This weeks #TenTweetNephJC makes us sad - does taking regular acetaminophen (paracetamol) cause hypertension?
Find out below in this rapid review of the Scottish trial, as we catch up on the #NephJC take on things 👇
Find out below in this rapid review of the Scottish trial, as we catch up on the #NephJC take on things 👇

What did I miss?
Observational trials suggest that acetaminophen increases BP, but (unlike NSAIDs) the widespread impression remains of a safe first-line therapy for chronic pain. The largest previous RCT had n=33.
Then PATH-BP dropped last month….
pubmed.ncbi.nlm.nih.gov/35130054/
Observational trials suggest that acetaminophen increases BP, but (unlike NSAIDs) the widespread impression remains of a safe first-line therapy for chronic pain. The largest previous RCT had n=33.
Then PATH-BP dropped last month….
pubmed.ncbi.nlm.nih.gov/35130054/
1 Tweet Methods
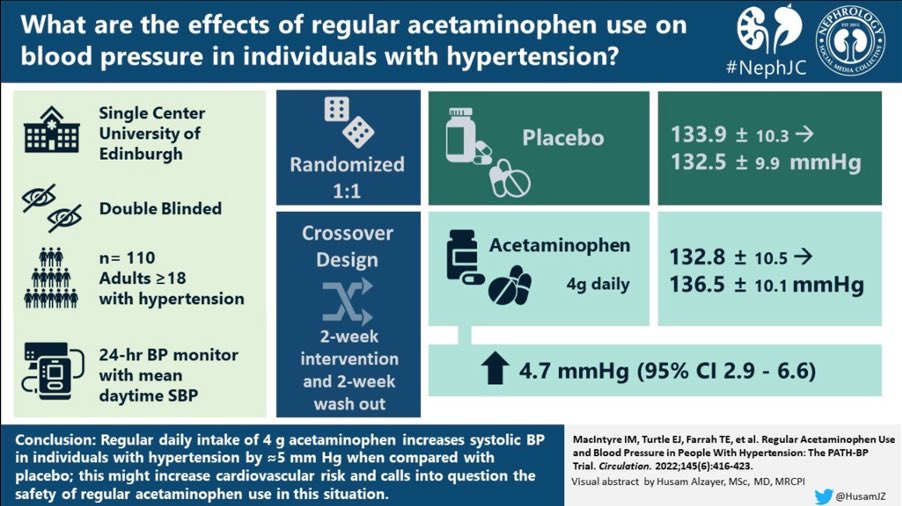
✔️ Single-centre, double-blind, placebo-controlled, crossover study
✔️ 4g/day acetaminophen (the standard UK dose) 🆚 placebo
✔️ 2 weeks active or placebo ➡️ 2 weeks washout ➡️ 2 weeks on opposite treatment
✔️ Primary outcome = change in 24 hour ambulatory BP
✔️ Single-centre, double-blind, placebo-controlled, crossover study
✔️ 4g/day acetaminophen (the standard UK dose) 🆚 placebo
✔️ 2 weeks active or placebo ➡️ 2 weeks washout ➡️ 2 weeks on opposite treatment
✔️ Primary outcome = change in 24 hour ambulatory BP
1 Tweet Results
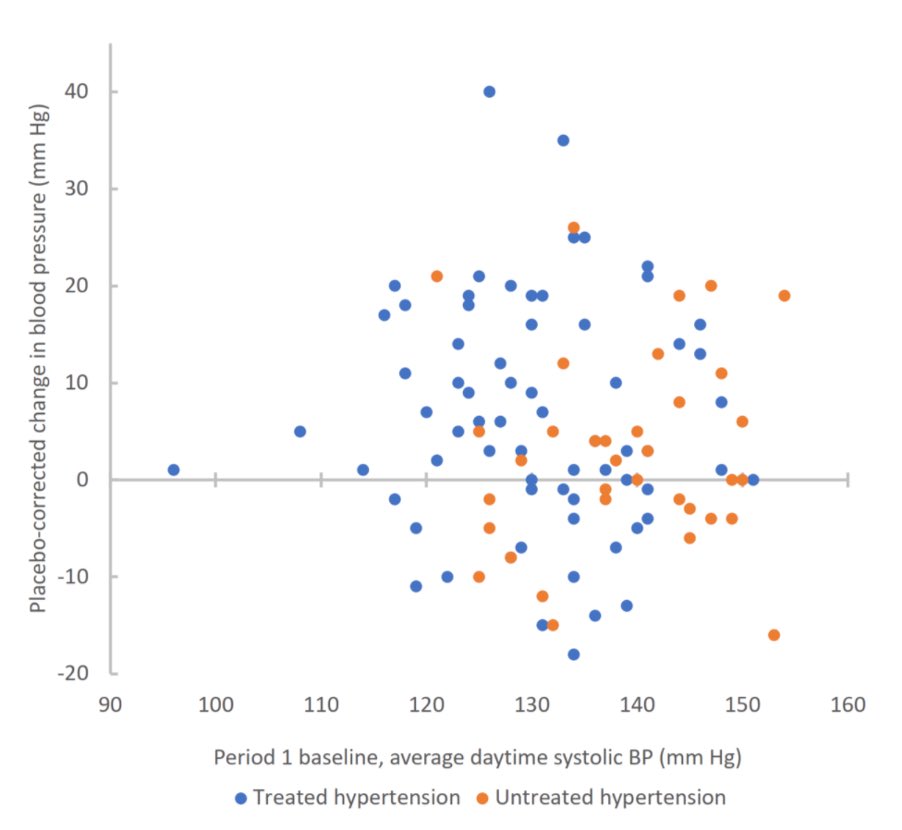
🔹103 patients
🔹 mean age 61
🔹 mean baseline BP 133/81, with 70% on at least one antihypertensive
Acetaminophen caused:
❗️Mean daytime systolic BP rise of 4.7 mmHg (p=<0.0001)
and
❗️Mean daytime diastolic BP rise of 1.6 mmHg (p=0.005)
🔹103 patients
🔹 mean age 61
🔹 mean baseline BP 133/81, with 70% on at least one antihypertensive
Acetaminophen caused:
❗️Mean daytime systolic BP rise of 4.7 mmHg (p=<0.0001)
and
❗️Mean daytime diastolic BP rise of 1.6 mmHg (p=0.005)
Give me something clever to say
“Given there’s a continuous relationship between BP & cardiovascular disease, & the use of paracetamol is so widespread, it is reasonable to hypothesise that the associated rise in BP could contribute to 1000s of additional CV events every year.”
“Given there’s a continuous relationship between BP & cardiovascular disease, & the use of paracetamol is so widespread, it is reasonable to hypothesise that the associated rise in BP could contribute to 1000s of additional CV events every year.”
Chat consensus?
1️⃣ Good trial, sad result
2️⃣ Can’t ignore impact of 4.7 mmHg rise in SBP on CV risk - it is a big deal
3️⃣ Our patients do need their pain managed: try non-pharmacological methods, but the ⬆️QoL from acetaminophen (or NSAIDs) can make side-effects worth the risk
1️⃣ Good trial, sad result
2️⃣ Can’t ignore impact of 4.7 mmHg rise in SBP on CV risk - it is a big deal
3️⃣ Our patients do need their pain managed: try non-pharmacological methods, but the ⬆️QoL from acetaminophen (or NSAIDs) can make side-effects worth the risk
Quote of the fortnight!
It’s again off topic and it’s again @captainchloride, but what a one tweet trial summary! Makes us feel bad for needing 10 tweets to do it….
It’s again off topic and it’s again @captainchloride, but what a one tweet trial summary! Makes us feel bad for needing 10 tweets to do it….
https://twitter.com/captainchloride/status/1501396447580725250?s=20&t=u4Gm39o4i0zdRmM35AV7hw
Final thoughts
✳️ Sometimes we have least data about the commonest meds - scary!
➡️ Up next - NephMadness chatter on 15/16 March, & then it’s a mechanistic study of diuretic resistance in CCF on 22/23 March. See you soon!
pubmed.ncbi.nlm.nih.gov/34529781/
Tweetorial by @jamiekwillows
✳️ Sometimes we have least data about the commonest meds - scary!
➡️ Up next - NephMadness chatter on 15/16 March, & then it’s a mechanistic study of diuretic resistance in CCF on 22/23 March. See you soon!
pubmed.ncbi.nlm.nih.gov/34529781/
Tweetorial by @jamiekwillows
• • •
Missing some Tweet in this thread? You can try to
force a refresh