Don't miss the launch Monday of a new accredited tweetorial on optimizing duration of antiplatelet therapy after #ACS/#PCI, with expert author @mirvatalasnag leading us through the data. #ACCWIC @DrMarthaGulati @ShelleyZieroth @TYWangMD @Drroxmehran @aayshacader #cardiotwitter 

Watch here tomorrow a new accredited, serialized tweetorial on optimizing duration of antiplatelet therapy after ACS/PCI. Earn 0.5 CE/#CME credits: #physicians, #nurses, #pharmacists! Expert faculty @mirvatalasnag. #medtwitter @academiccme #cardiotwitter #FOAMed @CardioNerds
1) Welcome to a tweetorial on optimizing duration of antiplatelet tx after #ACS/#PCI! Accredited for 0.50 credits by @academiccme! I am @mirvatalasnag . Be sure to see prior tweetorials on this topic and still earn credit at cardiometabolic-ce.com/category/plate… 

2) This series is supported by educational grants from AstraZeneca, Bayer, Chiesi, and NovoNordisk and is intended for healthcare providers. Faculty disclosures are listed at cardiometabolic-ce.com/disclosures/.
Now let's start with a case!
Now let's start with a case!
3) Case summary: 85y woman with history of GI bleeding secondary to peptic ulcer disease 3 months ago, is admitted with an NSTEMI. She is hemodynamically stable and her baseline Hb is 10 g/dl. 

5) Since the patient is hemodynamically stable with TIMI III flow in her epicardial coronary arteries, we do not proceed with ad hoc PCI & opt to discuss options at the heart team meeting. What would you recommend as a revascularization option in this 85 year old?
a. CABG with no antiplatelet
b. CABG with single antiplatelet
c. Complex PCI with DAPT for 1 month
d. Complex PCI with DAPT for 6 months
PLEASE VOTE
b. CABG with single antiplatelet
c. Complex PCI with DAPT for 1 month
d. Complex PCI with DAPT for 6 months
PLEASE VOTE
6) At the heart team meeting, we agreed to proceed with an endoscopy to determine her risk for a future bleed. It revealed a healing duodenal ulcer and no active bleeding. As such, given her age and frailty, she was deemed too high risk for CABG & complex PCI was offered.
7) Angio Post-PCI
IVUS guided PCI of the Left Main, LAD and Left Circumflex using DK Crush technique with Proximal Optimization using a 4.5 NC balloon.
IVUS guided PCI of the Left Main, LAD and Left Circumflex using DK Crush technique with Proximal Optimization using a 4.5 NC balloon.

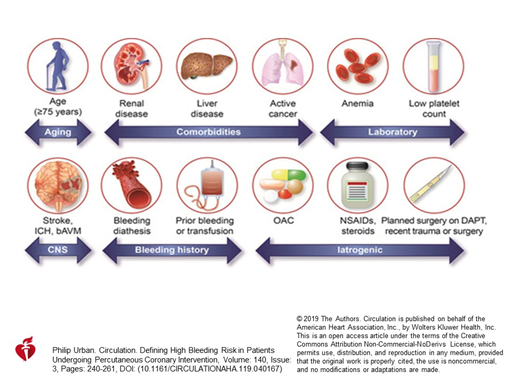
8) Her bleeding risk stems from age, anemia and prior bleeding. The decision to initiate DAPT and its duration needs to jointly evaluate and balance ischemic and bleeding risks. @AHAScience @escardio @ACCinTouch @SVRaoMD @DLBHATTMD @DrMauricioCohen @DocSavageTJU @JJheart_doc 
10) Please answer the poll and join us tomorrow for more discussion! @PCRonline @SCAI @apsic @Drroxmehran @CMichaelGibson @gabrielsteg @mamasmamas73 @DFCapodanno @vlgmrc @RenatoDLopes1 @cpcannon @GoggleDocs #FOAMed @VietHeartPA @Lross246
• • •
Missing some Tweet in this thread? You can try to
force a refresh