
Our study finds #COVID19 clinical risk tools should reflect factors predominantly affecting ethnic minorities including: multiethnic age structures, multimorbidity & deprivation
This will enable early identification & triage to appropriate care (1/10)
bmjopenrespres.bmj.com/content/8/1/e0…
This will enable early identification & triage to appropriate care (1/10)
bmjopenrespres.bmj.com/content/8/1/e0…
Background: Ethnic minorities account for 34% of critically ill patients with COVID-19 despite constituting 14% of the UK population
Effective triage at hospital admission is required to ensure pts from all ethnic groups are risk stratified to appropriate level of care
(2/10)
Effective triage at hospital admission is required to ensure pts from all ethnic groups are risk stratified to appropriate level of care
(2/10)
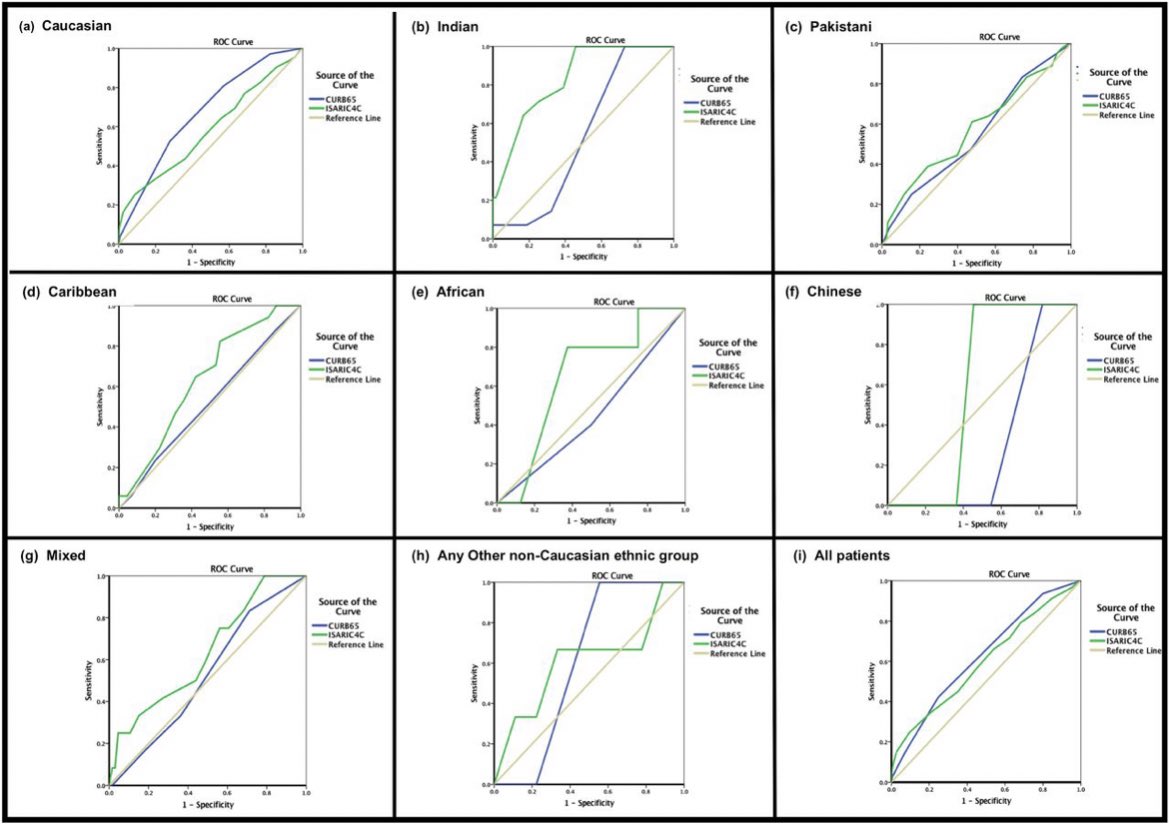
So far it has been unclear how well risk models perform to risk stratify individual ethnic minority groups and whether models sufficiently account for biological and socioenvironmental risk factors to which ethnic minorities are predominantly predisposed inc. #COVID19. (3/10)
Ethnic minorities are more likely than Caucasians to be hospitalised with #COVID19 from most deprived IMD quintile. Data cuts haven’t yet explored IMD subdomains -Barriers to Housing, Living Environment & Adult Skills-on presenting with multilobar pneumonia & ICU admission (4/10)
Admission from areas of highest indoor LE deprivation, outdoor LE deprivation, wider BHS deprivation and adult skills deprivation are associated with multilobar pneumonia on presentation and ICU admission, which are mortality risk factors. (5/10) #COVID 

Ethnic minority groups exhibit different risk profiles inc- different exposure to various derivation types, presentation with multilobar pneumonia and ICU admission - not a one size fits all.
Getting ethnicity coding right is essential @owenchinembiri @NHS_RHO @DrHNaqvi (6/10)
Getting ethnicity coding right is essential @owenchinembiri @NHS_RHO @DrHNaqvi (6/10)

We must develop clinical risk tools that triage patients from all ethnicities to the appropriate care level - admission risk tools must factor in hidden clinical risk factors including deprivation, multimorbidity multiethnic age structures. (7/10) 
Ethnic minorities are younger (yet admission clinical risk tools often score age but not other risk factors such as deprivation or multimorbidity)- look at the average age by ethnicity in the UK. Clinical risk tools must capture multiethnic age structures and risk factors (8/10) 
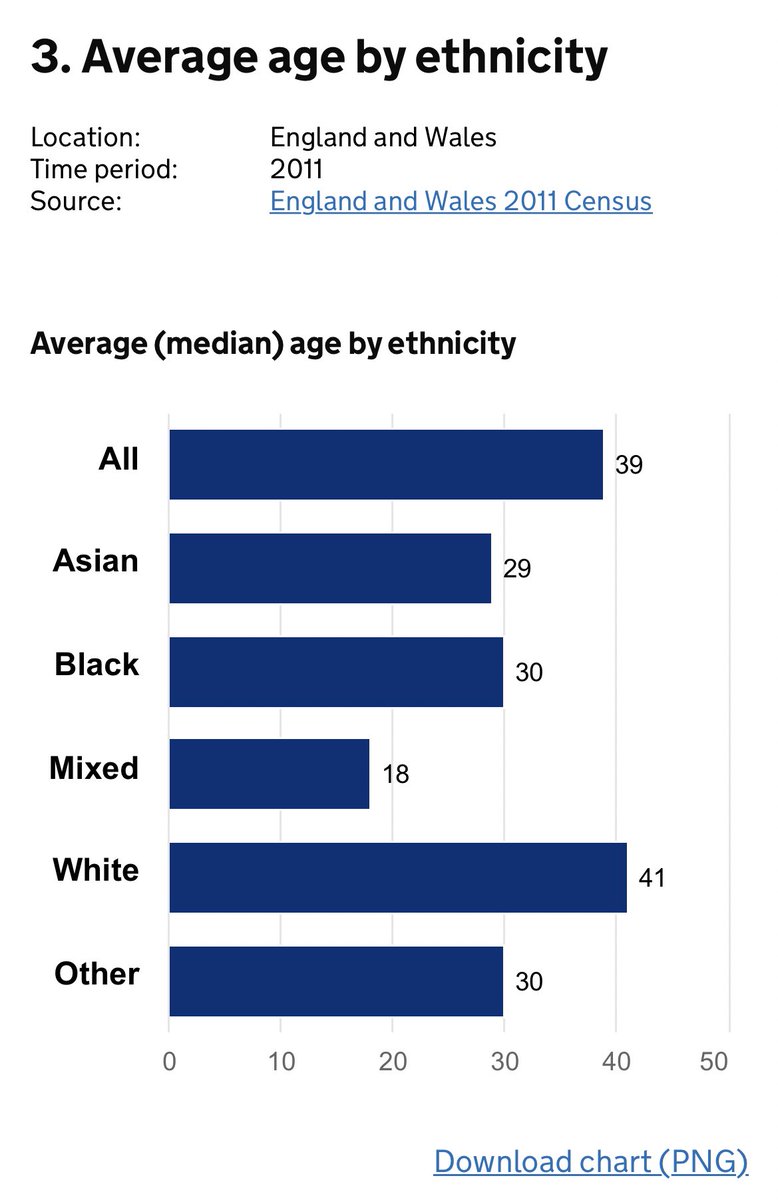
Ethnic minorities exhibit younger age structures, ⬆️ multimorbidity & disproportionate exposure to unscored risk factors inc. obesity & deprivation resulting in potential triage to an inappropriate level of care with clinicians left falsely reassured regarding severity. (9/10)
#COVID-19 admission clinical risk stratification tools need to be developed to account for risk factors to which ethnic minorities are predominantly exposed. This will enable early identification of patients at risk of deterioration & ensure triage to appropriate care (10/10)
With huge thanks as wel @seblugg 👍 (apols couldn’t find your Twitter handle earlier)
• • •
Missing some Tweet in this thread? You can try to
force a refresh



