Covid (@UCSF) Chronicles,Day 521
I can't resist one more thread on boosters. I see lots of debate on data: about antibody levels, infections vs severe infctns, etc. I don't see much about the big issue: the tension between 2 perspectives – that of individuals vs. society.(1/25🧵)
I can't resist one more thread on boosters. I see lots of debate on data: about antibody levels, infections vs severe infctns, etc. I don't see much about the big issue: the tension between 2 perspectives – that of individuals vs. society.(1/25🧵)
It's particularly tricky when talking about a global pandemic since (as we've learned, painfully) no person is an island: individual behavior impacts the collective & vice versa. In pandemics, there's also the matter of who comprises the collective: just domestic or global?(2/25)
For those who don't follow healthcare closely, you've stumbled into a longstanding tension in health policy, one that maps pretty well to two different and (mostly) fraternal fields: clinical medicine and public health.
As a physician (though one with public health... (3/25)
As a physician (though one with public health... (3/25)
... training), I was socialized to see life through the lens of individual patients. When the benefits of a certain strategy (say, a test or a treatment) exceed the harms for a given patient (as determined by sound clinical research), I was taught to offer it. Case closed. (4/25)
Whether MDs should consider "society" in care decisions has long been debated. I remember being influenced by this @NEJM piece published during my training: it argues that "The Doctor's Master" at the bedside must be his/her patient, not society.
nejm.org/doi/full/10.10… (5/25)
nejm.org/doi/full/10.10… (5/25)
The field of public health views its work through a different lens: its primary focus is on the collective health of a society. This leads PH to focus on things like nutrition, clean water and, yes, vaccinations...and not so much on medications, ICUs, x-rays, and the like.(6/25)
Let's not be too binary: good MDs care deeply about society at large; good public health professionals value individual welfare. In many cases, tensions are absent or easily reconciled.
But sometimes they lead to divergent analyses & recommendations. I believe that's...(7/25)
But sometimes they lead to divergent analyses & recommendations. I believe that's...(7/25)
... what underlies the booster controversy, though what comes out in the press & social media sometimes seems like a debate over a few percentage points here and there, or some arcane questions about how to interpret an Israeli vaccine efficacy curve. (8/25)
Against that background, let's consider the facts regarding boosters. I don't think there's much disagreement over the following points (I'll focus on mRNA vaccines in this):
a) The initial performance of Pfizer/Moderna was extraordinary: 95% protection against... (9/25)
a) The initial performance of Pfizer/Moderna was extraordinary: 95% protection against... (9/25)
...symptomatic infection; >99% protection vs. severe infection (hospital/death).
b) mRNAs have proven remarkably safe – some mild & transient side effects but serious ones are super rare. There's no (credible) debate about whether benefits of mRNAs outweigh risks. They do.(10/25)
b) mRNAs have proven remarkably safe – some mild & transient side effects but serious ones are super rare. There's no (credible) debate about whether benefits of mRNAs outweigh risks. They do.(10/25)
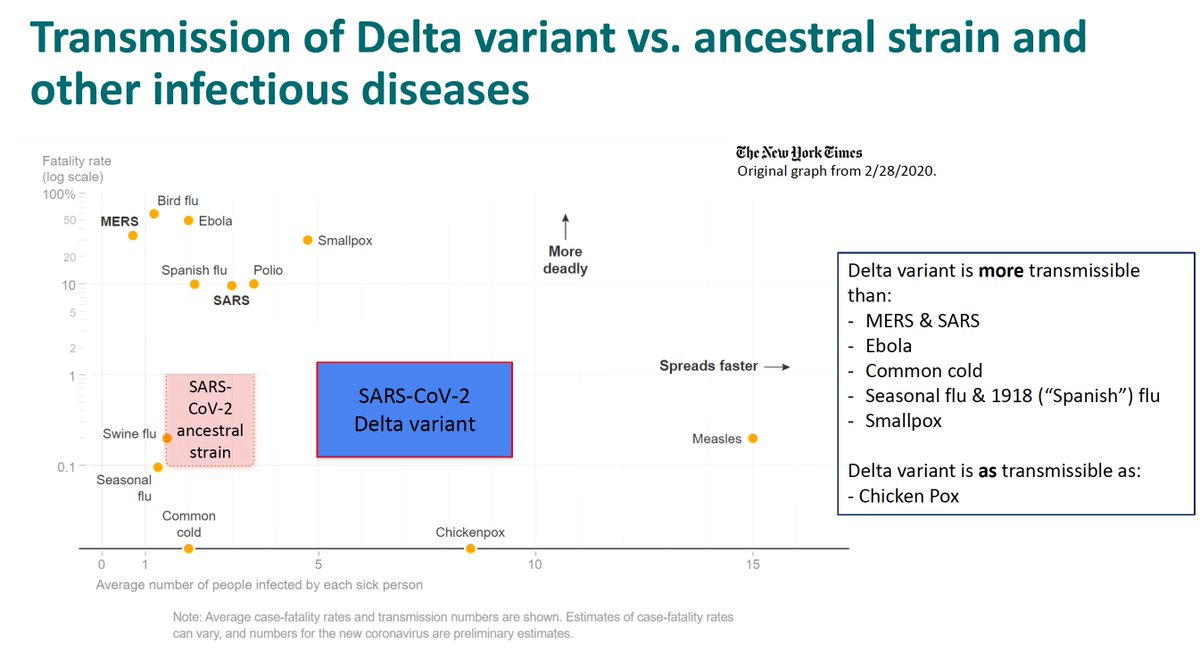
c) There's been a decay in the performance of the vaccines over time. Protection against symptomatic infection is much lower, ~55-80% (vs. original 95%), maybe worse for Pfizer. Protection against SEVERE infection has also decayed, though not as much. Most studies show...(11/25)
...it's fallen from >99% to 70-90%. In other words, vaccines still work well, but the protection is less robust. (You may be surprised how tricky it is to pin down these # s – there are lots of statistical moving parts that influence the estimates. Moreover, it's also...(12/25)
...hard to be sure whether ⬇vax performance is due to ⬇immunity, more infectious virus [Delta], or behavioral change [⬇masking]. In the end, though, if all cases are Delta & folks are being less careful, then it may not matter.)
d) Strong evidence points to declining...(13/25)
d) Strong evidence points to declining...(13/25)
...efficacy (at least against symptomatic Covid) that begins to worsen roughly 6 months after the second shot of Pfizer or Moderna. Empirical observations (not just the finding of lower levels of antibodies) now show that more... (14/25)
...vaccinated people get infected after 6 months, & we're also seeing more serious outcomes. The latter might be partly a consequence of a bunch of factors lining up: older people got vaxxed early, they are more likely to have marginal immunity, and more likely to have...(15/25)
... a bad outcome. Even so, the fact remains that vaccination is no longer as protective as it once was for elders.
e) A booster of some sort (we're mostly talking about 3rd shot of same vax, but mix-and-match seems to work well too) restores immunity at least to the... (16/X)
e) A booster of some sort (we're mostly talking about 3rd shot of same vax, but mix-and-match seems to work well too) restores immunity at least to the... (16/X)
... prior (fully vaxxed) level, & that's associated w/ restored protection. How protected & for how long is not yet known.
f) Side effects & complications of boosters aren't appreciably different from those of original shots.
Putting all of that together, the choice to...(17/25)
f) Side effects & complications of boosters aren't appreciably different from those of original shots.
Putting all of that together, the choice to...(17/25)
...boost (when considering benefits vs. risks to a given patient) seem pretty clear to me: boost, at least in people at heightened risk. And there's not just benefit to the person (less likely to have a symptomatic case, severe case, or Long Covid) but there's community...(18/25)
... benefit as well, as a boosted person is less likely to catch & spread.
So what's the debate about?
When viewing through a public health lens, one asks some other (very reasonable) questions:
a) Wouldn't it be better to give a booster dose to an unvaccinated person?(19/25)
So what's the debate about?
When viewing through a public health lens, one asks some other (very reasonable) questions:
a) Wouldn't it be better to give a booster dose to an unvaccinated person?(19/25)
At a societal level, answer may be yes. But there's a glut of vaccine in U.S.– plenty for BOTH unvaxxed & boosts. Argument "we should concentrate on vaxxing the unvaxxed" rings hollow: What exactly would we gain in our efforts to vaccinate the unvaxxed if we didn't boost? (20/25)
b) Will seeing boosters dissuade some from getting shots 1 & 2? Perhaps, but allowing folks who did the right thing (vax) to get Covid seems like too high a price.
And to me it's equally likely that seeing vaxxed people get sick would dissuade unvaxxed from their shots. (21/25)
And to me it's equally likely that seeing vaxxed people get sick would dissuade unvaxxed from their shots. (21/25)
c) Should we be sending extra shots abroad? The "no one is safe unless everyone is safe" argument is powerful. But for at-risk U.S. patients, safety is better assured by boosting immunity than sending a dose abroad. Yes, U.S. needs to lead efforts to vax the world, but...(22/25)
...withholding beneficial boosts here seems like the wrong way to do that. Plus it's politically unfeasible, even for globally-minded folks.
To me, the arguments for boosting high-risk individuals are compelling. The public health counterarguments are important, but...(23/25)
To me, the arguments for boosting high-risk individuals are compelling. The public health counterarguments are important, but...(23/25)
... we could make them for nearly everything we do in medicine: is it fair to treat diabetes, cancer, or stroke in U.S. w/ expensive, effective therapies when non-U.S. people don't have access? Pandemics ARE different, but in the end I'm swayed by the individual ... (24/25)
...perspective, which leads me to favor boosters for those who will clearly benefit. The tradeoffs seem more philosophical than pragmatic – we CAN do boosters while also putting real energy & resources into efforts to vaccinated the unvaxxed, both here & around the globe.(25/end)
• • •
Missing some Tweet in this thread? You can try to
force a refresh