Impact of radiation therapy facility volume on survival in patients with cancer.
@LeilaTchelebi @wedney2017 @NirajGusani @PennStHershey
Via @JournalCancer @ACS_Research
acsjournals.onlinelibrary.wiley.com/doi/full/10.10…
pubmed.ncbi.nlm.nih.gov/34398470/
@LeilaTchelebi @wedney2017 @NirajGusani @PennStHershey
Via @JournalCancer @ACS_Research
acsjournals.onlinelibrary.wiley.com/doi/full/10.10…
pubmed.ncbi.nlm.nih.gov/34398470/

Facility volume has been explored as a surrogate of quality of care in medicine.
pubmed.ncbi.nlm.nih.gov/12230353/
@AnnalsofIM
pubmed.ncbi.nlm.nih.gov/12230353/
@AnnalsofIM

In oncology, facility surgical volume is correlated with survival.
Work from @StoltzfusKelsey @LeilaTchelebi @DanTrifMD @NirajGusani in @JNCCN
Work from @StoltzfusKelsey @LeilaTchelebi @DanTrifMD @NirajGusani in @JNCCN
https://twitter.com/NicholasZaorsky/status/1364309270028812294
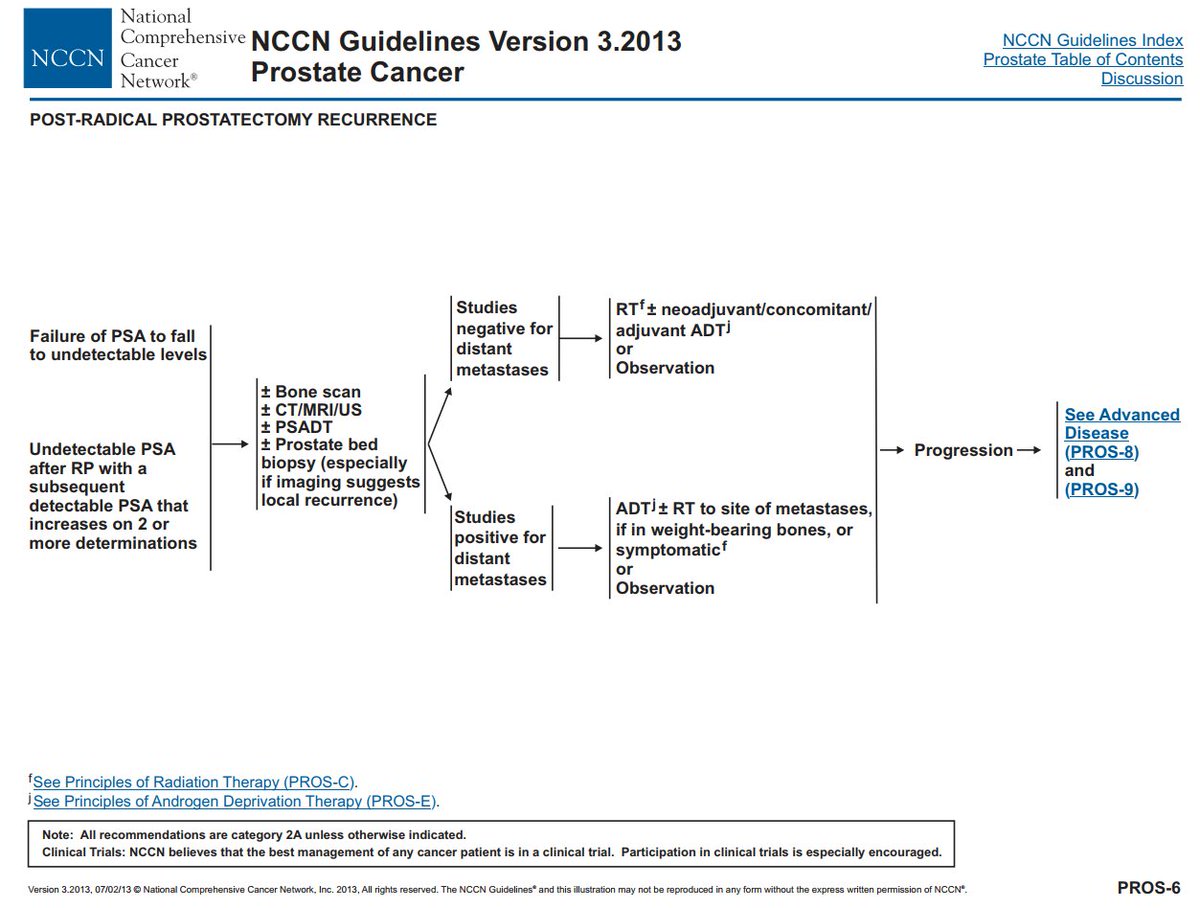
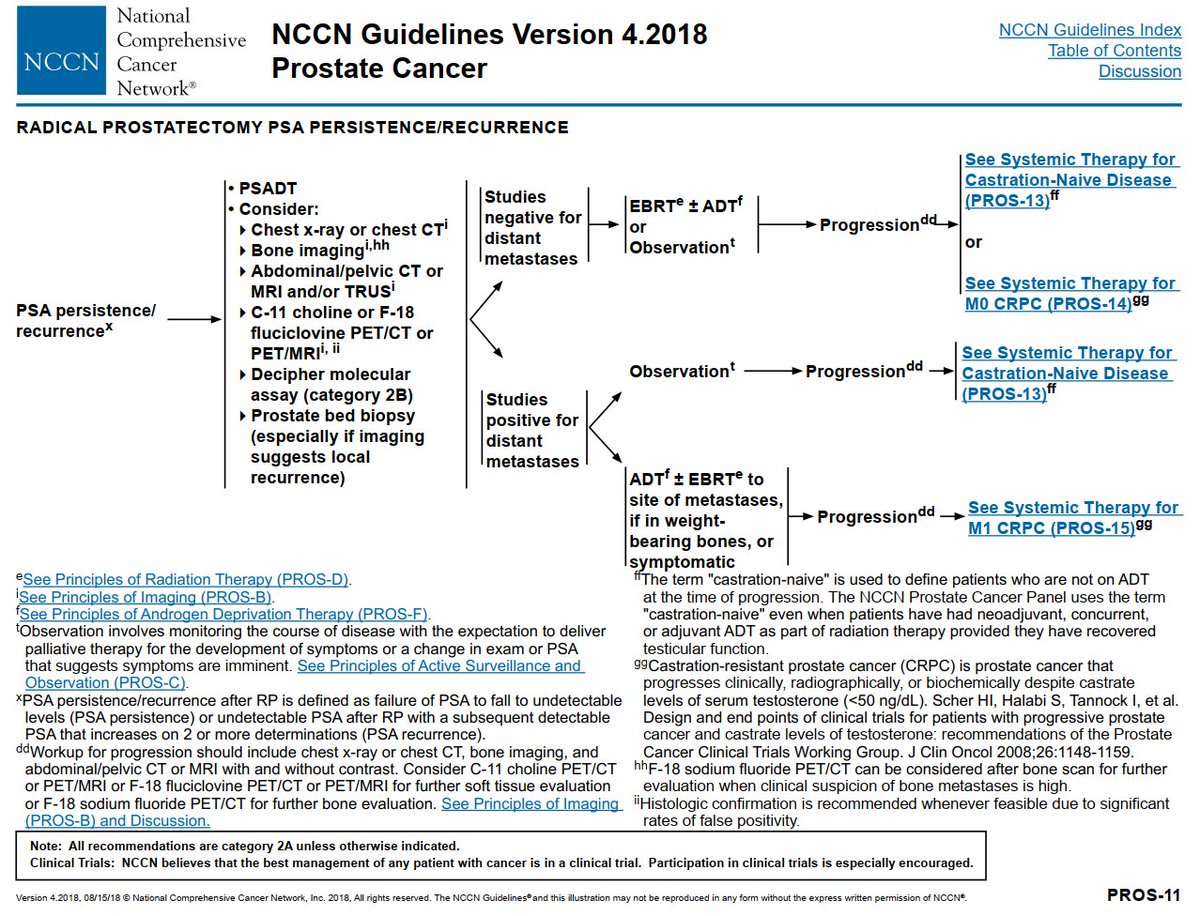
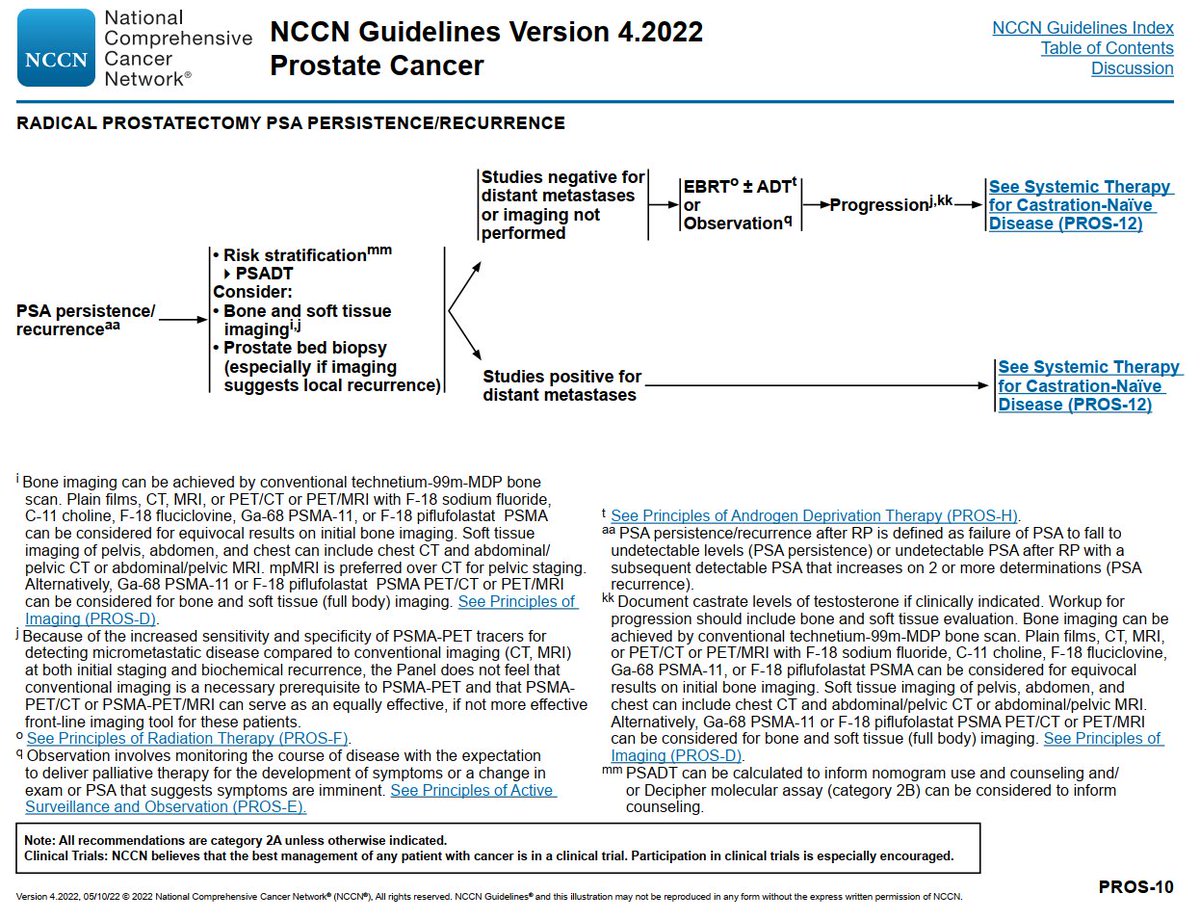
The @NCCN guidelines recommend patients be treated at high volume facilities when receiving treatment, e.g., lung and prostate cancer. #LCSM #PCSM
However, most commentary is on surgery.

However, most commentary is on surgery.


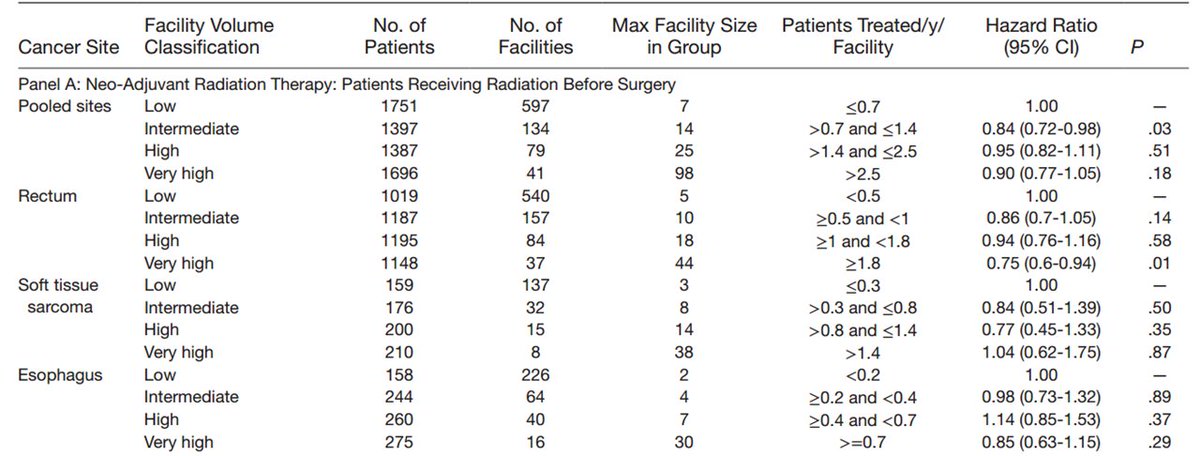
This is the first work to uniformly evaluate facility radiotherapy volume for many cancers.
We use a consistent definition (low, intermediate, high, very high volume) and 3 settings (adjuvant, definitive, neoadjuvant).
#RadOnc


We use a consistent definition (low, intermediate, high, very high volume) and 3 settings (adjuvant, definitive, neoadjuvant).
#RadOnc



If you had to lump all cancer sites and radiotherapy facilities into one figure, it would look like this.
There are:
97 very high volume facilities
178 high volume
284 intermediate volume
772 low volume
each group has 25% of patients; thus, there are more low volume facilities
There are:
97 very high volume facilities
178 high volume
284 intermediate volume
772 low volume
each group has 25% of patients; thus, there are more low volume facilities

Here are pt demographics/characteristics. Most pts we see are in the adjuvant or definitive setting. 

In adjuvant setting, almost all benefit was in breast cancer, but overall clinical impact was limited (a few percent) 



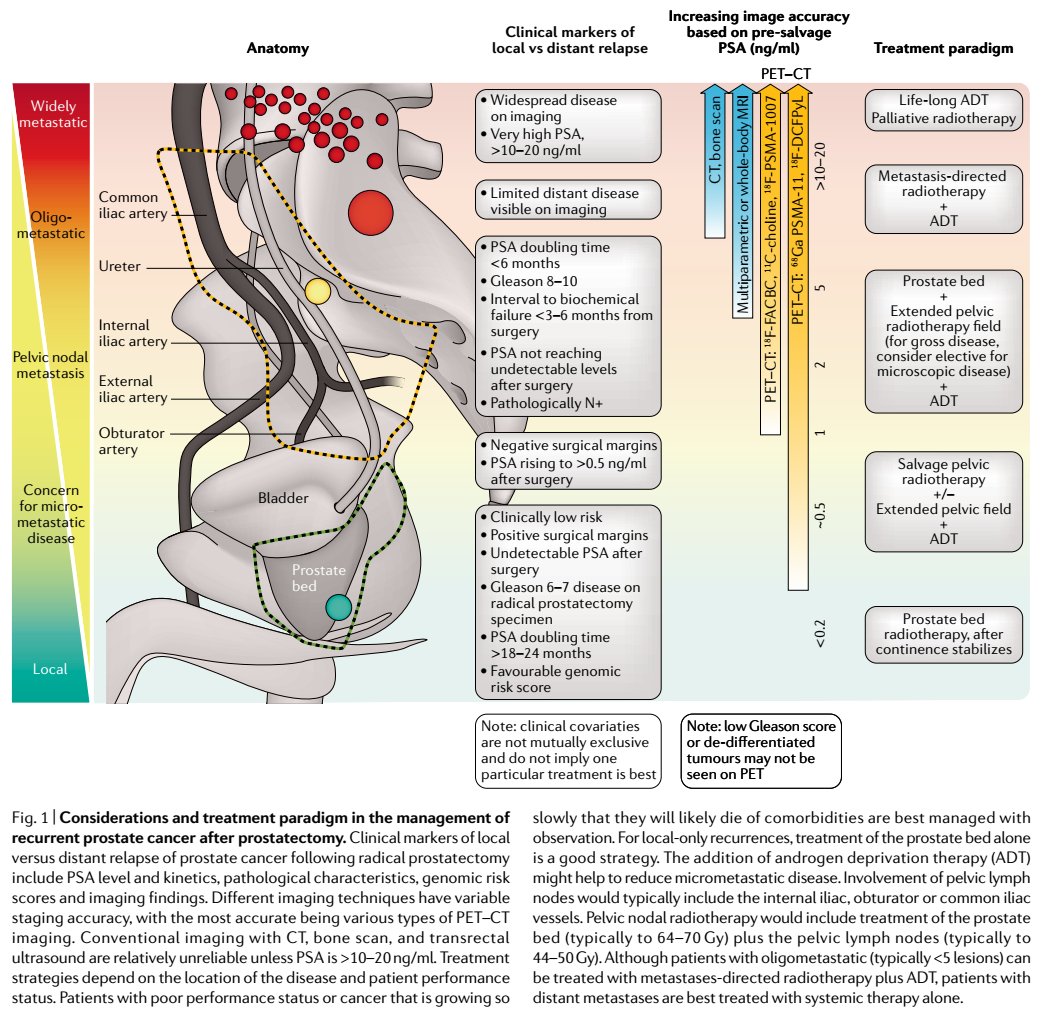
In definitive setting is where we saw most benefit:
non-small cell lung
prostate (though absolute benefit limited)
head and neck

non-small cell lung
prostate (though absolute benefit limited)
head and neck


This work does not include patients treated with palliative radiotherapy at time of initial diagnosis.
FYI, we have a separate prognostic model for those patients (it doesn't involve facility volume):
FYI, we have a separate prognostic model for those patients (it doesn't involve facility volume):
https://twitter.com/nicholaszaorsky/status/1364917128130945025
This work also does not include patients treated with palliative radiotherapy for recurrent disease.
Palliative radiotherapy likely makes up ~20-50% of facility volume for most facilities.
@subatomicdoc @tjroycemd @seanmmcbride do you know of a resource to get those data?
Palliative radiotherapy likely makes up ~20-50% of facility volume for most facilities.
@subatomicdoc @tjroycemd @seanmmcbride do you know of a resource to get those data?
This work also does not include all use of stereotactic radiotherapy / radiosurgery, which may be a significant portion of volume for certain facilities and physicians.
https://twitter.com/NicholasZaorsky/status/1352264313227022337
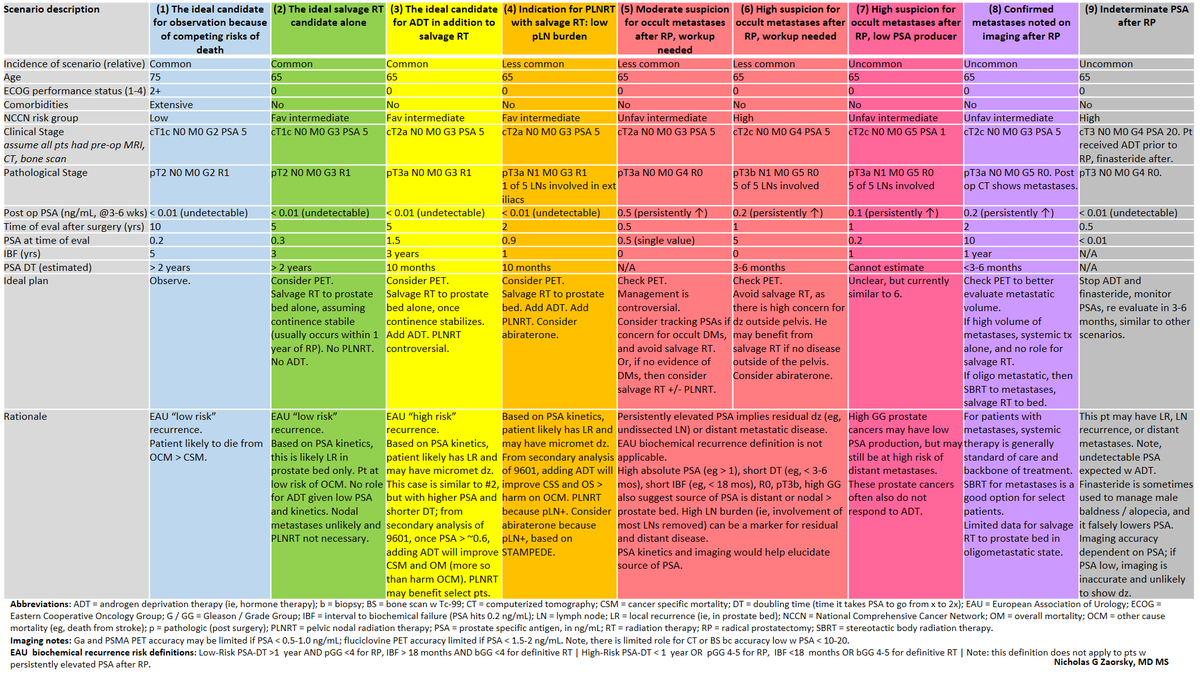
We accounted for covariates like use of surgery, chemotherapy, age, etc. However, there are unknowns. Facility radiotherapy volume may be a surrogate for: access to supplementary hospital services, peer review, clinical trials, expertise, @NCCN guideline concordant care.
@NCCN Our group showed heart disease and stroke are major competing risks of death. Centers that have dedicated cardio-oncology teams to mitigate these risks may have improved survival.
See great work from @Icro_Meattini for breast ca.
https://twitter.com/NicholasZaorsky/status/1254518239243243522
https://twitter.com/NicholasZaorsky/status/1195700095037136898
See great work from @Icro_Meattini for breast ca.
Similarly, some centers have more access to clinical trials. Enrollment on trial likely improves survival.
As @NCCN says in every guideline: "the best management of any patient with cancer is in a clinical trial."
As @NCCN says in every guideline: "the best management of any patient with cancer is in a clinical trial."
https://twitter.com/nicholaszaorsky/status/1192853426603999232
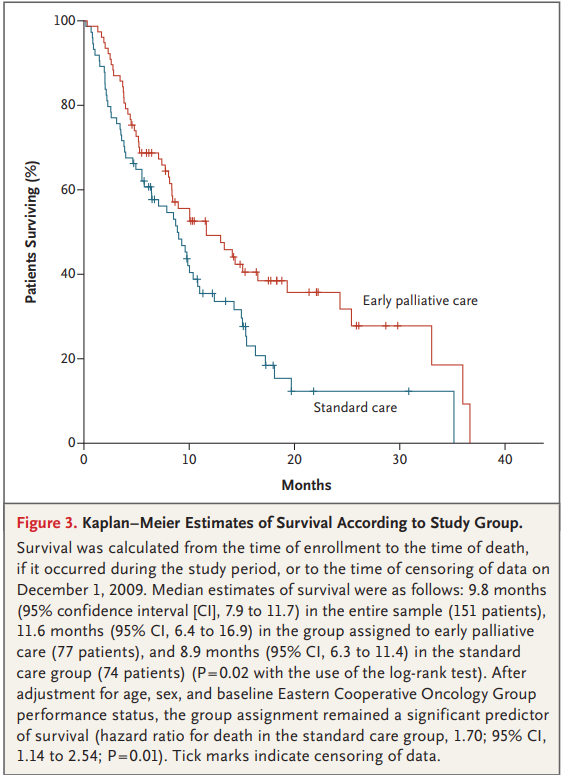
In our study, survival benefit of higher volume facilities was partly driven by lung cancer patients.
These facilities may also have better access to palliative care, which improves survival more than most drugs or radiotherapy techniques.
@NEJM
nejm.org/doi/pdf/10.105…
#PallOnc
These facilities may also have better access to palliative care, which improves survival more than most drugs or radiotherapy techniques.
@NEJM
nejm.org/doi/pdf/10.105…
#PallOnc
• • •
Missing some Tweet in this thread? You can try to
force a refresh