Coming up in @kesleeman presentation at #21OPCC - "Doctors desert the dying." Prompted Cicely Saunders to launch the modern hospice movement in the UK 

About 100k people die each year in UK needing palliative care but not receiving it - guess what were some of the determining factors @timsenior #21OPCC 

Need for palliative care globally is escalating - likely to double by 2060 - driven by dementia. #21OPCC
If we assume that average trends 2004-2014 continue, will see dramatic swings by 2040 in UK/Wales, aged care homes deaths (vs hospital/home) could become most common place to die: Sleeman #21OPCC
Before COVID, UK was a leader in palliative but were big gaps and inequalities in care, and a projected large increase in needs.
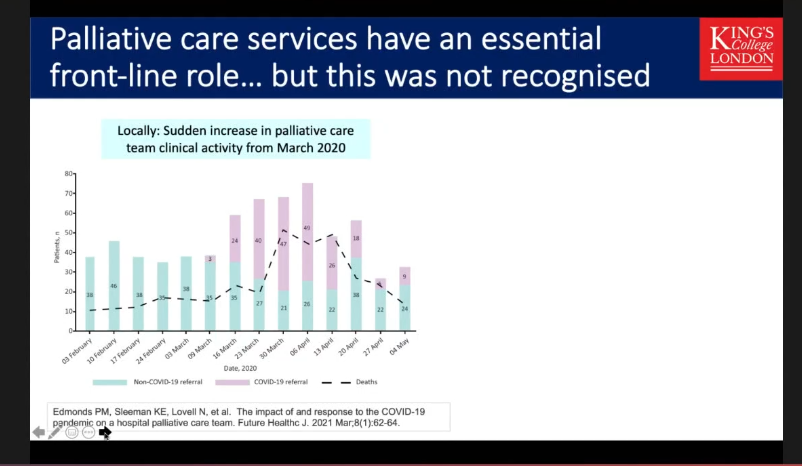
"And then COVID happened". And at first palliative care teams were being diverted....
@kesleeman #21OPCC
"And then COVID happened". And at first palliative care teams were being diverted....
@kesleeman #21OPCC
Palliative care experts did rapid systematic review, found was v little research on palliative care in pandemics but some that there was was rich.
Led to the COVpal study kcl.ac.uk/cicelysaunders…
Led to the COVpal study kcl.ac.uk/cicelysaunders…
Palliative care and hospice services felt overwhelmed and overlooked in early days of pandemic #21OPCC 

First 10 weeks of pandemic: Deaths in care homes increased by 220%, while home and hospital deaths increased by 77% and 90%, respectively. Hospice deaths fell by 20%. journals.sagepub.com/doi/full/10.11… #21OPCC
But longer time, increasing numbers of people dying from home, which not yet explained - people exercising choice to die at home or dying suddenly and not being able to access help? Sleeman #21OPCC 

This study suggested people were choosing to stay at home (GPs and community nurses were stepping in palliative care space). bjgpopen.org/content/5/4/BJ… 

(Excellent tip here for conference presenters who don't want their preliminary research tweeted - as well as saying so (thanks @kesleeman) put a little sign on the slide #21OPCC ) @MelissaSweetDr @coopesdetat 

Pandemic has shown how much we can achieve if clinical academics work together side by side on policy - was fast, innovative and highly successful during COVID but far fewer examples in end of life care than could have been: Sleeman #21OPCC
Sleeman assessing pandemic for palliative care through Lewin's Unfreeze Change Refreeze model #21OPCC
mindtools.com/pages/article/…
mindtools.com/pages/article/…
What do we need:
1. Better integration across teams
2. Identify and tackle inequality (paper coming next wk) - COVID and #BlackLivesMatter movement has put it to the fore
3. Recognise/support aged care
4. Bereavement support
5. Collaboration (academic/policy/services) #21OPCC
1. Better integration across teams
2. Identify and tackle inequality (paper coming next wk) - COVID and #BlackLivesMatter movement has put it to the fore
3. Recognise/support aged care
4. Bereavement support
5. Collaboration (academic/policy/services) #21OPCC
Shoutout from @kesleeman for this @bmj_latest
essay from @Lucy_Selman
"Covid grief has cracked us open: how clinicians respond could reshape attitudes to bereavement"
bmj.com/content/374/bm #21OPCC
essay from @Lucy_Selman
"Covid grief has cracked us open: how clinicians respond could reshape attitudes to bereavement"
bmj.com/content/374/bm #21OPCC
Finally @kesleeman recommends reading the Marie Curie The Better End of Life Report 2021 #21OPCC
mariecurie.org.uk/policy/better-…
mariecurie.org.uk/policy/better-…
plz unroll @threadreaderapp
• • •
Missing some Tweet in this thread? You can try to
force a refresh