilofemoral acute on chronic DVT. We have a few ways to treat here. I elected for mechanical thrombectomy with @InariMedical #ClotTriever. Size up to 13 F and start removing that clot.
*Dif vid for ed purposes
*Dif vid for ed purposes
13/ 8 passes later, significant “Extirpation of matter achieved” (know this phrase!). Next reIVUS to further assess compression burden and consider venoplasty and stenting.
#SingleSession #NoICU #NoLytics @drmoinlala @djc795 @DrAmirKaki @Dr_DanMD @LuaySayed @IvanHansonMD
#SingleSession #NoICU #NoLytics @drmoinlala @djc795 @DrAmirKaki @Dr_DanMD @LuaySayed @IvanHansonMD
14/ IVUS with >80% compression (overlying art) in com and ext iliac veins. Venoplasty with a 14 mm balloon followed by stenting with 18 x 150 mm self exp stent. Important key! Don’t overlap stents at inguinal lig and don’t over post dilate inflow (can create new compression). 

15/ So why was treating this #DVT important?
#MedThread #PTS #Tweetorial #IRAD #Vascular #Cardiology @TheNarulaSeries @timir_paul @mirvatalasnag @FredWuMD @trivaxheartmd @SimonDixonMBChB @amrabbasmd @RezaEmaminia @Almanfi_Cardio @Emad_Abdelhay @jaygirimd @AkhilGulati
#MedThread #PTS #Tweetorial #IRAD #Vascular #Cardiology @TheNarulaSeries @timir_paul @mirvatalasnag @FredWuMD @trivaxheartmd @SimonDixonMBChB @amrabbasmd @RezaEmaminia @Almanfi_Cardio @Emad_Abdelhay @jaygirimd @AkhilGulati

16/ Looking at the previous picture of his leg pre procedure—> Notice the mottling, darkening, and swelling. What is this called?
#ChronicVTE #DVT #VTE #Medthread #Tweetorial #PTS @MedTweetorials @leith_erica @KarenWooMD @sewveindoc @jeredcookmd @SanChris999 @drvasimlala
#ChronicVTE #DVT #VTE #Medthread #Tweetorial #PTS @MedTweetorials @leith_erica @KarenWooMD @sewveindoc @jeredcookmd @SanChris999 @drvasimlala
17/ Our goal with these procedures- improve QOL by preventing/improving post thrombotic syndrome (#PTS)!
Factors ➡️ PTS:
🩸extent of #DVT
🩸rate of recanalization;
🩸Episodes of ipsilateral DVT recurrence
🩸The extent of venous reflux
🩸#Venous valvular function
Factors ➡️ PTS:
🩸extent of #DVT
🩸rate of recanalization;
🩸Episodes of ipsilateral DVT recurrence
🩸The extent of venous reflux
🩸#Venous valvular function

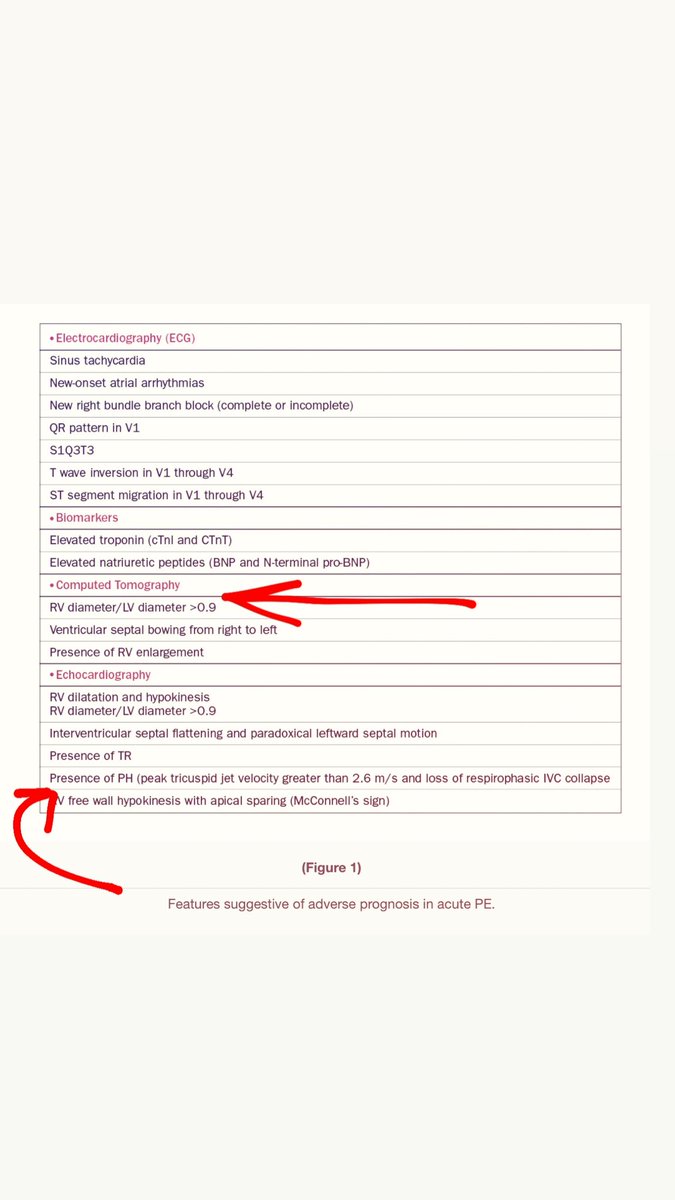
18/ Venous HTN can lead to changes in the capillary and lymphatic microcirculation
➡️ capillary leak
➡️fibrin deposition
➡️erythrocyte and leukocyte sequestration
➡️thrombocytosis, and inflammation.
These changes reduce skin and tissue O2, which in turn cause #PTS
➡️ capillary leak
➡️fibrin deposition
➡️erythrocyte and leukocyte sequestration
➡️thrombocytosis, and inflammation.
These changes reduce skin and tissue O2, which in turn cause #PTS
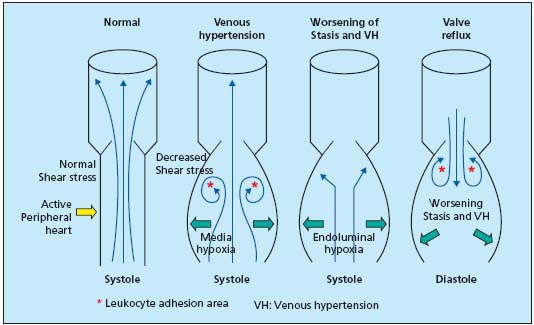
19/ How do we manage PTS and challenges that arise from it?
1st COMPRESSION! Early on, initiate ECS w/ 20-30mmHg knee-high stockings. As sx resolve, progress to 30-40mmHg ECS. The ACCP recommends use of ECS for a min of 2 years from onset of DVT, or longer if a benefit is seen
1st COMPRESSION! Early on, initiate ECS w/ 20-30mmHg knee-high stockings. As sx resolve, progress to 30-40mmHg ECS. The ACCP recommends use of ECS for a min of 2 years from onset of DVT, or longer if a benefit is seen

20/ Problem is- compression stockings fail :(
😔30-65% of patients will fail compression stockings
Raju S, Hollis K, Neglen P
Ann Vasc Surg. 2007 Nov; 21(6):790-5.
😔30-65% of patients will fail compression stockings
Raju S, Hollis K, Neglen P
Ann Vasc Surg. 2007 Nov; 21(6):790-5.

21/ A recent double-blind multicentre RCT (the SOX trial) n= 806 patients compared effectiveness of compression and placebo stockings worn on affected legs daily for 2 yrs. graduated compression stockings did not prevent the occurrence or influence the severity of #PTS
#VTE
#VTE
22/Goal= PREVENT POST THROMBOTIC SYNDROME!! How? Consider thrombectomy! All prox iliofemoral DVT should at least warrant a Cardio/IR/Vasc consult!
Who qualifies- Pts w/ prox clot with residual symptoms despite anticoagulation. Highly consider in young patients to prevent #PTS!
Who qualifies- Pts w/ prox clot with residual symptoms despite anticoagulation. Highly consider in young patients to prevent #PTS!
23/ Ok, so how about lytics? The role of lytics in prevention of #PTS in pts w/ acute DVT is currently being investigated with the ATTRACT study. Pts w/ acute DVT randomly assigned to OAC alone or OAC➕ lytic, which may include use of a pharmacomechanical device to remove the DVT
24/ So with chronic clot what have we learned?
♥️loves to be wall adherent
😖chronic venous changes lead to fibrosis
💉Small bore aspiration is ineffective in removing clot but can create small channels at cost of blood loss.
🧪Lytics seem to be effective for acute clot.
#VTE
♥️loves to be wall adherent
😖chronic venous changes lead to fibrosis
💉Small bore aspiration is ineffective in removing clot but can create small channels at cost of blood loss.
🧪Lytics seem to be effective for acute clot.
#VTE
25/ Additionally—>
☹️Lytics are expensive
☹️Lytics require ICU
☹️Lytics cause bleeding
☹️Lytics don’t work well with chronic
☹️Lytics usually require repeat procedures
#Lytics #singlesession #noTPA #noICU #VTE #DVT #Tweetorial #Medthread #Cardiotwitter #IRAD


☹️Lytics are expensive
☹️Lytics require ICU
☹️Lytics cause bleeding
☹️Lytics don’t work well with chronic
☹️Lytics usually require repeat procedures
#Lytics #singlesession #noTPA #noICU #VTE #DVT #Tweetorial #Medthread #Cardiotwitter #IRAD



26/ This is why I’ve really embraced the @InariMedical #ClotTriever. It is atraumatic to the vein and allows me to remove my worst enemy- Chronic Clot… and most importantly for the patient in a single session with low bleeding risk. #SingleSession #NoICU #NoLytics 

27/ CLOUT analysis
0% venous injury
0% Device related serious adverse events
92% freedom from mod-severe PTS
—> ZERO reports of venous valve damage. #CLOUT #BloodlessThrombectomy
0% venous injury
0% Device related serious adverse events
92% freedom from mod-severe PTS
—> ZERO reports of venous valve damage. #CLOUT #BloodlessThrombectomy

28/ To end - Tips and tricks for crossing chronic clot
First and foremost- IVUS. You have to understand what you are dealing with. MAKE IT YOUR BEST FRIEND!
First and foremost- IVUS. You have to understand what you are dealing with. MAKE IT YOUR BEST FRIEND!

29/ become best friends with a knuckled 0.035 glide advantage and some crossing Catheter
(Generally I cross with the glide and the IVUS)
Sometimes you need a small balloon 4-8 mm to create a channel and also to break up webs
Always know where you are on #IVUS!
(Generally I cross with the glide and the IVUS)
Sometimes you need a small balloon 4-8 mm to create a channel and also to break up webs
Always know where you are on #IVUS!
31/ sources:
EVtoday- diagnosing venous disease with IVUS
Saha et al. Contemporary management of acute and chronic deep venous thrombosis. British medical. 2016
Garcia, m. Aggressive Management of Chronic DVT and the Postthrombotic Syndrome, medscape 2010
Inari medical(COI)
EVtoday- diagnosing venous disease with IVUS
Saha et al. Contemporary management of acute and chronic deep venous thrombosis. British medical. 2016
Garcia, m. Aggressive Management of Chronic DVT and the Postthrombotic Syndrome, medscape 2010
Inari medical(COI)
@NadeenFaza @bcostelloMD @CMichaelGibson @DocSavageTJU @pravinp8 @hpatel824 @onco_cardiology @DocStrom @venkmurthy @SureshSharmaMD @MusaSharkawi @Rahul2282Sharma @NirmanBhatia @ekgpdx @RezaEmaminia @echocardiac @ASE360 @robertomlang @ChinnaiyanMD @purviparwani
@PinakShahMD @Pooh_Velagapudi @DrMarthaGulati @mmamas1973 @MDMankad @SVRaoMD @dr_chirumamilla @willsuh76 @DrSuzyFeigofsky @rwyeh @yourheartdoc1 @DrJRicci @iamritu @DeeDeeWangMD @DrCJBradley @AkhilNarangMD @tarun_jain93 @maquinonesmd @jameschilee @KhandelwalMD
@HeartOTXHeartMD @sarahhudsonuk @avolgman @rahatheart1 @DavidWienerMD @sunnyvmd @monsangh @feelingthepulse @achoiheart @akshitsharmaMD @adcaTicTocDoc @jeredcookmd @rezaemaminia @MartyTamMD @true_EP @sheelakrishmd @skilicmd @ekgpdx @chadialraies @mirvatalasnag
@jameschilee @Babar_Basir @DrHooksDO @chadialraies @ZaherFanari @motownpaesano @GindiRyan @AKassier @AlQarqazM @BobRabbaniMD @SachinParikhMD @TiberioFrisoli @DrAdaStefanescu @dr_chirumamilla @noshreza @UjjwalRastogiMD @majazayeri @SanChris999 @skilicmd
@rajdoc2005 @VMJ_SVM @TopHeartDocs @SVM_tweets @UoMVascSurgery @AorticDissectUS @escardio @ACCinTouch @MichiganACC @EricTopol @GARCIAEDINSON95 @yourheartdoc1 @drjohnm @Medscape @JAMACardio @InvasiveCardiol @cardioPCImom @ferdikiem @keaglemd @JACCJournals @CardiacConsult
@trivaxheartmd @CVCTForum @AbbottNews @HeartFailureTip @heartdocandcrew @HeartDocSharon @heartdoc101 @Heartdoc530 @heartdoc32 @cardioPCImom @JAMACardio @CN_publishing @CardioBot @TomLuscher @CardioMEMS @MedEdChat @CCMedEd @MedEduLab @MedEd_Journal @MedEdConference
@Dr_DanMD @GARCIAEDINSON95 @RonaldWinokurMD @DrYanLiu @RonaldWinokurMD @MarquandPatton @DrAmatangelo @alaa_gabi @bchTicTocDoc @cardioPCImom @CanucksFan80 @RBP0612 @ReentrantDani @ChiznerRyan @ManualOMedicine @grepmeded @pfarrugiamd
@majazayeri @AjayPMD @GuruKowlgi @JorgeP15
@majazayeri @AjayPMD @GuruKowlgi @JorgeP15
@Phil_Wiener @ZainAsadEP @AmrFBarakat @m_ahsan7 @ShanbhagAnusha @DRDAPO @RaidSaco @ikutkutMD @DrDHarmon @AlaMohsen87 @RankaSagar @Nidhi_Madan9 @SaidAshrafMD @AKassier @StrobelAaron @maniaconboard @varda88 @singamnv @SivaTaduru @ShivtejKaushal @RickyHansra @aniket_rali
• • •
Missing some Tweet in this thread? You can try to
force a refresh