1) Tweet summary of the review on electrolyte disorders associated with Immunotherapy @CJASN @bdubNephro @nupuruppal @NephroMD cjasn.asnjournals.org/content/early/… 
2) Immunotherapy 101 for the Nephrologists- what do Immune checkpoint inhibitors and CAR-T therapy do? @onconephsociety @ASCO 



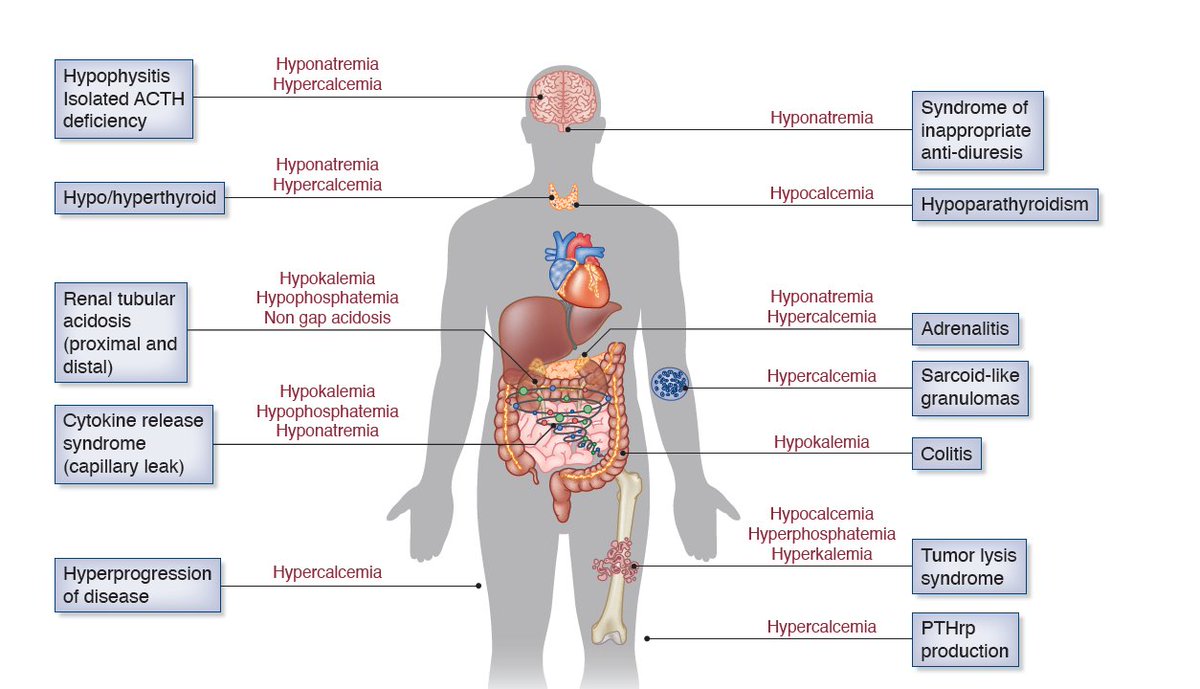
3) Hyponatremia- most common electrolyte abnormality noted with ICI therapy based on several studies, and in real life data pubmed.ncbi.nlm.nih.gov/34556301/ @Kidney_Int @renalmyeloma
4) SIAD is the most common mechanism as well described by @MegSise @BetterCallSeeth team. While adrenal causes are interesting- they are rarer. pubmed.ncbi.nlm.nih.gov/33374011/ @NDTsocial
5) Hyponatremia fairly common in CAR-T therapy as well as reported by @ShrutiGkidney and team @AJKDonline pubmed.ncbi.nlm.nih.gov/31973908/
6) Hypokalemia has been reported using ICIs and CAR-T. In a recent evaluation of the FAERS database, hypokalemia was the second most common electrolyte abnormality reported (18.71%) after hyponatremia @renalmyeloma. RTAs and colitis may be the two mechanism
7) Hypercalcemia associated with ICI therapy has some interesting mechanisms- sarcoid like granuloma formation, hyperprogression of disease, pthRP production by the ICI therapy and so forth- nicely summarized @NDTsocial pubmed.ncbi.nlm.nih.gov/33374000/ 

8) Hypocalcemia is very rare and proposed autoimmune hypoparathyroidism as the underlying mechanism. Initial studies had found high rates of this in RCTs analysis pubmed.ncbi.nlm.nih.gov/29762725/ @warpzone2017 @HerrmannMd
9) Hypophosphatemia--FAERS database showed that hypophosphatemia was reported in 3.36% of patients receiving a CTLA4 inhibitor, 1.49% of patients receiving a PD1i, CAR-T-- most common electrolyte abnormality, with 51% of experiencing severe hypophosphatemia @ShrutiGkidney
10)Hyperphosphatemia in patients receiving ICIs is not common across all classes-- perhaps best with Tumor Lysis syndrome associated with ICI therapy pubmed.ncbi.nlm.nih.gov/32274041/
11)Metabolic acidosis: The most frequent form of acidosis noted in association with the use of ICI is distal RTA.
12) RTA- 11 cases published thus far. Over 90% of the patients required steroid and alkali therapy. Kidney biopsies described in patients exposed to ICI with distal RTA even without AKI showed mild to moderate forms of interstitial nephritis.
13)Presently, there are no known patient-specific risk factors that may predispose a given patient to a particular ICI or CAR-T-related electrolyte/acid-base abnormality.
14) Limitations: We have summarized what is known about these agents from descriptions in case reports, case series and have extrapolated tissue pathologic findings, but the reader should be aware that early summaries may be prone to bias and confounding factors.
15) In summary, this is the first comprehensive review of all reported electrolyte dx with ICI therapy -- end tweetorial @threadreaderapp #unroll
• • •
Missing some Tweet in this thread? You can try to
force a refresh