Radiotherapy for renal cell carcinoma: current status and future directions
#RadOnc #kcsm #KidneyCancer @ASTRO_org @ESTRO_RT @ARRO_org @RadoncUh
Thread🧵

#RadOnc #kcsm #KidneyCancer @ASTRO_org @ESTRO_RT @ARRO_org @RadoncUh
Thread🧵

Thanks to @_ShankarSiva @DrAlexLouie @rob_uzzo @uretericbud @whallradonc @LPonsky @LeilaTchelebi for improving quality of this talk.
Thanks to @AmarUKishan @UCLA for invite to present.
Thanks to @AmarUKishan @UCLA for invite to present.
https://twitter.com/AmarUKishan/status/1598671748383531008
For reference, kidney cancer staging is here.
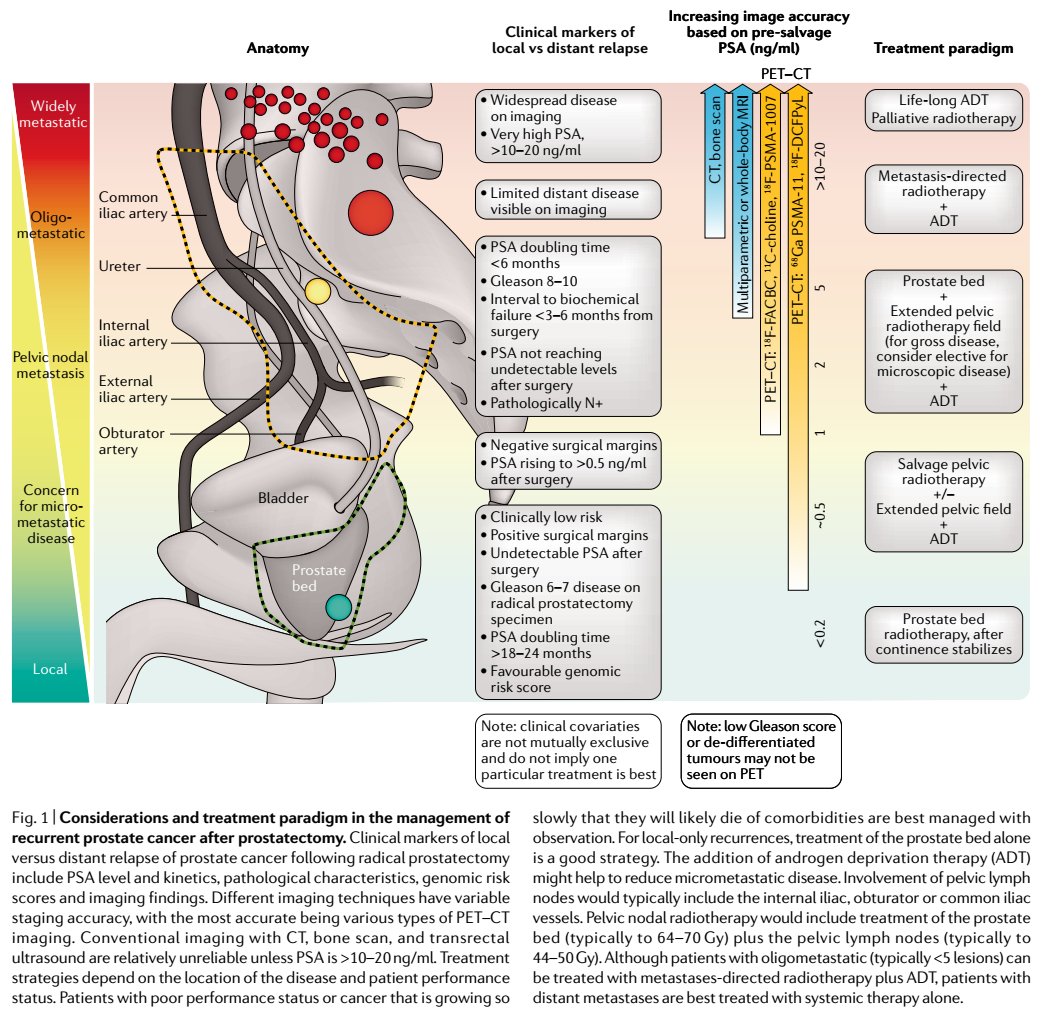
Currently, role of #radonc is for smaller cancers (eg, T1a/b, some T2) and metastatic disease.
Currently, role of #radonc is for smaller cancers (eg, T1a/b, some T2) and metastatic disease.
https://twitter.com/NicholasZaorsky/status/1590869044286357504
Kidney cancer used to be a clinical dx w symptoms, and it has evolved to become a radiographic dx wo symptoms.
Small renal masses (SRMs) are common today, akin to PSA-detected low-risk prostate cancers diagnosed in the 1990s.


Small renal masses (SRMs) are common today, akin to PSA-detected low-risk prostate cancers diagnosed in the 1990s.



The findings from a randomized trial in the 1980s led to a dark age of radiation therapy for kidney cancer. 



A meta-analysis of prospective (*actually retrospective) research served as an echo chamber, to suggest that radiotherapy for kidney cancer does not work.
@Annals_Oncology @myESMO
annalsofoncology.org/article/S0923-…
@Annals_Oncology @myESMO
annalsofoncology.org/article/S0923-…

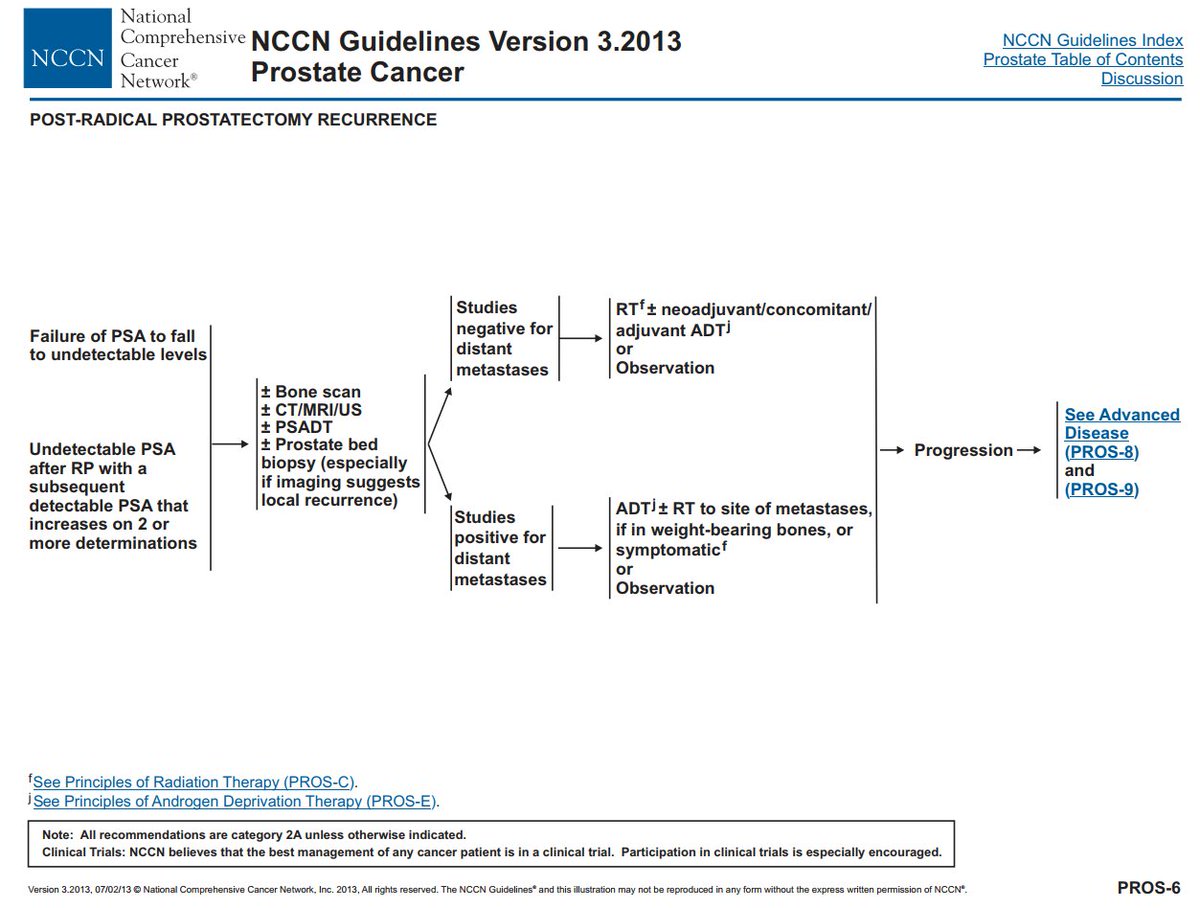
In 2013, @NCCN guidelines did not mention #radonc, except to say that radiation therapy had no role in the adjuvant setting. Meanwhile, partial nephrectomy (vs radical nephrectomy) become the most popular treatment approach.
jamanetwork.com/journals/jamas… @JAMASurgery @NCDB


jamanetwork.com/journals/jamas… @JAMASurgery @NCDB



Work from @uretericbud showed importance of competing risk of death.
CKD has been recognized as a major driver of other-cause mortality.
pubmed.ncbi.nlm.nih.gov/19933918/
nejm.org/doi/full/10.10…
pubmed.ncbi.nlm.nih.gov/20483451/
@JCO_ASCO @NEJM @TheLancetOncol



CKD has been recognized as a major driver of other-cause mortality.
pubmed.ncbi.nlm.nih.gov/19933918/
nejm.org/doi/full/10.10…
pubmed.ncbi.nlm.nih.gov/20483451/
@JCO_ASCO @NEJM @TheLancetOncol




Next, @_ShankarSiva led #radonc to re-introduce use of radiotherapy for kidney cancer.
The mechanism of cell death with high doses per fraction (>5-8 Gy/fx) is different than low doses per fraction (2 Gy/fx, similar to 1980s trial), and it seems to be effective for RCC.



The mechanism of cell death with high doses per fraction (>5-8 Gy/fx) is different than low doses per fraction (2 Gy/fx, similar to 1980s trial), and it seems to be effective for RCC.




#RadOnc physicians were already using SBRT for metastatic disease for many other cancers, so why not expand its use for primary and metastatic RCC?
https://twitter.com/NicholasZaorsky/status/1352264313227022337
When evaluating SBRT for metastatic disease from kidney cancer, local control is 90% and grade 3+ toxicity is 1%.
https://twitter.com/NicholasZaorsky/status/1149750368299036673
For primary kidney cancer, SBRT/SABR has many benefits over surgery, cryotherapy, and radiofrequency ablation.
Thanks to @_ShankarSiva for establishing the IROCK consortium.


Thanks to @_ShankarSiva for establishing the IROCK consortium.



From IROCK, for T1 RCC, we know that local control is 95%, grade 3+ toxicity is 0%, and impact on eGFR is relatively limited.
pubmed.ncbi.nlm.nih.gov/29266183/
pubmed.ncbi.nlm.nih.gov/32562838/
pubmed.ncbi.nlm.nih.gov/36400098/



pubmed.ncbi.nlm.nih.gov/29266183/
pubmed.ncbi.nlm.nih.gov/32562838/
pubmed.ncbi.nlm.nih.gov/36400098/




These results are consistent with a meta-analysis of SBRT for primary RCC.




https://twitter.com/NicholasZaorsky/status/1144586761961648129




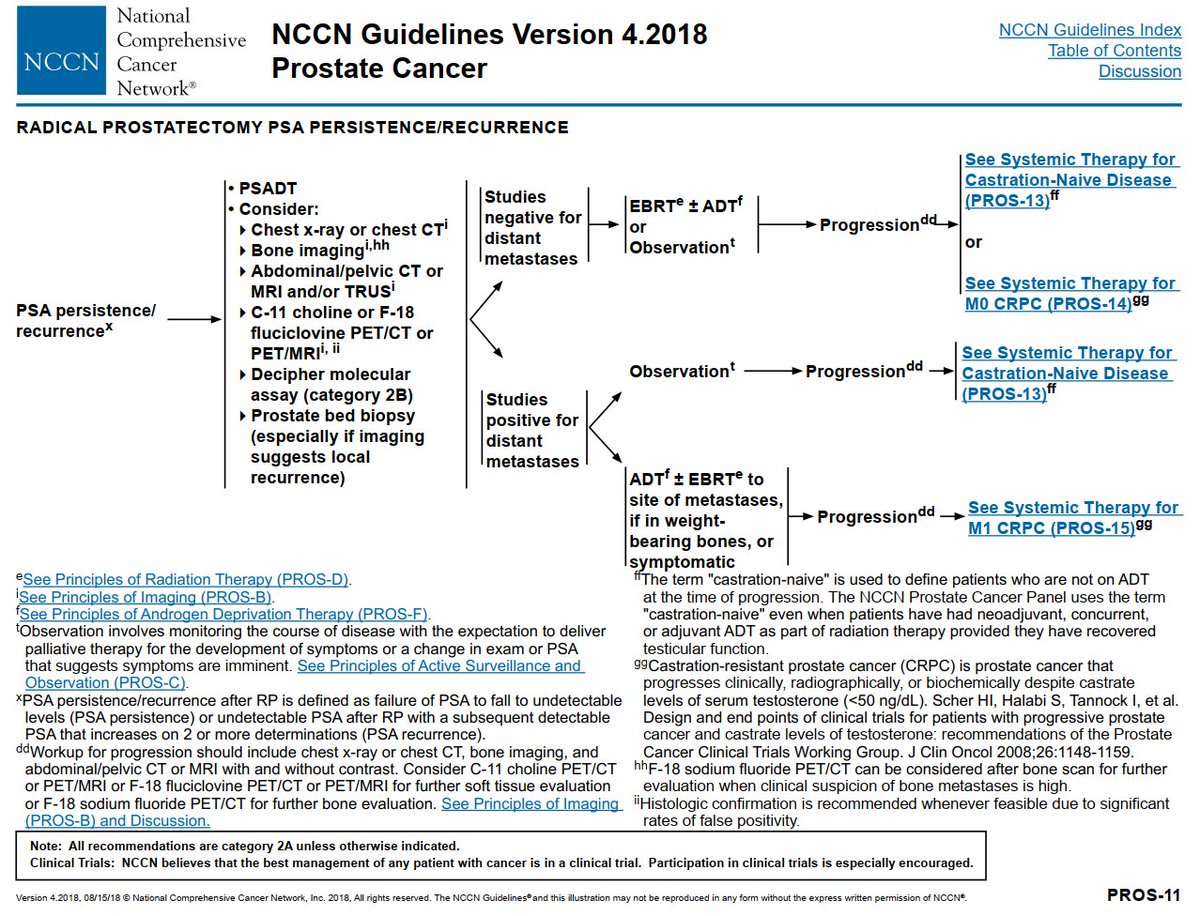
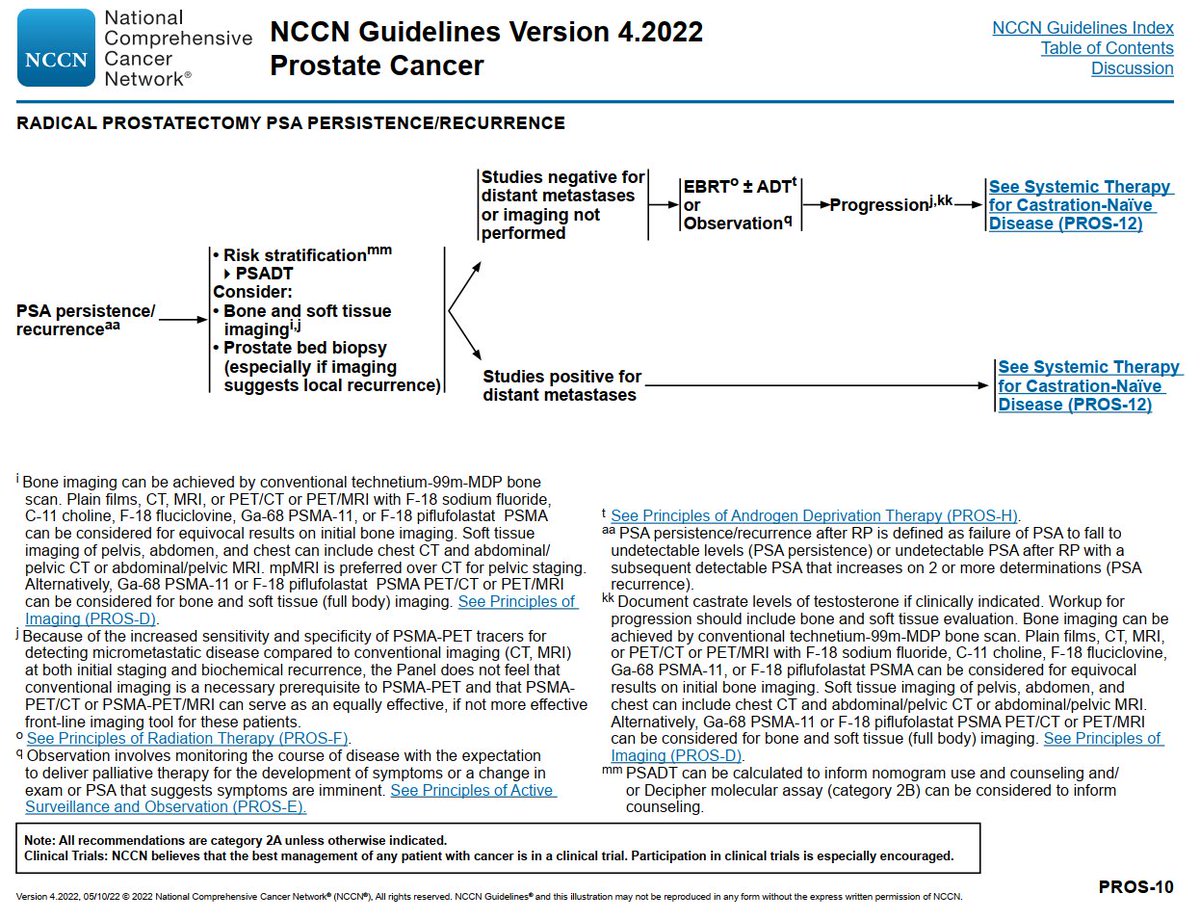
The 2020s are a new era for #radonc in @NCCN guidelines
@ASCO
dailynews.ascopubs.org/do/sabr-renal-…

@ASCO
dailynews.ascopubs.org/do/sabr-renal-…


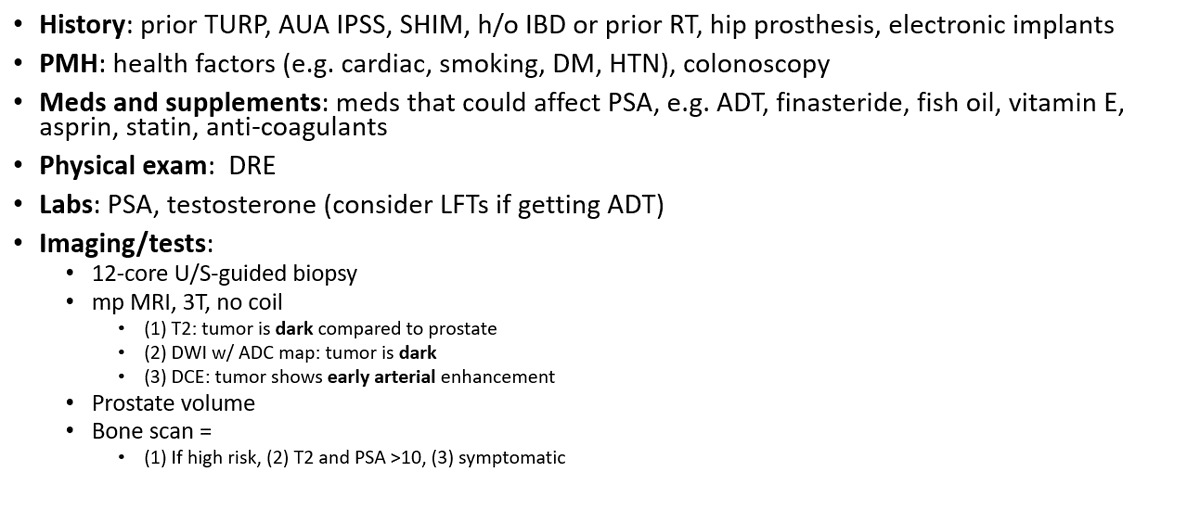
For a #radonc physician who plans to treat a patient with SBRT for primary RCC, what are the practical aspects of CT simulation?
@ARRO_org
@RadiumSociety is working on formal guidelines
@DrPaulNguyen @BrianJDavisMDPh @TimShowalter1 @MutlaySayan


@ARRO_org
@RadiumSociety is working on formal guidelines
@DrPaulNguyen @BrianJDavisMDPh @TimShowalter1 @MutlaySayan



For a #radonc physician who plans to treat a patient with SBRT for metastatic RCC, see the @ASCO guidelines: pubmed.ncbi.nlm.nih.gov/35728020/
Thanks for opportunity to collaborate, @KimrynRathmell @TiansterZhang @eric_facs @MattMilowsky.

Thanks for opportunity to collaborate, @KimrynRathmell @TiansterZhang @eric_facs @MattMilowsky.


#RadOnc plays a crucial role in tx of metastatic RCC.
Work from @ChadTangMD @PrajnanDasMD @MDAndersonNews: definitive RT in lieu of systemic tx for oligometastatic RCC.
pubmed.ncbi.nlm.nih.gov/34717797/
@TheLancetOncol
Work from @ChadTangMD @PrajnanDasMD @MDAndersonNews: definitive RT in lieu of systemic tx for oligometastatic RCC.
pubmed.ncbi.nlm.nih.gov/34717797/
@TheLancetOncol

SBRT is also an option for patients receiving TKI
Work from @DrPatCheung et al:
pubmed.ncbi.nlm.nih.gov/34399998/
See editorial from @_ShankarSiva @piet_ost @MichaelStaehler:
pubmed.ncbi.nlm.nih.gov/34563413/
@EUplatinum


Work from @DrPatCheung et al:
pubmed.ncbi.nlm.nih.gov/34399998/
See editorial from @_ShankarSiva @piet_ost @MichaelStaehler:
pubmed.ncbi.nlm.nih.gov/34563413/
@EUplatinum



IMO, TKIs should be held during RT.
In all of oncology, for every cancer where oncologists have combined RT + TKIs, there is never an improvement in survival, only worse toxicity.
In all of oncology, for every cancer where oncologists have combined RT + TKIs, there is never an improvement in survival, only worse toxicity.
https://twitter.com/nicholaszaorsky/status/1410269466454265867?lang=en
What is the future of #radonc for kidney cancer?
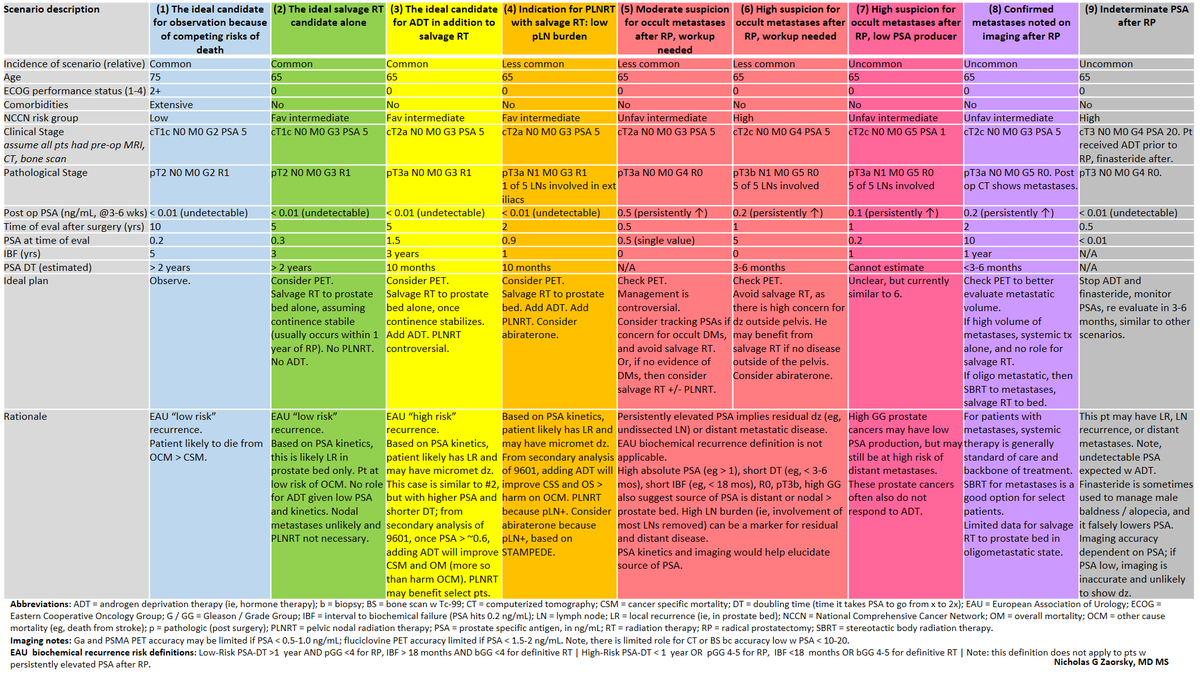
Here are some current unknowns and challenges for primary RCC.
In many ways, tx options and dogma for T1-2 RCC today are similar to localized prostate ca from 1990s.
We need a ProtecT for localized RCC.

Here are some current unknowns and challenges for primary RCC.
In many ways, tx options and dogma for T1-2 RCC today are similar to localized prostate ca from 1990s.
We need a ProtecT for localized RCC.


A core issue with metastatic cancer has been prognostication.
Physicians do not know which patients will progress rapidly, and have trouble selecting txs.
Our group has been working on improving prognostication for metastatic dz:
Physicians do not know which patients will progress rapidly, and have trouble selecting txs.
Our group has been working on improving prognostication for metastatic dz:
https://twitter.com/NicholasZaorsky/status/1418374866076672002
There are several ongoing randomized controlled trials in #radonc for RCC, eg FASTRACK I-II, RAPPORT from @_ShankarSiva 





Two great trials for SBRT to the primary tumor in the setting of metastatic dz:
CYTOSHRINK from @lalaniMD
ascopubs.org/doi/abs/10.120…
NRG GU 012 / SAMURAI from @whallradonc @DrRanaMcKay @PBarataMD @HimanshuNagarMD @ChadTangMD @_ShankarSiva @CGlideHurst @wandering_gu @NRGonc

CYTOSHRINK from @lalaniMD
ascopubs.org/doi/abs/10.120…
NRG GU 012 / SAMURAI from @whallradonc @DrRanaMcKay @PBarataMD @HimanshuNagarMD @ChadTangMD @_ShankarSiva @CGlideHurst @wandering_gu @NRGonc


Tx of the primary in setting of metastatic cancer has been area of controversy.
The pts derive most benefit:
1, low volume mets (eg, STAMPEDE, w tx to mets), and
2, get SBRT (not surgery)
RCC may fit the criteria.
@PCaParker @Prof_Nick_James @mattsydes
The pts derive most benefit:
1, low volume mets (eg, STAMPEDE, w tx to mets), and
2, get SBRT (not surgery)
RCC may fit the criteria.
@PCaParker @Prof_Nick_James @mattsydes
https://twitter.com/jryckman3/status/1552019701156429824
In summary, here are the current status and future directions of #radonc for kidney cancer.
@ASTRO_org @ESTRO_RT
@ASTRO_org @ESTRO_RT

• • •
Missing some Tweet in this thread? You can try to
force a refresh