What is your take on #vasodilators in acute #HeartFailure? The upcoming November issue of #EHJACVC will bring you a PRO/CON "Vasodilator therapy in acute heart failure revisited"
As our PRO paper was published in advanced access, a sneak preview Tweetorial below...
@EHJACVCEiC
As our PRO paper was published in advanced access, a sneak preview Tweetorial below...
@EHJACVCEiC
First some background...
Current @escardio guidelines state (IIb, B): "In patients with AHF and a systolic blood pressure (SBP) >110 mmHg, intravenous vasodilators may be considered as an initial therapy to improve symptoms and reduce congestion."
Only 1 flowchart has them in...
Current @escardio guidelines state (IIb, B): "In patients with AHF and a systolic blood pressure (SBP) >110 mmHg, intravenous vasodilators may be considered as an initial therapy to improve symptoms and reduce congestion."
Only 1 flowchart has them in...

So far, I consider this a fair recommendation... In hyper/normotensive pulmonary oedema, they might be helpful in some cases, with their main benefit a reduced need for (non-)invasive ventilation!
Beautiful (older) trial by Gad Cotter on this: thelancet.com/journals/lance…
Beautiful (older) trial by Gad Cotter on this: thelancet.com/journals/lance…
Our PRO viewpoint however is more a critique of this flowchart. Personally, I am really annoyed by this updated version in the guidelines, which carries the risk of increasing the already inappropriately high use of #inotropes or even worse #vasopressors... 

Great effort by @SVanhentenrijk to write this piece, discussing pathophysiology & reasons for vasodilators in AHF, explaining why we need trials in the RIGHT population (low cardiac output w increased systemic vascular resistance).
Super mentorship by @venumenon10 @WilsonTangMD
Super mentorship by @venumenon10 @WilsonTangMD
First, know your drugs, not all #vasodilators are alike...
Organic nitrates: mainly preload reduction, afterload at higher dose
Hydralazine: pure afterload reduction
Nitroprusside: balanced preload/afterload reduction (my favorite in AHF)
Organic nitrates: mainly preload reduction, afterload at higher dose
Hydralazine: pure afterload reduction
Nitroprusside: balanced preload/afterload reduction (my favorite in AHF)

If You remember 1 thing from our paper, let it be: "SBP = awful marker of #afterload or ventriculo-arterial coupling, making it pretty useless in decision to employ #vasodilators"
If anything vasodilators work best in patients with LOW SBP: link.springer.com/article/10.100… @AlexMebazaa
If anything vasodilators work best in patients with LOW SBP: link.springer.com/article/10.100… @AlexMebazaa
Why is this? Need pressure-volume loops in here:
In preserved CO/SV (steep Ees~contractility), reducing afterload (Ea) has little impact on stroke volume (SV), which is already high. However, marked impact on BP (preload dependency!)
In preserved CO/SV (steep Ees~contractility), reducing afterload (Ea) has little impact on stroke volume (SV), which is already high. However, marked impact on BP (preload dependency!)

In low CO/SV (more flat Ees) however, despite lower SBP to start from, impact of reducing afterload (Ea) on BP is minimal, because lower vascular tonus is compensated by a massive increase in SV (afterload dependency!) 

Thus, as the Great Guyton has teached us:
Blood pressure is not the same as #Perfusion
So we need to employ vasodilators in patients who are very vasoconstricted with low #CardiacOutput, typically w low SBP, low #PulsePressure & preserved MAP
90/70 mmHg means MAP=77 mmHg!!!
Blood pressure is not the same as #Perfusion
So we need to employ vasodilators in patients who are very vasoconstricted with low #CardiacOutput, typically w low SBP, low #PulsePressure & preserved MAP
90/70 mmHg means MAP=77 mmHg!!!

If you have understood this well, who gets vasodilator therapy from you?
Let's give it some time to reflect... Will come up with the answer tomorrow!
We finish this perspective w indications for which vasodilators seem as good as their alternatives (diuretics, inotropes, vasopressors mechanical support) for which the line of evidence is thin as well.
We finish this perspective w indications for which vasodilators seem as good as their alternatives (diuretics, inotropes, vasopressors mechanical support) for which the line of evidence is thin as well.
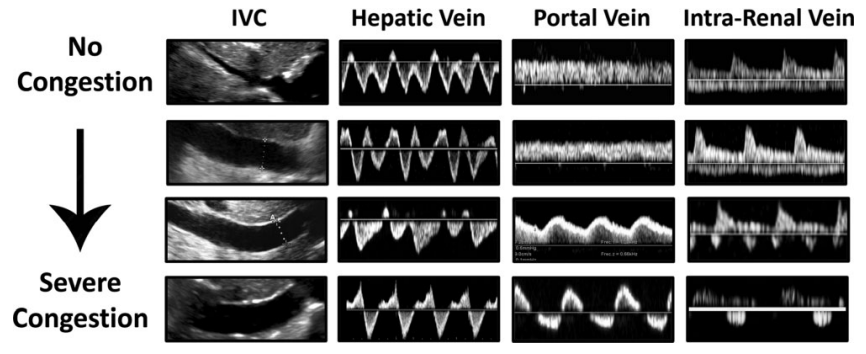
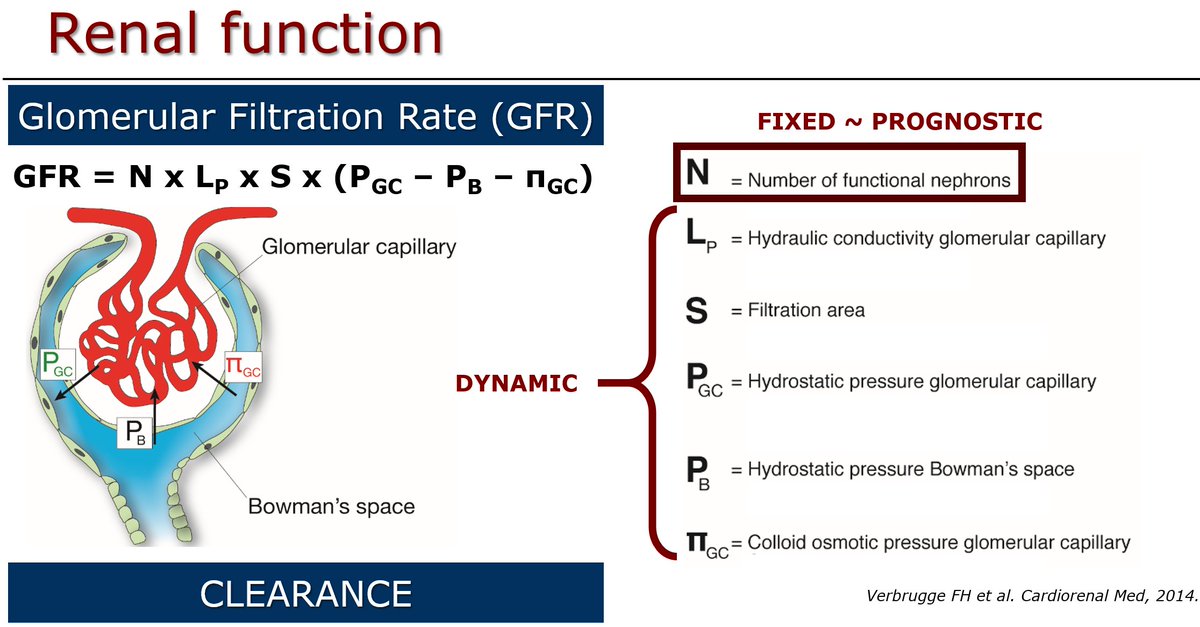
✅Optimise renal perfusion to enhance decongestion
✅Improve perfusion to prevent end-organ damage
✅Enabling early optimization of disease-modifying treatments (switch from IV nitroprusside to oral sac/val!)
✅Reduce surgical risk by reducing lung water & optimized hemodynamics
✅Improve perfusion to prevent end-organ damage
✅Enabling early optimization of disease-modifying treatments (switch from IV nitroprusside to oral sac/val!)
✅Reduce surgical risk by reducing lung water & optimized hemodynamics
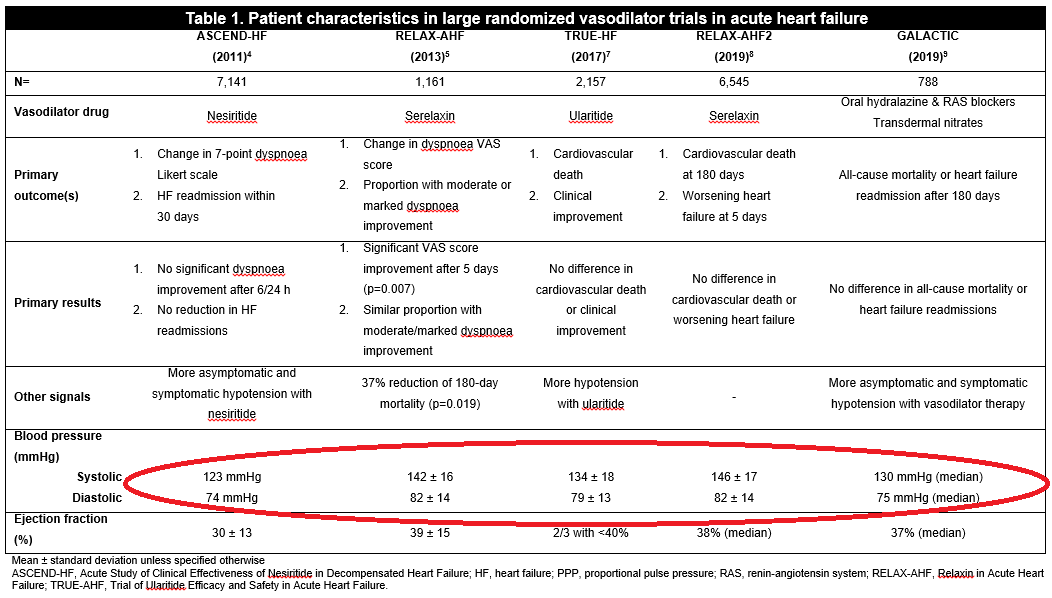
The CON party, will undoubtedly point towards failing trials with vasodilators in AHF, but look who they recruited, this is no low output #Heartfailure! 
• • •
Missing some Tweet in this thread? You can try to
force a refresh