Welcome to the final set of tweetorials from @GoggleDocs A look at some of the interesting trials on hypertension from #ESCCongress
First up we're giving you some SSaSS!
No, not that, we are talking about salt and salt substitution!
What is the recommendation for daily sodium intake according to @American_Heart for healthy individuals?
The AHA recommends no more than 2300mgs salt per day and no more than 1500mgs in HTN…though many eat more than this…
So putting that into teaspoons of salt…
1/4 teaspoon salt = 575 mg sodium
1/2 teaspoon salt = 1,150 mg sodium
3/4 teaspoon salt = 1,725 mg sodium
1 teaspoon salt = 2,300 mg sodium
1/4 teaspoon salt = 575 mg sodium
1/2 teaspoon salt = 1,150 mg sodium
3/4 teaspoon salt = 1,725 mg sodium
1 teaspoon salt = 2,300 mg sodium
Low sodium diets are recommended in CCF, CKD and also been found to aid BP reduction …. but what about salt substitution…
Salt substitution aims to reduce sodium intake by replacing sodium with potassium salts
➡️ also has an added benefit (for some) of increasing potassium intake …one issue.. the more the potassium chloride used the more metallic the taste
➡️ also has an added benefit (for some) of increasing potassium intake …one issue.. the more the potassium chloride used the more metallic the taste
In this study, different percentages of KCl were tested to assess acceptability… upto 30% KCl substitution was reasonably acceptable.
clinicalhypertension.biomedcentral.com/articles/10.11…
clinicalhypertension.biomedcentral.com/articles/10.11…
The impact of this salt substitution on BP has been shown with metanalyses showing 5.5mmHg SBP and 2.4mmHg in DBP in hypertensive individuals…with benefit even seen in normotensive people
ahajournals.org/doi/10.1161/HY…
ahajournals.org/doi/10.1161/HY…

But what about impact on CVD and mortality? Well, not much data…
Stay tuned for a look to see whether this study was worth its salt...
So...nejm.org/doi/full/10.10… - The Salt Substitute and Stroke Study (SSaSS)
This study enrolled 20,995 people from 600 villages across rural China over 5 years to either 100% Nacl or 75% NaCl/25% KCl substitution
Inclusions
History of stroke or >60yrs old
History of ⬆️BP (>/= 160mmHg if untreated, >/= 140 if treated)
Exclusions
Contraindication to salt substitution, K+ sparing diuretic use, K+ supplement use or serious kidney disease, likely to live <6/12 or ate mostly outside the house
History of stroke or >60yrs old
History of ⬆️BP (>/= 160mmHg if untreated, >/= 140 if treated)
Exclusions
Contraindication to salt substitution, K+ sparing diuretic use, K+ supplement use or serious kidney disease, likely to live <6/12 or ate mostly outside the house
Primary outcome – stroke 🧠
Secondary outcome – MACE (non-fatal stroke, non-fatal ACS or CV mortality)🫀 and all cause mortality ☠️
Key safety outcome – hyperkalaemia (and also sudden death)
Secondary outcome – MACE (non-fatal stroke, non-fatal ACS or CV mortality)🫀 and all cause mortality ☠️
Key safety outcome – hyperkalaemia (and also sudden death)
Interesting to see ⬆️ percentage with uncontrolled hypertension, ⬇️ACEi use, M=F split and relatively ⬇️diabetes population
Nice data showing BP reduction over this trial period (mean FU 4.74yrs) and as expected reduced sodium excretion 

But we know this from previous trials and data… what about the important CV results….
Primary Outcome
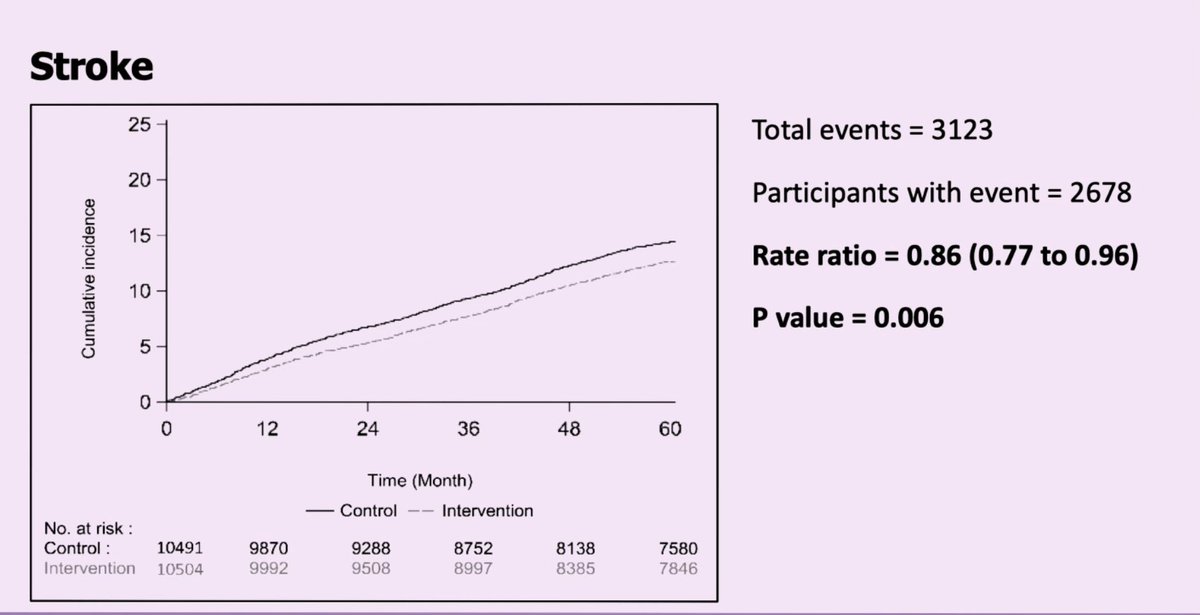
🧠⬇️13% rate of fatal or non-fatal stroke p = 0.006 [29.14 vs 33.65 events/1000 patient yrs] - no difference in non-fatal stroke
Secondary Outcomes
13% ⬇️MACE p<0.001
12% ⬇️Death from any cause p<0.001
13% ⬇️Death from vascular causes
30%⬇️Non-fatal ACS
🧠⬇️13% rate of fatal or non-fatal stroke p = 0.006 [29.14 vs 33.65 events/1000 patient yrs] - no difference in non-fatal stroke
Secondary Outcomes
13% ⬇️MACE p<0.001
12% ⬇️Death from any cause p<0.001
13% ⬇️Death from vascular causes
30%⬇️Non-fatal ACS
Some impressive findings of reduced stroke and further reductions in all cause mortality, death from vascular causes and non-fatal ACS with no real significant adverse events....
Rural Chinese population - can this be generalisable?
Potassium was not monitored serially throughout the trial (so hyperkalaemia potentially might have been missed) - though no major adverse event differences
Potassium was not monitored serially throughout the trial (so hyperkalaemia potentially might have been missed) - though no major adverse event differences
Do we need more data?
Can we generalize this to other areas?
Is this something that we should be advising now?
What does this mean for practical application?
Is this a chance for a population based intervention?
Can we generalize this to other areas?
Is this something that we should be advising now?
What does this mean for practical application?
Is this a chance for a population based intervention?
That's for you to answer. Based on this trial, I would...
So I ask you again… is this study worth its salt?
That’s all for now.
But do return as we continue our journey and STEP further into rural China with another blood pressure trial!
But do return as we continue our journey and STEP further into rural China with another blood pressure trial!
• • •
Missing some Tweet in this thread? You can try to
force a refresh