Restricted access to the NHS during the pandemic...
...the evidence and policies that led to excessively rationed healthcare provision in the UK.
Summary thread
1/18
RT pls
#YourNHSNeedsYou
#MedTwitter
thelancet.com/journals/lanep…
...the evidence and policies that led to excessively rationed healthcare provision in the UK.
Summary thread
1/18
RT pls
#YourNHSNeedsYou
#MedTwitter
thelancet.com/journals/lanep…
This paper was developed from a collaboration between primary, secondary, and public health care specialists. Its aim was to examine and highlight the policies that have led to restricted access to healthcare in the UK.
2/18
2/18
It shows:
1. No triage for suspected or confirmed COVID-19 cases
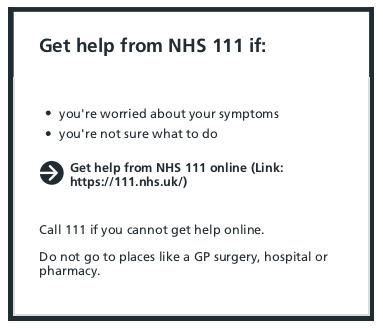
Despite WHO recommendation to triage all patients with this novel coronavirus, patients are told to NOT contact their GP and instead use an AUTOMATED, online patient-led triage system,... BUT only if concerned...
1. No triage for suspected or confirmed COVID-19 cases
Despite WHO recommendation to triage all patients with this novel coronavirus, patients are told to NOT contact their GP and instead use an AUTOMATED, online patient-led triage system,... BUT only if concerned...
And...
"Notably, thresholds for onward referral using these new and unproven triage systems were high [15]."
4/18
dx.doi.org/10.1136/bmjhci…
"Notably, thresholds for onward referral using these new and unproven triage systems were high [15]."
4/18
dx.doi.org/10.1136/bmjhci…
This is the advice for a 72 year old with persistent cough and fever for SEVEN days +/- silent hypoxia (as of 02/11/21):
5/18
5/18

"Equally concerning, the subsequent automated safety-net advice given to the patient included ‘how to manage breathlessness at home’ [[13]] – a practice that would have been inconceivable in 2019."
Accessed 02/11/21:
Accessed 02/11/21:

Beyond XS morbidity and mortality: "Any offsetting of the healthcare burden achieved by restricting access to clinical contact early on in the disease is lost when patients - albeit fewer in number - present more severely unwell further on in the course of the disease [7, 8, 9]"
2. Oxygen was also rationed.
Not just for COVID-19 patients but "for all adults treated in NHS hospitals" in England (Directive issued April 2020).
8/18
Not just for COVID-19 patients but "for all adults treated in NHS hospitals" in England (Directive issued April 2020).
8/18

Thankfully some localities identified these shortcomings and implemented virtual wards, where patients could be remotely monitored...
although the patient still needs to get through to healthcare first.
doi.org/10.1136/bmj.m2…
although the patient still needs to get through to healthcare first.
doi.org/10.1136/bmj.m2…
And in November 2020, the oximetry@home service started in England - providing access to oxygen monitoring for vulnerable patients. For those able to access it (still no clinical triage of cases), it looks like a life-saving and resource-saving intervention...
10/18
10/18

3. Bed capacity was also reduced.
Basic healthcare 'bed' capacity was reduced by 8% at the start of the pandemic, and remains 4% lower. (Source: NHS providers).
doi.org/10.1136/bmjope…
Basic healthcare 'bed' capacity was reduced by 8% at the start of the pandemic, and remains 4% lower. (Source: NHS providers).
doi.org/10.1136/bmjope…
The point:
"Waiting for patients to deteriorate and then providing care is neither effective nor efficient."
12/18
"Waiting for patients to deteriorate and then providing care is neither effective nor efficient."
12/18
"The public can still order a diagnostic test without clinical supervision, are still triaged through an automated or non-clinical pathway, and astonishingly, are still offered advice on how to manage breathlessness at home without ever having seen or spoken to a doctor or nurse"
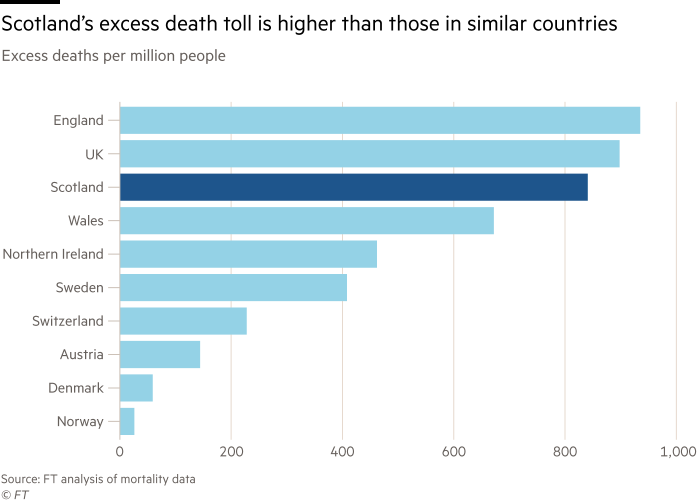
We must learn. To do so we must acknowledge that these practices are not consistent with basic medical principles, evidence, or clinical sense. There are currently 1400 additional deaths per week in the UK (the same as died in the entirety of 2019 from flu). Something is wrong.
The perception that we do not have the capacity to take on triage and follow-up of vulnerable patients with Covid is wrong...we do not have the capacity to NOT take it on...
15/18
15/18
"Without the essential access to healthcare we lose the opportunity to prevent disease progression and with it the opportunities to save lives, prevent disability, and to more effectively safeguard the NHS."
Politicians and non-clinical managers are not qualified to dictate clinical guidelines. Neither are they the right people to determine how limited resources are best used. We must insist on our standards, and where resources are not provided to do so, we must raise concerns
END
END
• • •
Missing some Tweet in this thread? You can try to
force a refresh