
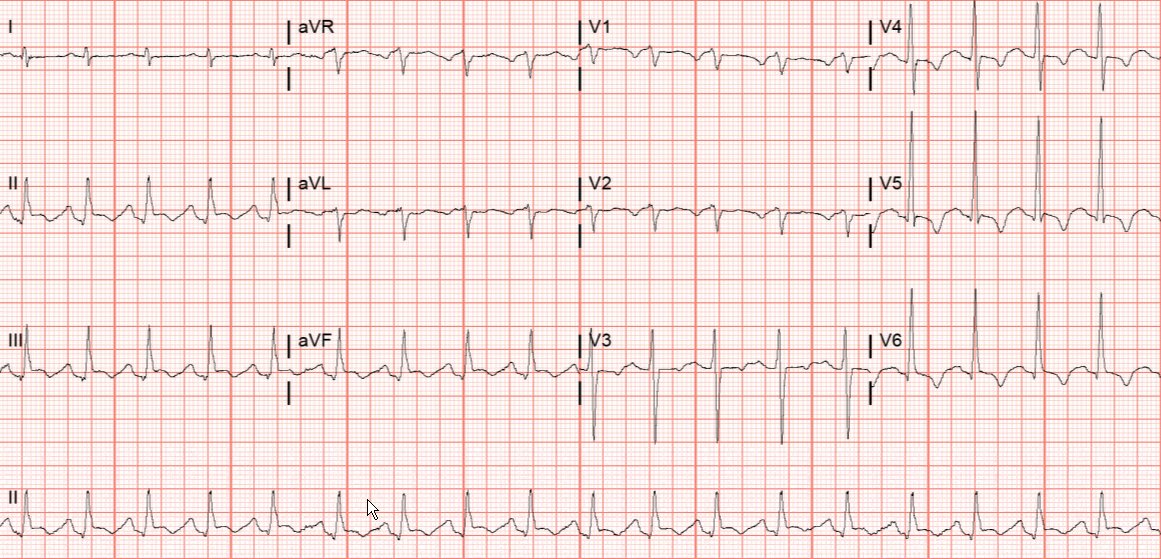
ICU stories (this story includes the answer to the quiz from yesterday): Young pt w PMH of HTN/HLD/DM2/CAD (stent of obtuse marginal) presented with chest/abd pain, N/V. Stat EKG (infero-lateral "changes"; ST elevation in inferior leads?): 
Emergent cath: "diffusely diseased LAD w stenosis 40%, non-dominant Cx with diffuse disease and stenosis <40%, widely patent OM stent, dominant RCA w diffuse disease and stenosis 50%. Pt did not have hemodynamically significant stenosis to explain symptoms and was admitted to CCU
... on nitro drip (for BP control). Next am, pt went into a wide-complex tachycardia that deteriorated in seconds to V fib. CPR started. Defib x1 back to SR. The post-ROSC ECG (that I posted yesterday) showed: 
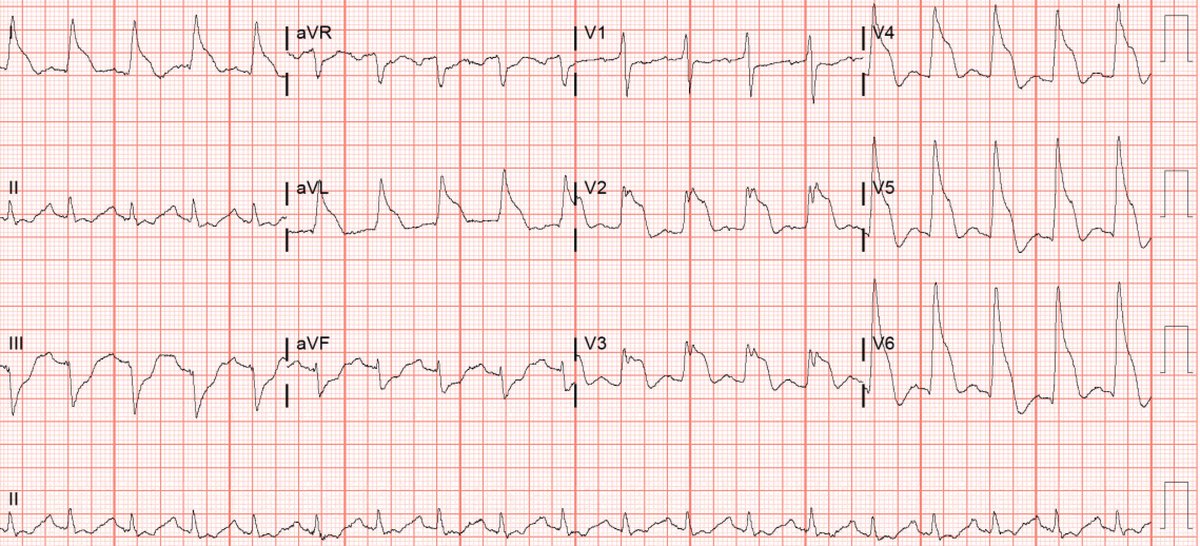
Really ugly looking ☝️, right? An ABG a few min post-ROSC showed normal K (4.1). Pt was intubated and underwent repeat emergent coronary angiogram that showed essentially same findings w the previous night's one. An IABP was placed
POCUS was performed 2 min after ICU arrival. This was the PLAX view (dilated LV; not much contractility in the anteroseptal and inferolateral walls):
PSAX:
4-chamber view (here the base seems to be contracting while the mid- and apical segments not much):
Subcostal:
And a more RV-focused view that was read as "normal" by the - later performed - "formal" echo:
Do you - especially the POCUS-savvy and the cardiologists - agree with the formal echo report that this RV is "normal"?
Next am, during rounds, I took a quick look with POCUS and it was already showing some recovery (subtle?). This was the 4-chamber view:
And the PSAX:
However, pt was oliguric w uop 10 cc/hour. Even though catecholamines are in general contraindicated in this scenario, I decided to try dobutamine drip and see if an ⬆️ in cardiac output would lead to ⬆️ uop. BTW, Vexus was 1. This was the LVOT VTI without and with dobutamine: 



LVOT VTI increased from ~ 10 to ~17. There was "contractile reserve". This was the impressive change in contractility shown in POCUS. The 4-chamber view:
And the PSAX:
Despite the increase in CO, the uop did not improve ☹️. After a couple of hours, I stopped the dobutamine drip. If something does not work, why keep doing it? This is Critical Care!
Three days later, LV/RV functions were back to normal. In retrospect, this was a case of Takotsubo cardiomyopathy!
Take-home messages:
1. These funny-looking ECGs for us, the not detail-oriented physicians who have an attention span of 5 sec, should be viewed as potentially secondary to MANY different pathologies. Obviously, we don’t want to miss a case of hyperkalemia, as ...
1. These funny-looking ECGs for us, the not detail-oriented physicians who have an attention span of 5 sec, should be viewed as potentially secondary to MANY different pathologies. Obviously, we don’t want to miss a case of hyperkalemia, as ...
... it would not be fun to code a hyperkalemic pt in the cath lab (kudos to @EM_RESUS for drawing attention to this scenario). On the other hand, AMI is a time-critical diagnosis (remember “shark fin” in ECG?) and needs to be ruled out ASAP (“time is muscle”).
2. I think Takotsubo cardiomyopathy is a great imitator and can present with a variety of cardiorespiratory or electrocardiographic pictures
3. I don’t know if it’s heresy - since I have not heard it being said that often - but I think it’s fair to say that Takotsubo
3. I don’t know if it’s heresy - since I have not heard it being said that often - but I think it’s fair to say that Takotsubo
cardiomyopathy can co-exist with coronary artery disease
4. POCUS provides a quick + easy way to assess if the therapeutic hemodynamic interventions really accomplish what they are supposed to (for example: do inotropes really increase CO?) and, if not, to be quickly discontinued
4. POCUS provides a quick + easy way to assess if the therapeutic hemodynamic interventions really accomplish what they are supposed to (for example: do inotropes really increase CO?) and, if not, to be quickly discontinued
5. It's OK to disagree with the formal echo report. The radiologists miss “things” in the x-rays and the CTs. Why do we expect the cardiologists to be flawless? The more experience you get with POCUS, the more you will find yourself questioning the echo reports. That’s fine as
...long as you use these cases as educational opportunities
Thanks for voting (yesterday) and reading today!
BTW, since all good Netflix series end with a final scene full of mystery, this was the patient’s ECG the next day 😊:
Thanks for voting (yesterday) and reading today!
BTW, since all good Netflix series end with a final scene full of mystery, this was the patient’s ECG the next day 😊:

#POCUS #ECHOFIRST #FOAMed #FOAMus #FOAMcc #IMPOCUS #MedEd #EMBound @ACEP_EUS @MetroHealth_EM @MH_EMultrasound @jminardi21 @ThinkingCC @RJonesSonoEM @jaffa_md @katiewiskar @kyliebaker888 @TomJelic @msiuba @siddharth_dugar
@thepocusatlas @NephroP @HeyDrNik @ICUltrasonica @khaycock2 @NickJohnsonMD @EmergenxyPhysic @DraHuerta09 @pocusmeded @POCUSClub @thepocusatlas @AmbrizMau @ecocritic_es @TaotePOCUS
@NephroGuy @VelezNephHepato @pocusfoamed @interconsulta @EmergencyEcho @echotalk @cianmcdermott @ImagenCardiaca @apenarEM @Porrose @chileanestesia @vaszochios @nickmmark @cjosephy @The_echo_lady @pdsalinas @GUH_ICU_Anaesth @EM_RESUS @KalagaraHari @UAlberta_Sono @EMUGs_
@UAlberta_ICU @UAB_Sono @MDBeni @MonaresTI @EMUGs_ @MedCriticaMex @critconcepts @pablitorf @MediCasos @ultra2ente @ACEP_EUS @grepmeded @ImagenCardiaca @RosenelliEM @FisioPocus @em_res @msenussiMD
• • •
Missing some Tweet in this thread? You can try to
force a refresh





