#
When government policy is not evidence based and is not in the interest of the patient...we must speak out.
🧵
#YourNHSNeedsYou #FBNHS
@dgurdasani1 @trishgreenhalgh @doctor_oxford @theAliceRoberts @mikegalsworthy @YourNHS2021 @NHSMillion @docrussjackson @PeoplesNHS @NurseSayNO
When government policy is not evidence based and is not in the interest of the patient...we must speak out.
🧵
#YourNHSNeedsYou #FBNHS
@dgurdasani1 @trishgreenhalgh @doctor_oxford @theAliceRoberts @mikegalsworthy @YourNHS2021 @NHSMillion @docrussjackson @PeoplesNHS @NurseSayNO
As panic gripped a rudderless nation, worst-case scenarios were being projected and simulations cast doom over the healthcare service’s ability to cope, the relative unknown fatality of this new infection foraging the globe loomed over our heads.
It was March 2020, and within this culture of fear, speculation became an acceptable basis for decision-making. Fear of needing to ration became rationing itself; protecting the NHS became failing to protect the people, and government policy suddenly became 'clinical guidelines’
There are a number of examples where executive directives and government policy (or sometimes lack thereof) retracted the standards of care we are used to implementing.
Sending patients back to care homes without being sure they were non-infectious was likely uncomfortable, to say the least.
Lowering our long-established target oxygen levels for when to start oxygen (and for many when to admit patients) was undoubtably difficult for many physicians, paramedics and nurses to endure.
Allowing patients with a respiratory infection to remain at home while breathless would also have been unfathomable just a year previously. And the list goes on.
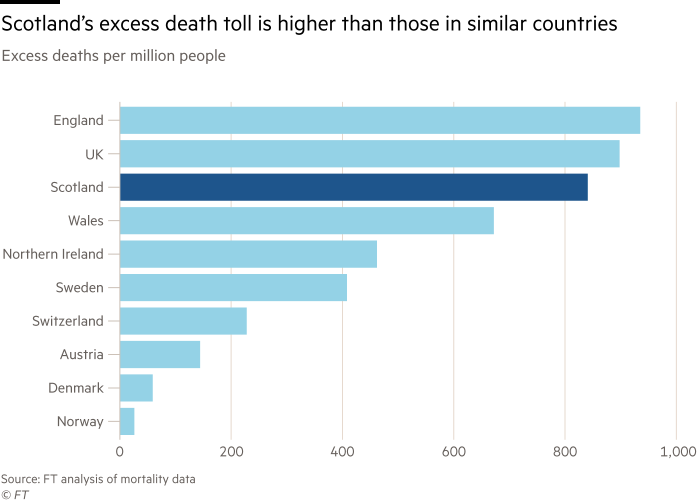
No doubt, there are pressing questions shared by public, victims and the traumatised healthcare staff: why? What happened? Why did our formidable healthcare service fail to prevent so many preventable deaths?
Perhaps the delay in lockdown, the lack of PPE, or simply the casual arrogance of leadership failed us. While the question as to the reason for the impotent response to the pandemic continues to consume our much needed emotional reserves, we must ask more reflective questions.
The pandemic rages on…killing more than three times the number of patients dying each year from pneumonia and tipping a normally unsafe bed occupancy level into a frankly dangerous state of affairs. So how should we respond?
At present we are fighting a pandemic during one of the most demanding winters in history. We are going into Winter with an NHS bed occupancy of 95%, a situation never before encountered. Primary care has also never faced such a mismatch between demands and available resources.
The threat is imminent. And the threat is the inaction taken by those charged with ensuring the health, safety, and liberty of the UK citizen.
So we must raise our voices and demand a more appropriate response to this national emergency. It is not business as usual. It cannot be business as usual. We must let the public know what is going on and force our leaders – local and national – to act now.
#SaveOurNHS
#SaveOurNHS
• • •
Missing some Tweet in this thread? You can try to
force a refresh