I will now be tweeting from the ''Collaboration and Integration session, chaired by Camilla Rowland #21OPCC
First presenter in this session is Judy Hollingworth talking about 'Palliative care practitioners and community advocates collaborate in a disadvantaged rural region' #21OPCC
After a lovely acknowledgement to country, Judy begins her story about collaboration and causation #21OPCC 

Collaborators incl #palliativecare nurses, specialists. Judy became a #palliativecare volunteer. Community support would make a huge difference to the overstretched system #21OPCC
In a regional area in the Midcoast council region of NSW
"Long way to travel to care, long way for care to travel to the people that need it" - Judy Hollingworth #21OPCC
"Long way to travel to care, long way for care to travel to the people that need it" - Judy Hollingworth #21OPCC

Fastest ageing electorate in the state, and the population is quite scattered geographically. Both pose a challenge to accessing care. #21OPCC
#COVID19 and natural disasters (drought, bushfires) have placed additional impact on access to health in the region in the last few years #21OPCC
Sometimes the most appropriate care is out of the region. Free for patients to leave to access care, but many have to pay for transport back! #21OPCC
Triumph in last 12 months = now have a part-time #palliativecare specialist in the region since Aug 2020 🙂 #21OPCC
Asking for solutions for chronic unmet need of #palliativecare trained specialists in allied health. #21OPCC
#Palliativecare staff appealed to community for support to help minimise the distress in patients and carers, and to support them in not being able to meet or delegate basic needs #21OPCC
Q asked How can we reduce anxiety on patients, carers and colleagues? Community consultation to determine what the level of concern in #palliativecare delivery was #21OPCC
Consultation incl patients, carers and #palliativecare specialists to advocate for #palliativecare, fundraising and raising awareness #21OPCC
Generated relatively large amount of funds via fundraising events, donations and grants #21OPCC - helped to fund practitioners and equipement
(Sorry for spelling error in previous tweet - SB equipment)
Funding also supported 80 people over 4 years in at-home care #21OPCC
Funding also supported 80 people over 4 years in at-home care #21OPCC
Additional staff have been recruited for the region - #palliativecare nurses and allied health workers in both local hospital and community health #21OPCC
It was a true collaborative-community to advocate for better #palliativecare in the region, and a combination of high trust, generosity, alacrity and creativity #21OPCC. Great learnings for other communities
"This kind of spirit lives in every community, I believe" - Judy Hollingworth #21OPCC
Dr Katrin Gerber @NAgeingRI is up next to discuss 'Predicting death - training hospital assessment teams to identify patients nearing the end-of-life' #21OPCC
Being able to predict when people are dying may mean people have better care and opportunity to discuss end-of-life decisions #21OPCC
Research being discussed by Dr Katrin included interviews with assessment teams in Melbourne hospitals #21OPCC
Assessment teams used clinical indicators, assessments from others, visual markers (ie "looks unwell"), intuition to identify patients who might be dying #21OPCC
Why was dying recognised so late in assessment teams? Short duration of contact with patient, staff experience, lack of feedback, system pressure (active treatment + vacate beds) #21OPCC
Insufficient documentation - signs of dying were often not documented, for fear of getting things wrong. Guarded prognosis. Avoidance #21OPCC
Lack of confidence, knowledge and training underpinned the other barriers in identifying when people might die. #21OPCC
Training in a Palliative Prognostic Index, a 5-tool item, was conducted. The Index was used to categorise prognosis by likeliness of when the patient might die (less than 3 weeks, more than 3 weeks) #21OPCC
Tools incl oral intake, oedema, dyspnoea at rest, delirium and palliative performance scale #21OPCC
Pre-post training survey data collected to determine if PPI tool effective #21OPCC
Benefits of the training and implementation of PPI - incl quick and easy, conversation starter, increased confidence in the tool, going beyond intuition in prognosis (quantified gut-feeling) and more specific to begin end-of-life conversations #21OPCC
Challenges incl = knowledge of delirium varied, specificity, time-pressure in hospitals. Points to need for making the PPI a standard part of hospital culture. #21OPCC
Prognostic tools can increase staff's knowledge and confidence in recognising signs of dying. Local champions are needed to answer questions, encourage staff to use the tool. #21OPCC
Next: Joint presentation by Prof Josephine Clayton & Dr Srivalli Vilapakkam Nagarajan, talking about 'The Advance Project: team-based initiation of advance care planning and palliative care in general practices' #21OPCC
The Advance Project is supported by @HammondCare theadvanceproject.com.au
Goals of the second phase of this project incl -
improve care outcomes in Australian GPs, through earlier consideration and uptake of ACP in older and chronically ill patients #21OPCC
improve care outcomes in Australian GPs, through earlier consideration and uptake of ACP in older and chronically ill patients #21OPCC
The Advance Project website links to a wide range of resources, such as 'supporting you to live well with a chronic illness' theadvanceproject.com.au/tabid/5219/Def… #21OPCC
Key findings from the evaluation of the Advance Project incl = mostly positive feedback. The tools help to make the conversation about advance care planning more approachable #21OPCC
The training workshops were rated highly, most participants said that they intended to use the Advance Project resources as part of their routine clinical practice #21OPCC
Patients found the ACP conversation with their GP uncomfortable but useful, and the patient resources on the website were beneficial #21OPCC
Identified facilitators for implementation incl team approach to initiate ACP/#palliativecare conversations beneficial and GP champions play a key part in making changes in initiating conversations #21OPCC
The mentoring aspect of the project plays another key role in implementing the Advance Project #21OPCC
The next steps of the project are to build capacity in aged care setting #21OPCC
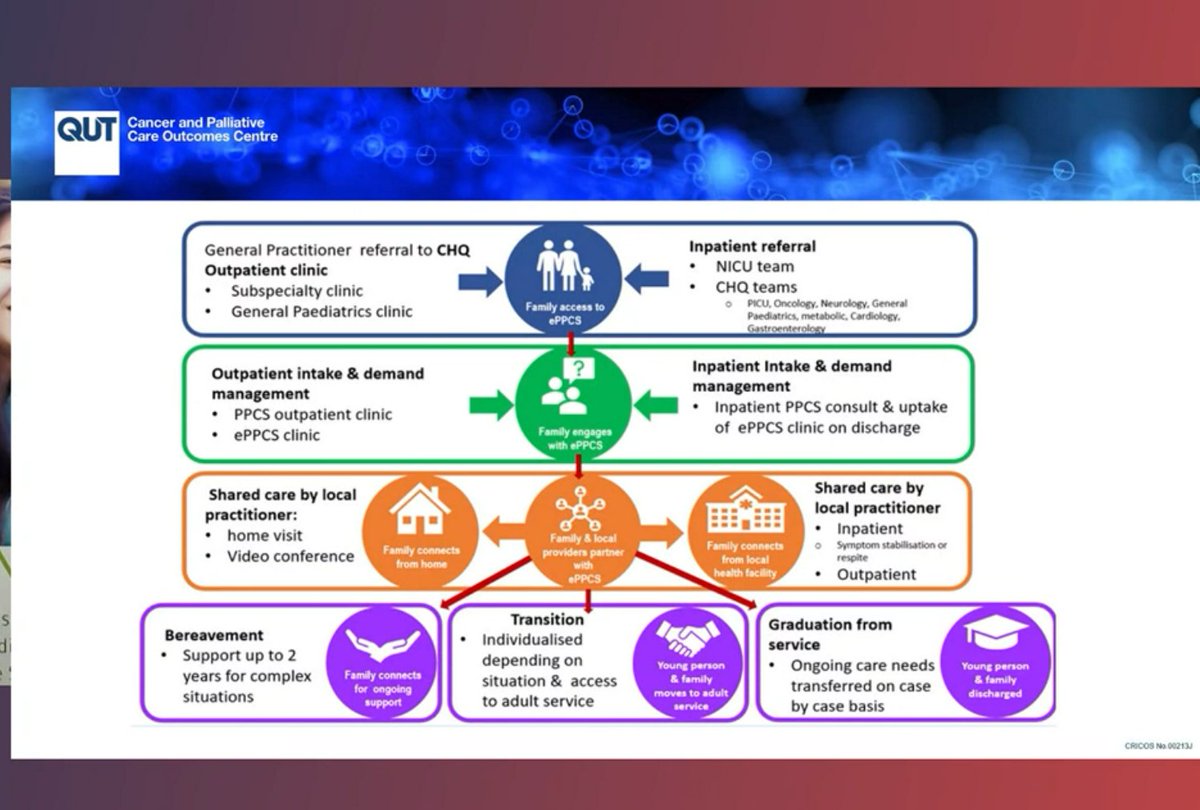
@AlisonBowers12 @QUT will be presenting on the 'Evaluation of the paediatric palliative care outreach collaborative' #21OPCC
EPPCS a collaborative to improve access to paediatric #palliativecare for children and families living in regional, rural and remote areas of Qld #21OPCC
The study used the RE-AIM evaluation framework - (Reach, effectiveness, adoption, implementation, maintenance), by conducting semi-structured interviews. Really useful framework to evaluate implementation projects in #palliativecare #21OPCC
The evaluation of the paediatric #palliativecare outreach collaborative includes anybody outside of SE Qld #21OPCC
Key findings from the telehealth satisfaction survey = the quality of the video image and audio was predominantly perceived as acceptable #21OPCC
Overall, the telehealth system was perceived to be accessible and easy to use #21OPCC
Clinicians did not think the patient-professional rapport was impaired by using telehealth #21OPCC
Findings of the evaluation to date indicate that telehealth outreach may be an acceptable method for delivering paediatric #palliativecare to families in regional, rural and remote QLD #21OPCC
Next speaker is Deborah Cochran at Mercy Health, who will talk about 'Multi-disciplinary SMART clinic for non-malignancy patients and their carers' and has an interest in holistic care #21OPCC
@MercyHealthAus has an out-patient clinic to address #palliativecare needs with a non-malignant end of life illness #21OPCC
Name of clinic = SMART - symptom, management and referral team #21OPCC
Referrals to SMART clinic must be triaged against clinical information, endorsed by medical practitioner and meet state-wide clinic referral criteria #21OPCC
All patients assessed prior to appointment via the PCOC symptom assessment scale - measuring the levels of distress the patient experiences, and the problem severity score #21OPCC
Added two additional tools to assess their cohort - the COPD-CAT (for those with lung disorders) and IPOS for renal patients #21OPCC
Carers' needs were also assessed #21OPCC
Symptom management plans were tailored to meet each patient's needs #21OPCC
#COVID19 impact on the clinic - only opened in begin 2020 to be shut down in April 2021. Phone consults were offered, followed up by home visits #21OPCC
A pleasing result from the clinic is that not one patient has presented to ED since the clinic opened, due to early identification of needs and symptoms - this is a really great result! #21OPCC @MercyHealthAus
A heart-warming acknowledgement to country and moment to acknowledge people we've lost, Rev Jenny Busch, a Chaplain at Children's Hospital QLD, starts her presentation on 'Until the very end: the life-giving work of paediatric' #palliativecare #21OPCC
Qld Health committed to Spiritual care and an important part of holistic care. Spiritual care more about listening, a place to explore questions, focus on a journey rather than a destination #palliativecare #21OPCC
Significant number of people prefer not to be visited by a #spiritualcare provider in hospital #21OPCC
#SpiritualCare is not simply about religion, but most people have questions at the end-of-life and a #spiritualcare provider may be able to help them with #palliativecare #21OPCC 

These 7 aspects may form part of #spiritualcare Experiential, ritual, myth/narrative, doctrinal, ethical, social, material #21OPCC
Two common aspects of faith that #spiritualcare providers may come across are in scripture and in prayer, sometimes not in alignment with clinical practices. Important to ask questions and learn to understand how and why their faith is important to them at end-of-life #21OPCC
Camilla - so important to remember that spirituality is a vital component of #palliativecare #21OPCC
Final presentation in the 'Integration and Collaboration' session is 'Working Smarter Together - an example of true integration to benefit a whole community' by Carol Hope #21OPCC
Significant health challenges in West Moreton (QLD) region - need for integrated model of #palliativecare #21OPCC 

Challenges to develop an integrated model - 'David and Goliath' - govt v non-govt resources. Wanted equitable distribution of work #21OPCC
But, there were also opportunities - shared appreciation of each others challenges, patient and family centred model, greater opportunities to access grants and funding together (as opposed to separately). #21OPCC
One of the first principles of the model was that it needed to meet the changing #palliativecare needs of the West Moreton community #21OPCC
Inpatient unit = combined 20 #palliativecare beds between Ipswich Hospice Care and West Moreton Palliative Care #21OPCC
Clear pathways for referral, shared learning opportunities, shared equipment & resources, and pathways for communication and professional support supported the integrated model of #palliativecare #21OPCC
Future opportunities include Shared clinical roles, research collaborations, shared regional on-call model and shared pandemic response #21OPCC
Similar to many other programs discussed in this session, the project kicked off about the same time as #COVID19. #21OPCC
• • •
Missing some Tweet in this thread? You can try to
force a refresh