Preoperative approach to sellar region masses, what the surgeon needs to know (at least what I think they need to know)
Additional reporting tips from surgeons are welcomed and encouraged! #Neurosurgery @TheASNR #radres #MedEd #MedTwitter #futureradres #endocrine #Neurology
Additional reporting tips from surgeons are welcomed and encouraged! #Neurosurgery @TheASNR #radres #MedEd #MedTwitter #futureradres #endocrine #Neurology

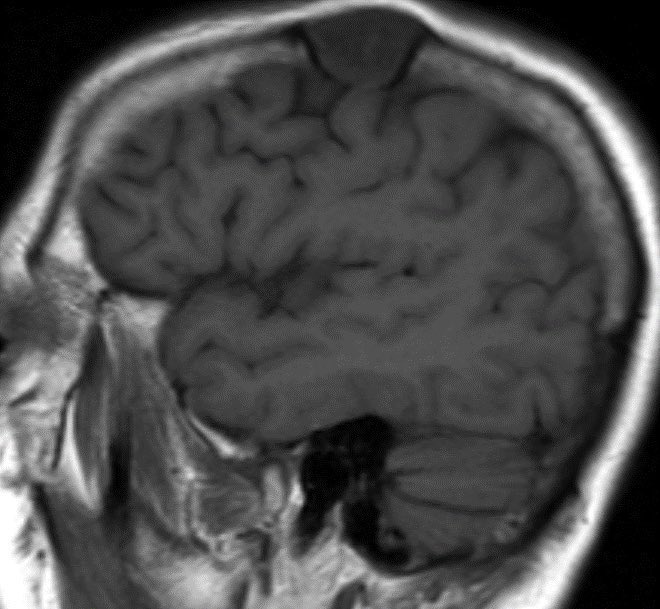
1️⃣Where is the mass located?
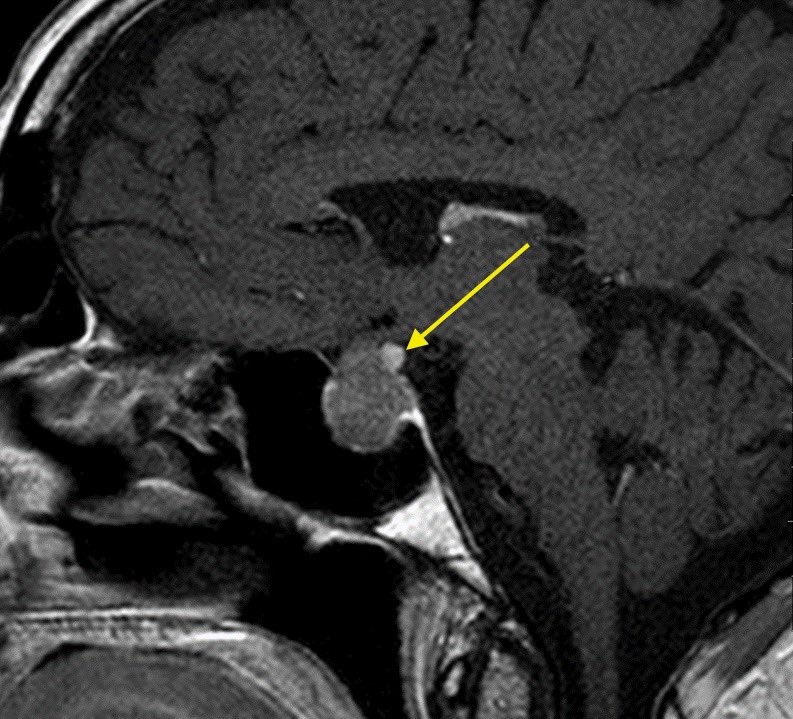
Is it sellar based? suprasellar (S)? clival? Planum sphenoidale (PS)? Tuberculum sellae (arrow)?
▶️Location can change operative approach including but not limited to subfrontal vs transsphenoidal
Is it sellar based? suprasellar (S)? clival? Planum sphenoidale (PS)? Tuberculum sellae (arrow)?
▶️Location can change operative approach including but not limited to subfrontal vs transsphenoidal

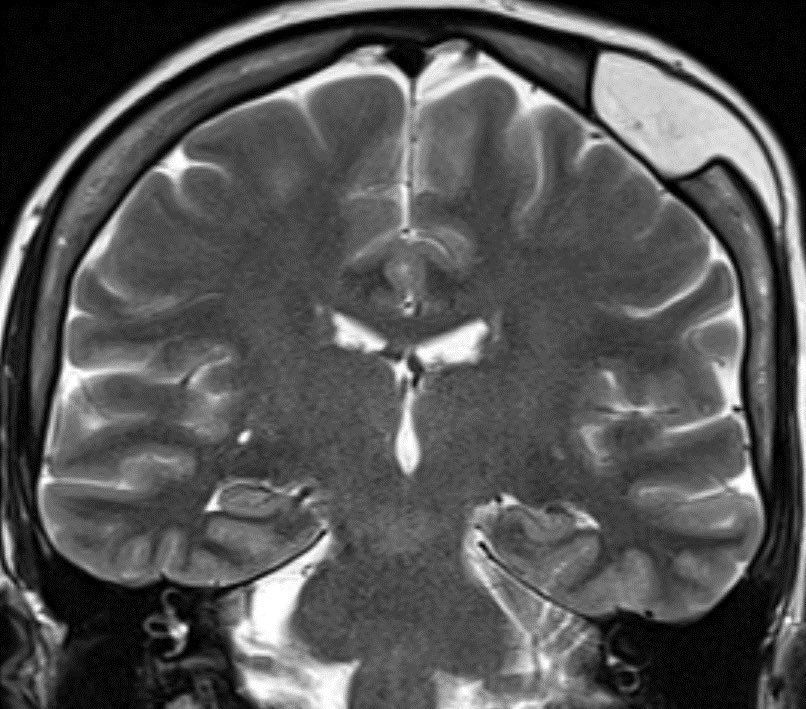
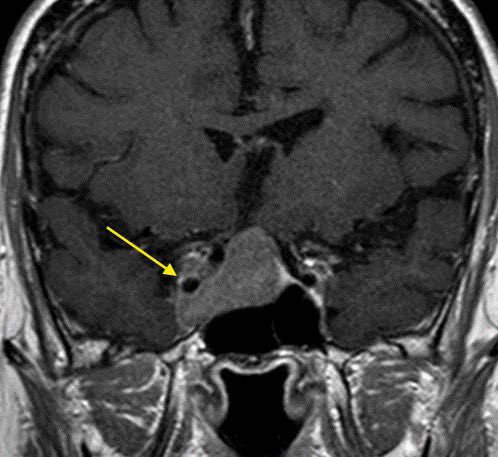
2️⃣Where is the normal pituitary gland?
▶️this can be tough when the mass is large but the normal tissue often enhances more avidly than tumor so look for a strip of relatively avid enhancement along the periphery of the mass. Surgeons do not want to remove normal pit tissue
▶️this can be tough when the mass is large but the normal tissue often enhances more avidly than tumor so look for a strip of relatively avid enhancement along the periphery of the mass. Surgeons do not want to remove normal pit tissue

3️⃣Where is the tumor in relation to the stalk?
Transection of the pit stalk can lead to endocrine dysfunction

Transection of the pit stalk can lead to endocrine dysfunction

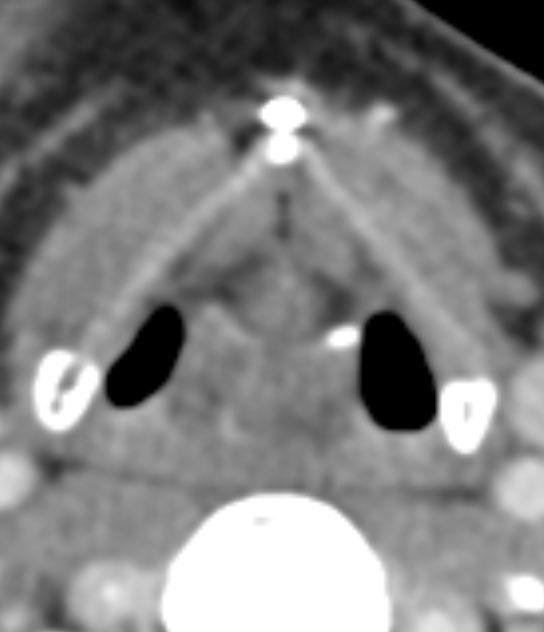
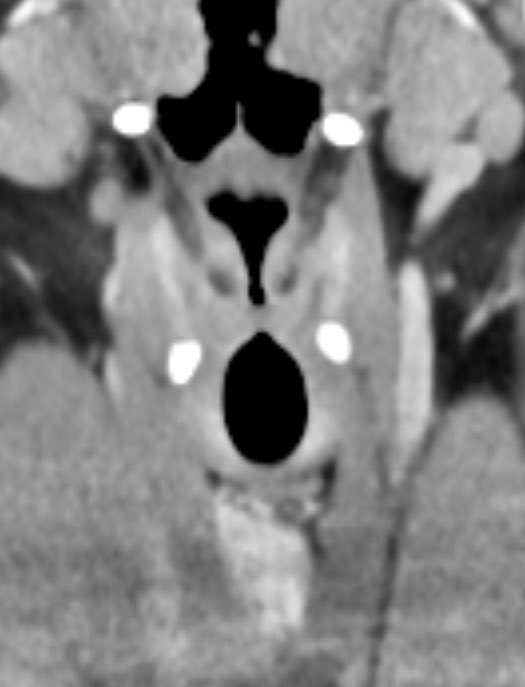
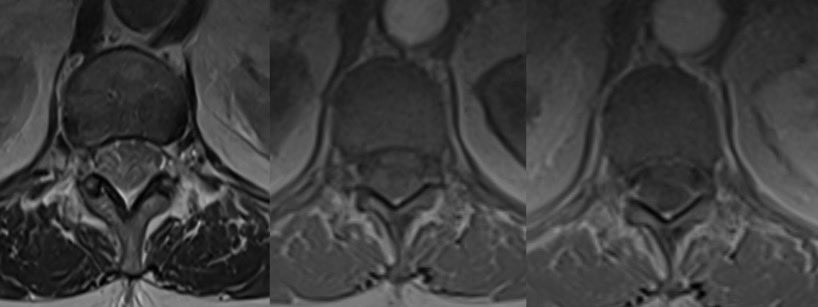
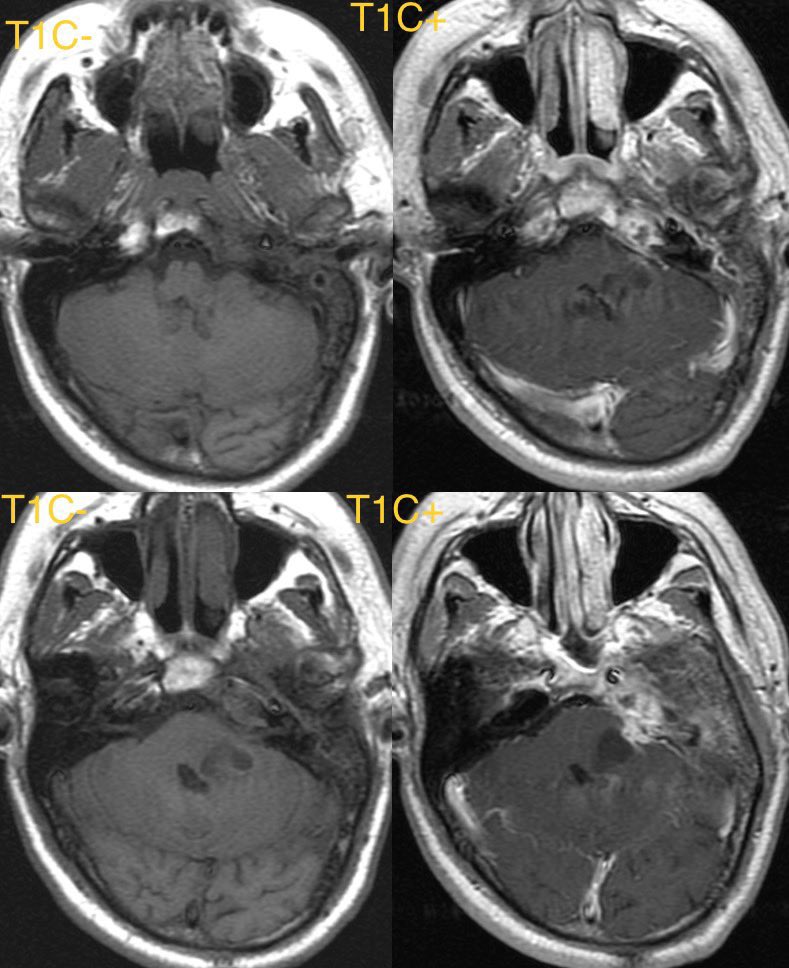
4️⃣Does the mass invade the cavernous sinus?
I have seen some variation for evaluating cavernous sinus invasion
I use encasement of greater than 2/3 of the cavernous carotid as invasion and if it crosses the midcarotid line I use that as more suggestive/indeterminate

I have seen some variation for evaluating cavernous sinus invasion
I use encasement of greater than 2/3 of the cavernous carotid as invasion and if it crosses the midcarotid line I use that as more suggestive/indeterminate

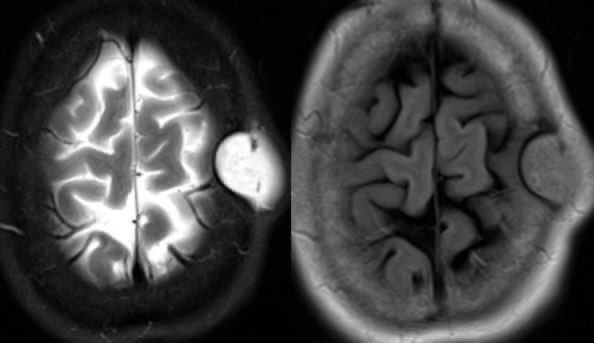
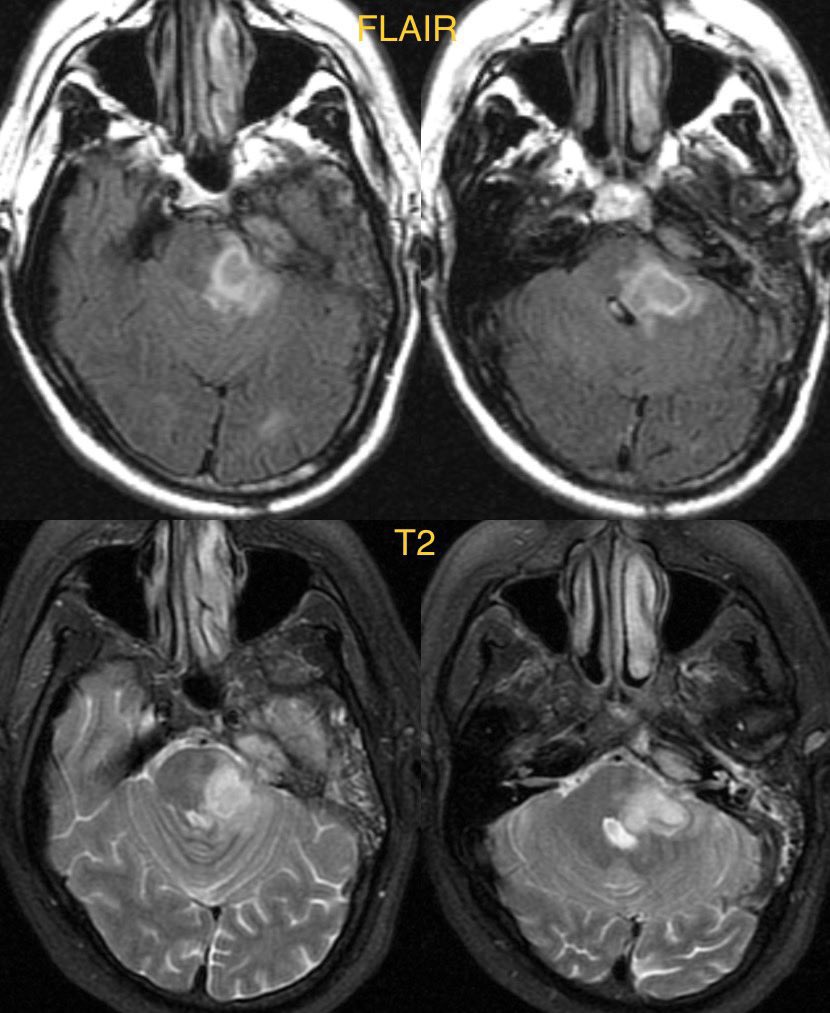
5️⃣Is there hemorrhage/evidence of apoplexy?
High signal on T1 and fluid-fluid levels on T2 suggest hemorrhage which should be correlated for apoplexy. SWI is often not helpful due to surrounding bone/air susceptibility and lack of associated hemosiderin deposition

High signal on T1 and fluid-fluid levels on T2 suggest hemorrhage which should be correlated for apoplexy. SWI is often not helpful due to surrounding bone/air susceptibility and lack of associated hemosiderin deposition


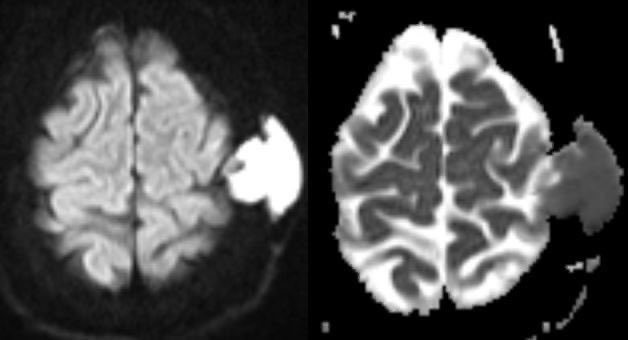
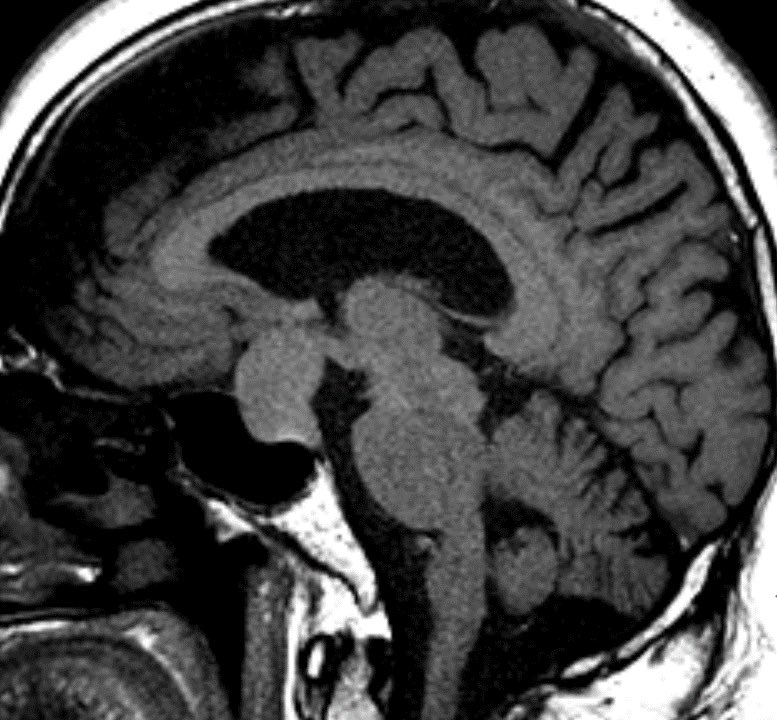
6️⃣Where is the optic chiasm? Is it compressed?
Avoiding injury to the optic chiasm and debulking tumor/decompressing the chiasm is of course, preferred

Avoiding injury to the optic chiasm and debulking tumor/decompressing the chiasm is of course, preferred

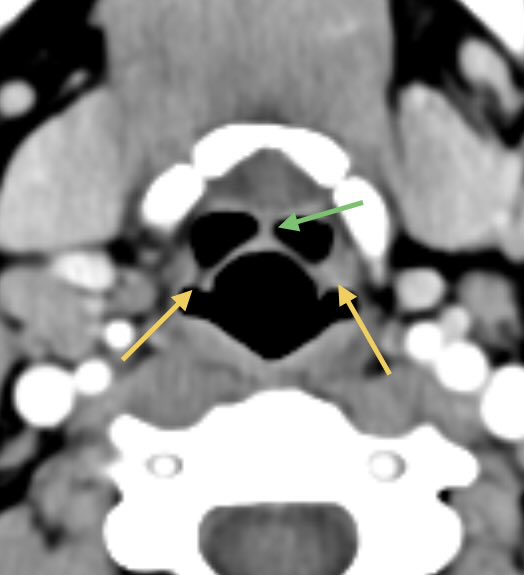
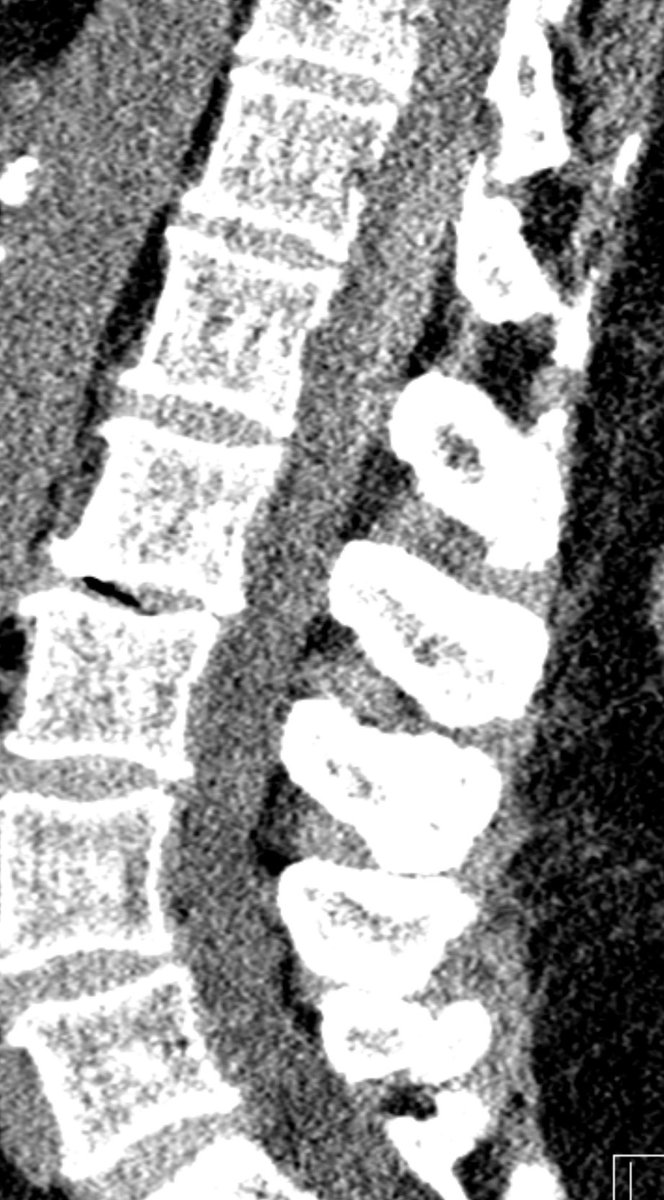
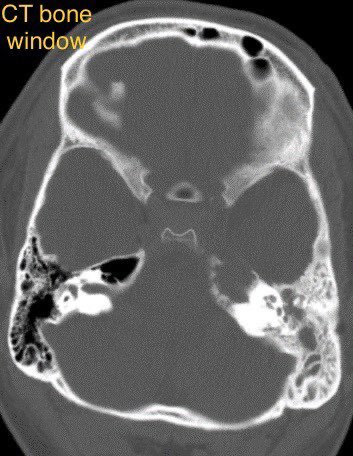
7️⃣Where is the intersinus septum of the sphenoid? Are there cavernous carotid variants? Where is the anterior clinoid in relation to the carotid? Is the carotid canal covered? Are there sphenoid sinus variants?
Sinus setum: yellow➡️
Carotid canal: green➡️
Onodi cell: red➡️

Sinus setum: yellow➡️
Carotid canal: green➡️
Onodi cell: red➡️


Learning points to report:
1️⃣Mass location
2️⃣Where is the normal pit tissue
3️⃣Stalk location
4️⃣Cavernous sinus invasion
5️⃣Any hemorrhage/apoplexy
6️⃣Optic chiasm compression
7️⃣Sphenoid sinus and carotid variant anatomy 🧠
1️⃣Mass location
2️⃣Where is the normal pit tissue
3️⃣Stalk location
4️⃣Cavernous sinus invasion
5️⃣Any hemorrhage/apoplexy
6️⃣Optic chiasm compression
7️⃣Sphenoid sinus and carotid variant anatomy 🧠
Bonus: A patent sphenopalatine artery improves the odds of a healthy nasosetal flap used to cover the surgical defect and prevent postop CSF leak. 🧠
• • •
Missing some Tweet in this thread? You can try to
force a refresh