First, an observation. If you want to see what's actually going on in front of you, it's probably best to look through your eyes and not through your smart phone.
Social media tends to sensationalize the mundane and amplify voices with a particular point of view or agenda.
/2
Social media tends to sensationalize the mundane and amplify voices with a particular point of view or agenda.
/2

The ER docs I talked to last night felt the department was manageable. Comments ranged from 'steady but not crazy', to 'we're pretty good, not too bad at all'.
This kind of optimism from an ER doc is reassuring.
/3
This kind of optimism from an ER doc is reassuring.
/3

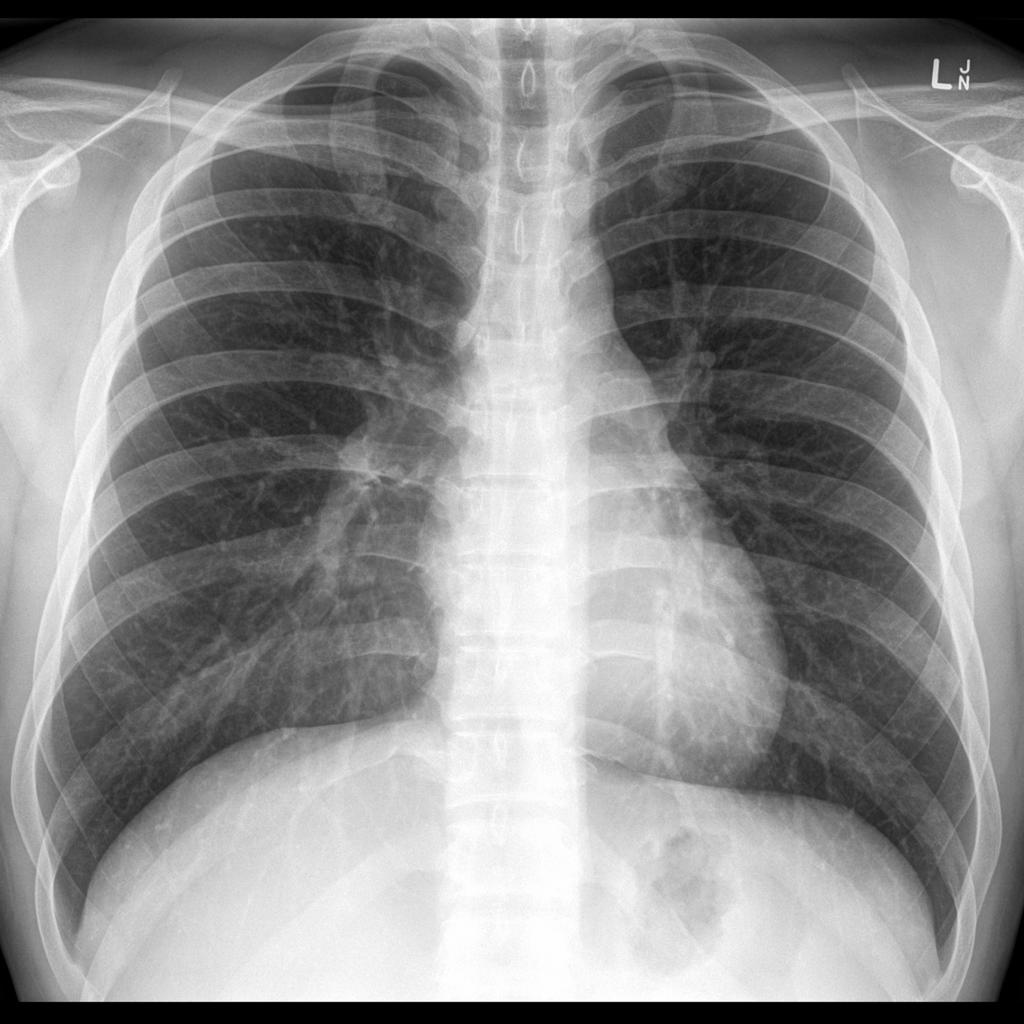
From an imaging point of view, there's been another shift.
The volume of imagining for COVID related illness is ticking down.
Not only are we seeing fewer chest X-rays, but we're seeing fewer CT scans to rule out COVID related strokes and pulmonary emboli.
/4
The volume of imagining for COVID related illness is ticking down.
Not only are we seeing fewer chest X-rays, but we're seeing fewer CT scans to rule out COVID related strokes and pulmonary emboli.
/4

I did an analysis of all chest X-rays over an 8 hour period. Of the 40 patients, 75% were completely normal or had disease unrelated to COVID, such as congestive heart failure.
/5
/5

The last 5% had moderate COVID-19 pneumonias. There were no severe pneumonias in the sample group.
/7
/7

The age breakdown was also very interesting.
Of the 40 patients, there were no school age children.
Among those with pneumonias, the vast majority were 60 yrs old or older.
Young adults comprised 20% of those with pneumonias, so they are not invulnerable to Omicron.
/8
Of the 40 patients, there were no school age children.
Among those with pneumonias, the vast majority were 60 yrs old or older.
Young adults comprised 20% of those with pneumonias, so they are not invulnerable to Omicron.
/8

The take home message is that, at least in our small corner of Ontario, things are calming down.
There is no longer the sense of urgency that we had 2 weeks ago.
We are not through this wave yet, but we can certainly see the shore, and it's in reach.
#Omicron @HRHospital
/9
There is no longer the sense of urgency that we had 2 weeks ago.
We are not through this wave yet, but we can certainly see the shore, and it's in reach.
#Omicron @HRHospital
/9

• • •
Missing some Tweet in this thread? You can try to
force a refresh