Developing safe & effective vaccine faster in a pandemic?
Helps but benefits only nations that can manufacture
Ensuring every region can make + administer vaccines as fast as rich nations?
Priceless.
Here's how via @JHSPH_CHS @JenniferNuzzo & me et al
bit.ly/3EwEA5n
Helps but benefits only nations that can manufacture
Ensuring every region can make + administer vaccines as fast as rich nations?
Priceless.
Here's how via @JHSPH_CHS @JenniferNuzzo & me et al
bit.ly/3EwEA5n

The COVID-19 pandemic has highlighted some strengths and some significant gaps and weaknesses in this global pandemic R&D and response ecosystem 2/
centerforhealthsecurity.org/our-work/publi…
centerforhealthsecurity.org/our-work/publi…
On one hand, pre-pandemic research into mRNA vaccines & public investment in COVID-19 vx R&D paid off hugely
Not one but several highly effective COVID-19 vaccines were developed, trialed & brought to market in 1 year
Previous record was 4 years (mumps) 2/
h/t @OurWorldInData
Not one but several highly effective COVID-19 vaccines were developed, trialed & brought to market in 1 year
Previous record was 4 years (mumps) 2/
h/t @OurWorldInData

Since being authorized for public use, more doses of COVID-19 vaccines were administered in 10 months (7 billion) than world usually makes in an entire year of all vaccines combined (~5 billion)
Recent pieces from @ChadBown + I outline how this happened3/
onlinelibrary.wiley.com/doi/epdf/10.11…
Recent pieces from @ChadBown + I outline how this happened3/
onlinelibrary.wiley.com/doi/epdf/10.11…
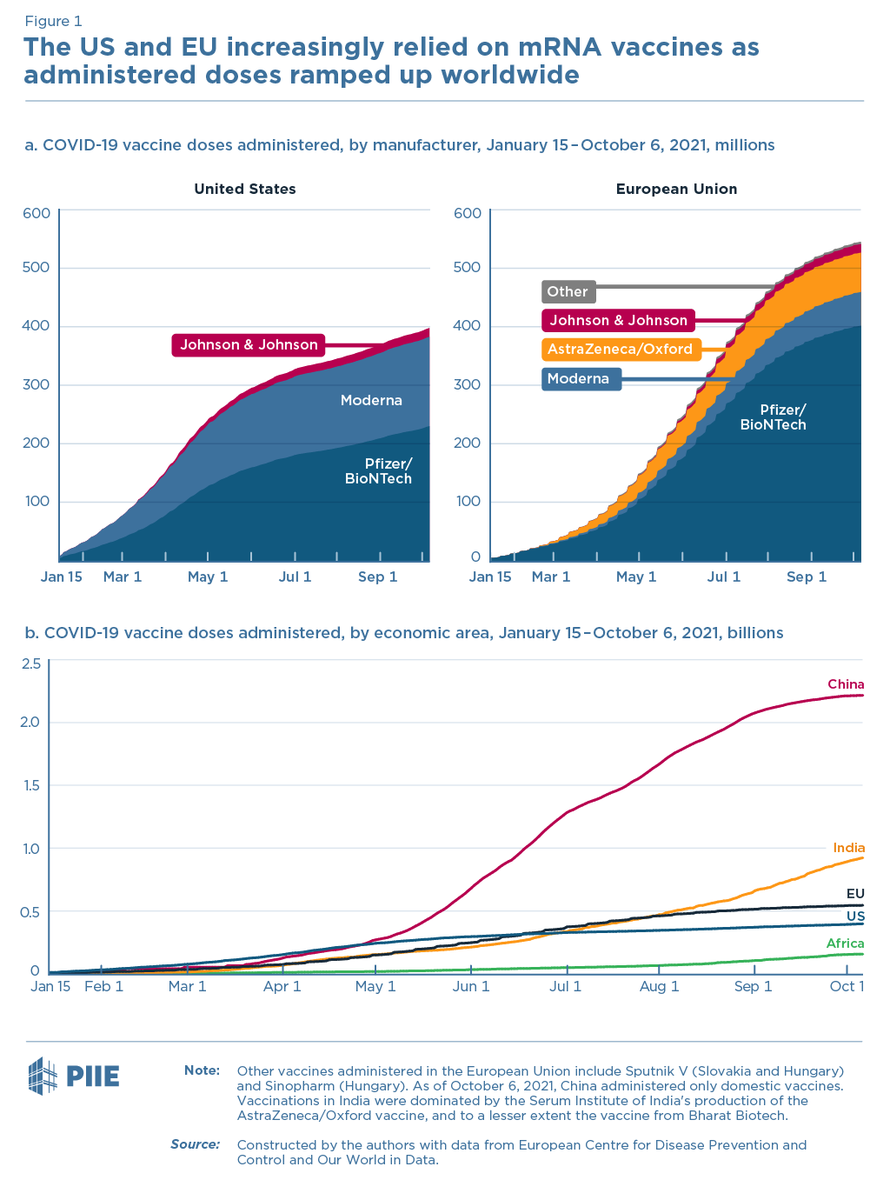
But, on the other hand, most LMICs haven't been able to acquire and administer enough COVID-19 vaccines
Just 10 nations account for nearly 75% of all COVID-19 vaccine doses administered worldwide—a statistic that has barely improved since the first authorization 4/
Just 10 nations account for nearly 75% of all COVID-19 vaccine doses administered worldwide—a statistic that has barely improved since the first authorization 4/

The cost of this vaccine inequity has been devastating
COVID deaths are increasing faster in regions + income groups that have had the lowest vaccination rates
COVID-19 deaths in 2021 are already 50%+ more than all of 2020 despite availability of multiple effective vaccines 5/
COVID deaths are increasing faster in regions + income groups that have had the lowest vaccination rates
COVID-19 deaths in 2021 are already 50%+ more than all of 2020 despite availability of multiple effective vaccines 5/

A major part of the problem has been what Nicki Lurie has called the “conductor-less orchestra"
Prior to pandemic, no global entities had mandate, financing, or capacity to initiate vaccine development or coordinate approval, manufacturing scale up, or ensure equitable access 6/
Prior to pandemic, no global entities had mandate, financing, or capacity to initiate vaccine development or coordinate approval, manufacturing scale up, or ensure equitable access 6/
COVAX tried to fill gap & had some success: raised US$9.8 billion, contracted for 4.3 billion vx doses & delivered 341 million doses to 144 countries (as of 10/10/21)
But COVAX has delivered less than a third of its year end goal + 40% of those doses were donated not purchased7/
But COVAX has delivered less than a third of its year end goal + 40% of those doses were donated not purchased7/
Fixing this problem isnt just a matter of thinking a/b what we could have done better w/COVAX
We must also anticipate how the COVID response has changed government, industry & civil society priorities for confronting future threats
We must navigate the world that COVID has made
We must also anticipate how the COVID response has changed government, industry & civil society priorities for confronting future threats
We must navigate the world that COVID has made
1. COVID-19 has illustrated to governments value of early and efficacious vaccines
Countries are creating new research initiatives & restoring manufacturing capacity
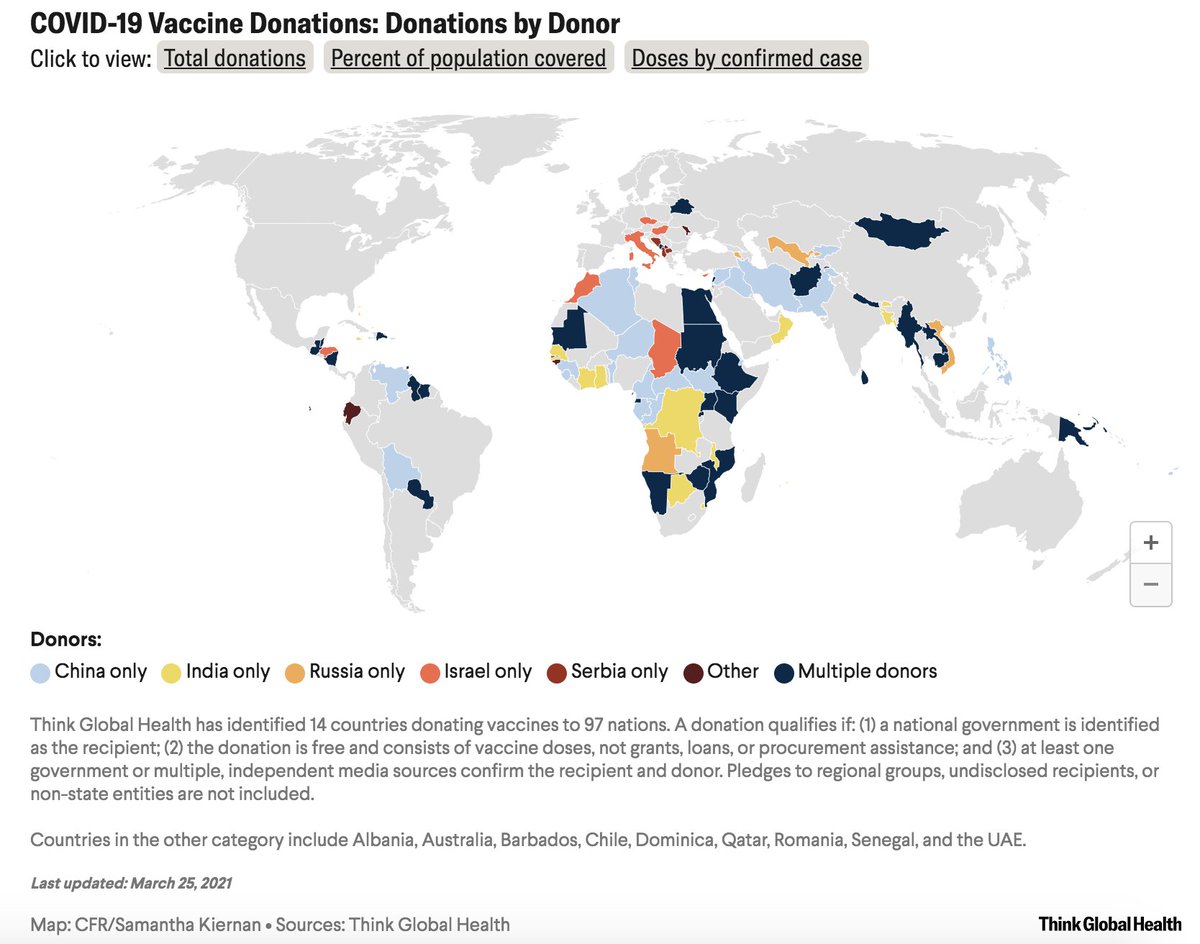
China hardly exported vaccines before pandemic & has now become largest exporter of COVID-19 vaccines so far 9/
Countries are creating new research initiatives & restoring manufacturing capacity
China hardly exported vaccines before pandemic & has now become largest exporter of COVID-19 vaccines so far 9/
2. COVID19 has shown pandemics are potentially profitable
Pfizer's COVID vaccine is most profitable pharmaceutical product in history
Record profits have drawn new vaccine makers into
market but made them less willing to enter into agreements w/equitable access requirements 10/
Pfizer's COVID vaccine is most profitable pharmaceutical product in history
Record profits have drawn new vaccine makers into
market but made them less willing to enter into agreements w/equitable access requirements 10/
3. COVID has shown governments won't share scarce vx supplies in a crisis w/out direct incentives to do so
This “me-first” approach to vaccines will dim nations’ enthusiasm for relying on global pooled procurement and access and benefit sharing arrangements in future crises 11/
This “me-first” approach to vaccines will dim nations’ enthusiasm for relying on global pooled procurement and access and benefit sharing arrangements in future crises 11/
4. COVID has shown global health cooperation can no longer be separated from geopolitical competition
Pandemics historically spurred more int'l cooperation. Not w/COVID
Cooperation on future pandemic R&D + response is more feasible w/regional partners or like-minded states 12/
Pandemics historically spurred more int'l cooperation. Not w/COVID
Cooperation on future pandemic R&D + response is more feasible w/regional partners or like-minded states 12/
Any future pandemic pathogen that emerges will do so in a world changed by and aware of these realities
To heed those lessons and to prevent the devastation of this crisis from repeating in next pandemic, my colleagues & I make detailed recommendations. Here are highlights: 13/
To heed those lessons and to prevent the devastation of this crisis from repeating in next pandemic, my colleagues & I make detailed recommendations. Here are highlights: 13/
First, establishing vaccine manufacturing capacity in LMICs is essential for future pandemic preparedness.
But, it should be viewed as a complement, not a near-term substitute, for also investing in economies of scale afforded by centralized production capacity 14/
But, it should be viewed as a complement, not a near-term substitute, for also investing in economies of scale afforded by centralized production capacity 14/
Our strategy outlines:
(a) mechanisms to facilitate technology transfer of potential pandemic vaccines & associated platforms;
(b) Flexible business models to make expanded manufacturing capacity viable between pandemics
(c)Investments in regional regulation & supply chains 15/
(a) mechanisms to facilitate technology transfer of potential pandemic vaccines & associated platforms;
(b) Flexible business models to make expanded manufacturing capacity viable between pandemics
(c)Investments in regional regulation & supply chains 15/
Second, it isn't feasible to make everything needed for vaccine administration in every country
Expanding vaccine manufacturing globally depends on reducing the export bans & barriers that have hindered cross-border trade of & investment in vaccines in this pandemic 16/
Expanding vaccine manufacturing globally depends on reducing the export bans & barriers that have hindered cross-border trade of & investment in vaccines in this pandemic 16/

Our strategy outlines:
(a) regional trade & investment agreements that would cover hub production of vaccines and vaccine-related inputs
(b) More global standardization of the specialized inputs (bags, filter, pumps etc) needed to make vaccines
(c) Supply chain transparency 17/
(a) regional trade & investment agreements that would cover hub production of vaccines and vaccine-related inputs
(b) More global standardization of the specialized inputs (bags, filter, pumps etc) needed to make vaccines
(c) Supply chain transparency 17/
Third, more financing is needed to end COVID-19 but it won't solve the procurement problems this pandemic revealed
Wealthy governments will always be able to either outbid a multilateral body or to seize locally produced vaccine doses in a pandemic
In COVAX, they did both 18/
Wealthy governments will always be able to either outbid a multilateral body or to seize locally produced vaccine doses in a pandemic
In COVAX, they did both 18/
The key to pandemic procurement is getting vaccine producing nations to participate in it. That means:
a. Trusted mechanisms established in advance;
b. COVAX has done a lot but concerns ab performance make it unlikely to be trusted in crisis
c. Regional mechanisms offer more hope
a. Trusted mechanisms established in advance;
b. COVAX has done a lot but concerns ab performance make it unlikely to be trusted in crisis
c. Regional mechanisms offer more hope
Read the whole report!
It has a lot useful to say on pre-pandemic R&D on prototype vaccine candidates, vaccine distribution + allocation, and post-market studies, and more
20/
centerforhealthsecurity.org/our-work/pubs_…
It has a lot useful to say on pre-pandemic R&D on prototype vaccine candidates, vaccine distribution + allocation, and post-market studies, and more
20/
centerforhealthsecurity.org/our-work/pubs_…
Many thx contributors & those who provided input @JHSPH_CHS @CFR_org incl @JenniferNuzzo @samckiernan @AmeshAA @RickABright @creynoldsdc @llborio @Yadav_supplychn @glassmanamanda @GaviSeth @JeremyFarrar @BhadeliaMD
Authors (most likely me) are responsible for opinions & errors
Authors (most likely me) are responsible for opinions & errors
Last, but far from least, many thanks also to my brilliant coauthors @MatthewPShearer @NatashaK_MSPH @noellehuhn @EmilyPondMPH
I would have credited you in the original thread if I were better at twitter sleuthing & had managed to discover your handles earlier! cc @JenniferNuzzo
I would have credited you in the original thread if I were better at twitter sleuthing & had managed to discover your handles earlier! cc @JenniferNuzzo
• • •
Missing some Tweet in this thread? You can try to
force a refresh