1/My hardest #tweetorial yet! Are you up for the challenge?
How stroke perfusion imaging works!
Ever wonder why it’s Tmax & not Tmin? Do you not question & let RAPID read the perfusion for you? Not anymore!
#stroke #neurotwitter #neurorad #meded #FOAMed #radtwitter #medtwitter
How stroke perfusion imaging works!
Ever wonder why it’s Tmax & not Tmin? Do you not question & let RAPID read the perfusion for you? Not anymore!
#stroke #neurotwitter #neurorad #meded #FOAMed #radtwitter #medtwitter

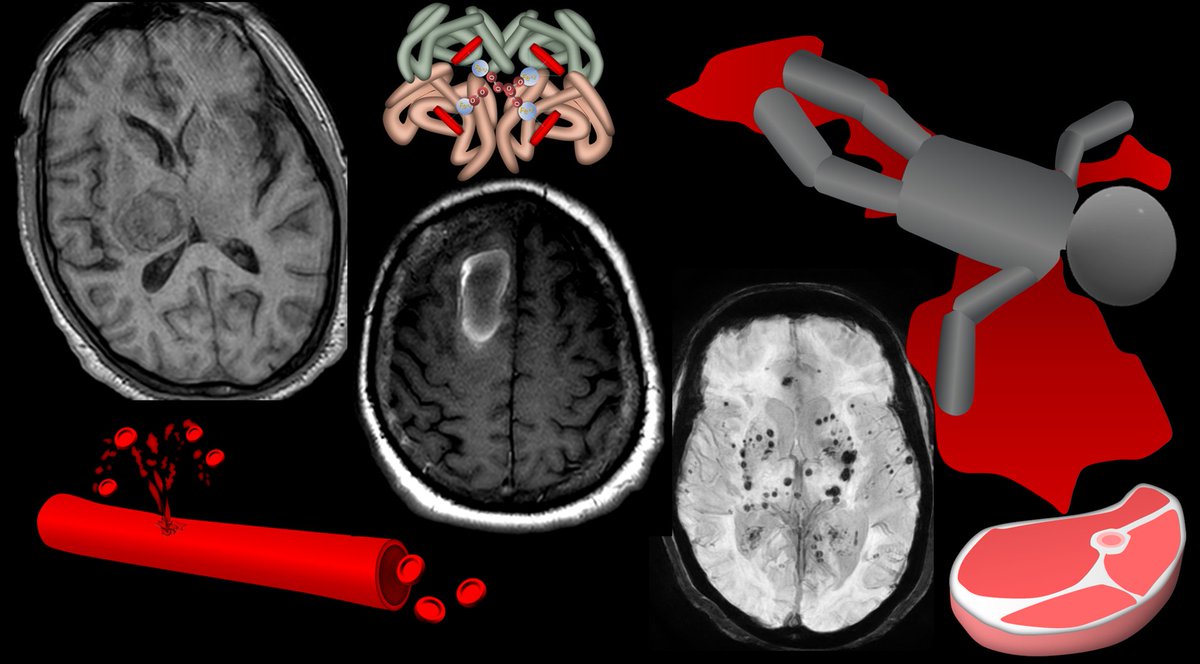
2/Perfusion imaging is based on one principle: When you inject CT or MR intravenous contrast, the contrast flows w/blood & so contrast can be a surrogate marker for blood. This is key, b/c we can track contrast—it changes CT density or MR signal so we can see where it goes 

3/So if we can track how contrast gets to the tissue (by changes in CT density or MR signal), then we can approximate how BLOOD is getting to the tissue. And how much blood is getting to the tissue is what perfusion imaging is all about. 

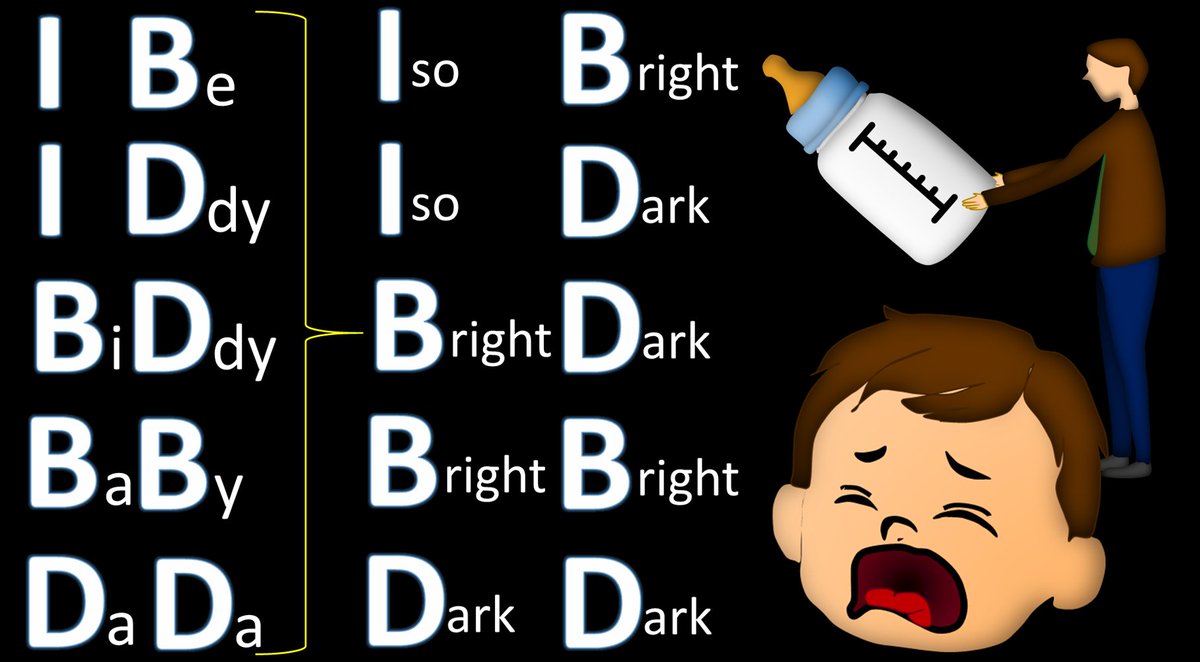
4/Clinically, there are 2 main perfusion parameters used: (1)Cerebral blood flow (CBF), which is how FAST blood gets to the tissue & (2) Tmax or time to max residue function. Everyone knows Tmax is used to estimate penumbra, but does anyone know what it really is??? You will now 

5/Let’s start w/CBF. CBF is how FAST blood gets to tissue. We could estimate it by measuring how fast contrast accumulates in tissue—make a curve of the amount of contrast in a tissue over time. If the curve has a steep slope, contrast/blood is being delivered fast & CBF is high 

6/Unfortunately, it’s not that simple. You can’t just measure the slope of the contrast curve in tissue to get CBF. Many things change how fast contrast travels besides just blood flow. If you inject more contrast or inject it faster—these increase how fast contrast washes in 

7/If we can’t measure how fast contrast washes in to get CBF, we’ll measure how it washes out! If you want to measure river velocity, dropping in dye & measuring how fast it washes out gets the same answer as watching it wash in. But we can’t drop contrast directly in the brain! 
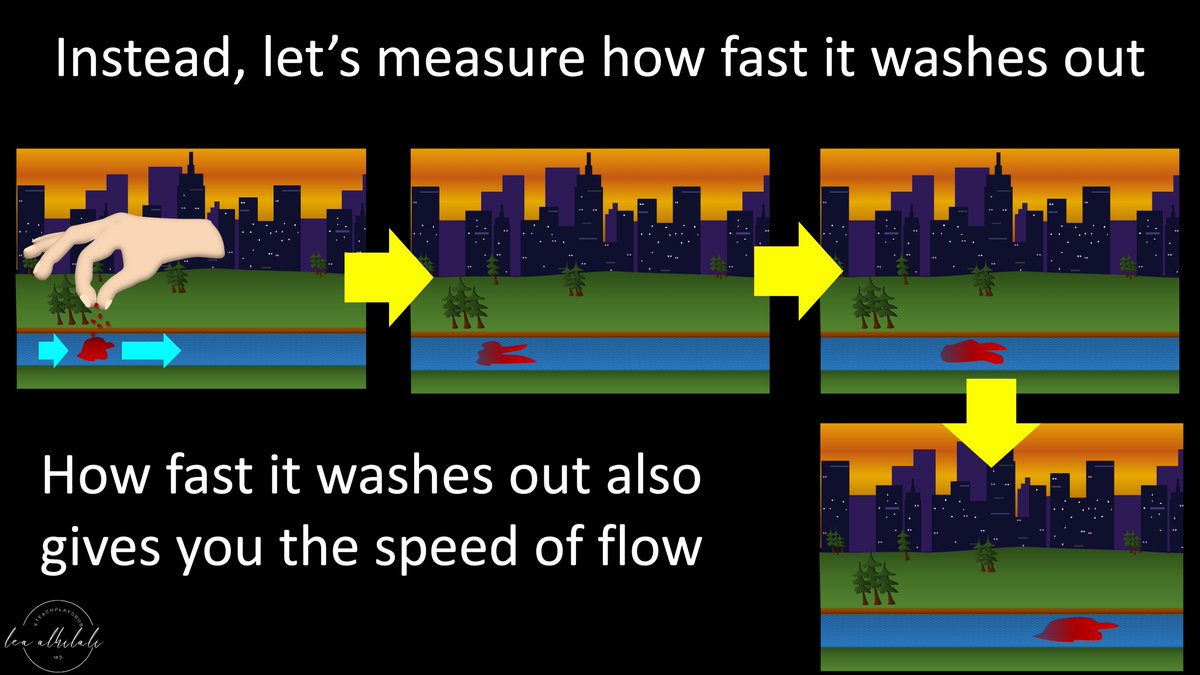
8/So we must back calculate. Pretend we want to know how fast a kitchen prepares food—Restaurant Continental Breakfast Flow or rCBF. If we know when ingredients arrive & we know when food gets on our table, we can back calculate kitchen speed--& that’s what we do for the real CBF 

9/When the ingredients arrive is the arterial input function. We measure over a cerebral artery to see when the blood first arrives. It’s equal to how long it takes the restaurant to get the ingredients from the supplier—how long it takes the artery to get blood after injection 

10/How fast food is building up on our table is the tissue concentration. We measure in brain parenchyma to detect the buildup of contrast. How long it takes for blood to get from injection to tissue is equal to how long it takes ingredients to be turned into food on our table 

11/Time for the kitchen to turn ingredients to food for the table is CBF. We want to find CBF by dropping contrast right in a brain artery & see how fast it washes out to tissue. This is kitchen time--the time for a blood drop to wash out from artery (kitchen) to tissue (table) 

12/If we know:
1)Time for blood to get from injector to artery
2)Time to get from injector to tissue
We can then back calculate time it takes to get from artery to tissue.
So we use the arterial input function & tissue concentration to back calculate the artery to tissue time
1)Time for blood to get from injector to artery
2)Time to get from injector to tissue
We can then back calculate time it takes to get from artery to tissue.
So we use the arterial input function & tissue concentration to back calculate the artery to tissue time

13/This back-calculated artery to tissue time simulates dropping blood into a brain artery & watching it wash out—like our dye & river—the best way to find CBF
This back-calculated function is the "residue function"—not a real measurement in the brain, but a calculated entity
This back-calculated function is the "residue function"—not a real measurement in the brain, but a calculated entity

14/Residue function is what you would get if you dropped a perfectly tight bolus of blood into an artery & then watched it washout into tissue as it is replaced by fresh blood. It is exactly what we wanted to do w/dye in the river 

15/The function is maximized the second you drop all that blood into the artery—before any washes out.
This is equal to the time it takes for blood to hit the artery—none has washed out.
So Tmax (time to max residue function) is the time it takes blood to reach the artery
This is equal to the time it takes for blood to hit the artery—none has washed out.
So Tmax (time to max residue function) is the time it takes blood to reach the artery

16/The height of the residue function is CBF.
This is b/c the residue function represents the blood being dropped right into the artery & timing how long it takes to wash out.
So we calculate CBF by measuring the height of the residue function
This is b/c the residue function represents the blood being dropped right into the artery & timing how long it takes to wash out.
So we calculate CBF by measuring the height of the residue function

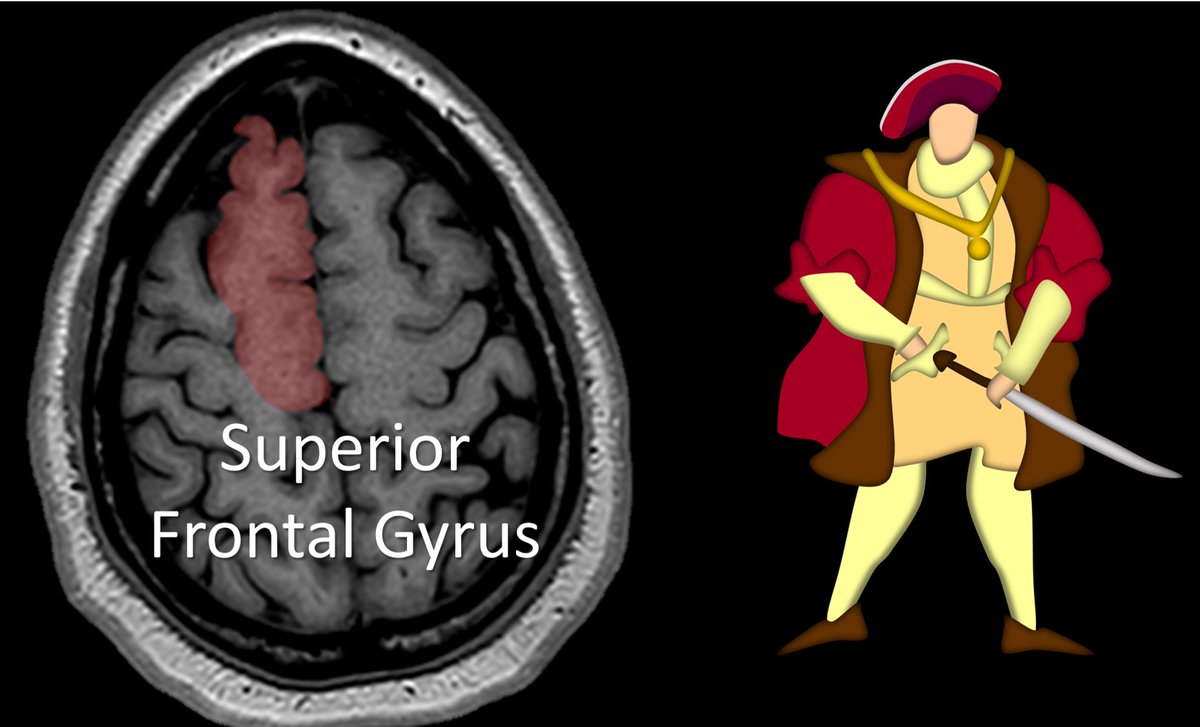
17/Since Tmax is the time it takes for blood to reach the artery, it doesn’t take into account the time it takes blood to travel through the microvasculature to the tissue. So it isn’t affected by microvascular pathology—making it a great indicator of large vessel occlusion (LVO) 

18/So now you know all the inner workings of the kitchen behind the numbers and names you seen in perfusion imaging.
May this be the Tmax of your knowledge function and leave you hungry for more!
May this be the Tmax of your knowledge function and leave you hungry for more!

• • •
Missing some Tweet in this thread? You can try to
force a refresh