1/Don’t let all your effort be in VEIN!
Developmental venous anomalies (DVAs) are often thought incidental but ignore them at your own risk!
A #tweetorial about how to know when DVAs are the most important finding
#meded #medtwitter #neurorad #neurotwitter #radtwitter #radres
Developmental venous anomalies (DVAs) are often thought incidental but ignore them at your own risk!
A #tweetorial about how to know when DVAs are the most important finding
#meded #medtwitter #neurorad #neurotwitter #radtwitter #radres

2/DVAs aren’t hard to recognize on imaging—they have a typical “caput medusae” appearance.
Dilated medullary veins look like snakes all converging into the medusa head of a large draining vein.
Dilated medullary veins look like snakes all converging into the medusa head of a large draining vein.

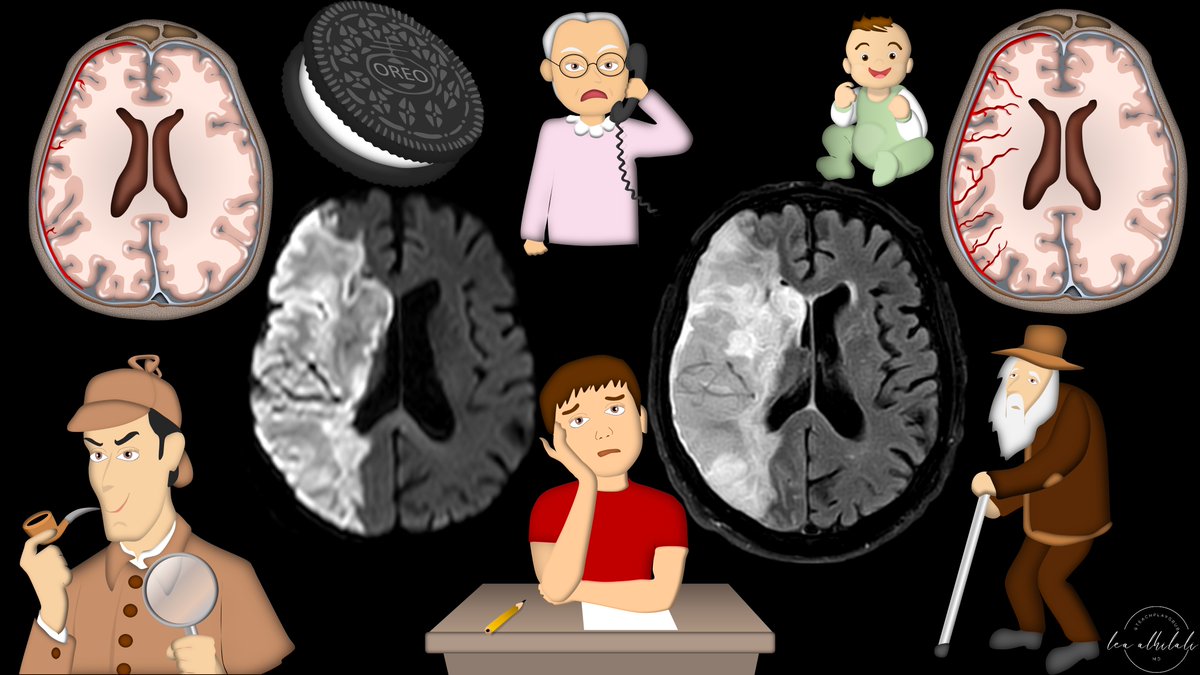
3/DVAs are incredibly common—1 in 50 may have one
Although >90% are asymptomatic, that would still results in a relatively large number of patients w/symptoms
Also, w/increasing knowledge of DVA physiology, we may find they’re responsible for more symptoms than we realize
Although >90% are asymptomatic, that would still results in a relatively large number of patients w/symptoms
Also, w/increasing knowledge of DVA physiology, we may find they’re responsible for more symptoms than we realize

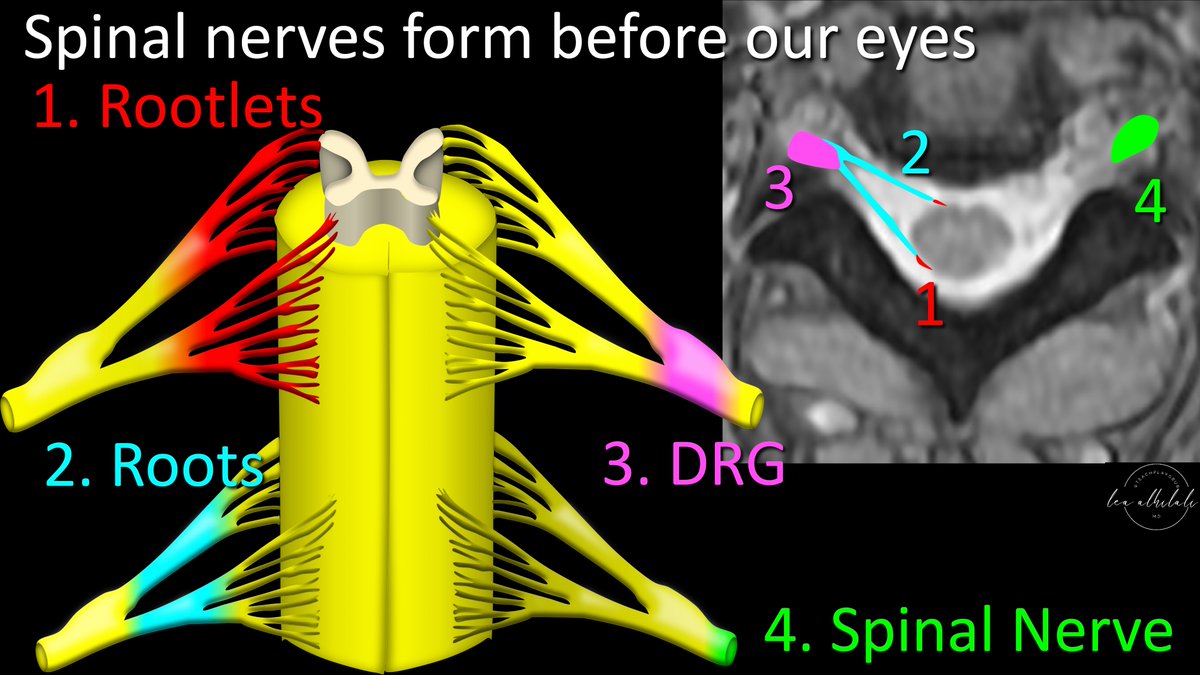
4/What causes a DVA to form? First you must understand normal venous drainage before you can understand its anomalies
Medullary veins drain the white matter & can either drain deep into subependymal veins or into superficial medullary veins & into the superficial venous system
Medullary veins drain the white matter & can either drain deep into subependymal veins or into superficial medullary veins & into the superficial venous system

5/DVAs form when normal drainage for a medullary vein doesn’t form or regresses.
The medullary veins from the opposite drainage system (either superficial or deep) swoop in like a super hero to try to save that territory, by taking over its drainage—and forming a DVA
The medullary veins from the opposite drainage system (either superficial or deep) swoop in like a super hero to try to save that territory, by taking over its drainage—and forming a DVA

6/Think of it like the morning after the party. Someone’s gotta clean up the mess & drain it away.
A DVA is what happens when the normal people responsible for cleaning up bail & some poor sucker is left cleaning up everything, even if it wasn’t his mess.
A DVA is what happens when the normal people responsible for cleaning up bail & some poor sucker is left cleaning up everything, even if it wasn’t his mess.

7/This is why DVAs always drain the opposite of what you would expect (ie, deep white matter drains superficial, superficial white matter drains deep) bc the normal drainage bailed on that white matter & a DVA was left to clean up an area that wasn’t even its mess. 

8/But obviously having 1 person do all the cleaning when it was meant for multiple people is not efficient & can overwhelm the person doing the cleaning
Same w/DVAs—they can be overwhelmed & have venous hypertension. This causes gliosis/T2 signal around it & can cause headache
Same w/DVAs—they can be overwhelmed & have venous hypertension. This causes gliosis/T2 signal around it & can cause headache

9/Venous hypertension can also affect neurological function in the region.
Poor venous drainage is like a bathtub that doesn’t drain well—stagnant water isn’t going to clean you well.
Same w/venous hypertension—region isn’t going to function well, w/hypometabolism on PET
Poor venous drainage is like a bathtub that doesn’t drain well—stagnant water isn’t going to clean you well.
Same w/venous hypertension—region isn’t going to function well, w/hypometabolism on PET

10/DVAs are not prepared to handle the extra flow. Remember, the draining stem was only expecting to handle drainage from its own medullary vein.
Making it responsible for medullary veins that should have been drained elsewhere is like turning the faucet on high
Making it responsible for medullary veins that should have been drained elsewhere is like turning the faucet on high

11/This increased flow impacts the DVA itself. It results in more pressure on the wall of the vein, resulting wall damage & thickening.
This wall damage/thickening makes DVAs more susceptible to stenoses, slow flow, & occlusions than normal veins
This wall damage/thickening makes DVAs more susceptible to stenoses, slow flow, & occlusions than normal veins

12/Increased wall pressure is like the wall receiving a punch
So you can imagine if you are punched over & over, that might make it so you don’t want to let people in—and you might close off entirely! No wonder these may thrombose!
So you can imagine if you are punched over & over, that might make it so you don’t want to let people in—and you might close off entirely! No wonder these may thrombose!

13/DVAs are also associated w/cerebral cavernous malformations or CCMs.
CCMs & DVAs go together like peas & carrots—as many as 1/3rd of CCMs have DVAs.
CCMs are prone to bleed. Many bleeds previously thought from DVAs were from associated CCMs. Why is there an association?
CCMs & DVAs go together like peas & carrots—as many as 1/3rd of CCMs have DVAs.
CCMs are prone to bleed. Many bleeds previously thought from DVAs were from associated CCMs. Why is there an association?

14/There are two theories.
First, is the hemodynamic theory.
CCM is actually a response to the parenchymal injury that comes from chronic venous hypertension & the DVA not being able to carry its flow. This results in release of angiogenetic factors as a response to injury
First, is the hemodynamic theory.
CCM is actually a response to the parenchymal injury that comes from chronic venous hypertension & the DVA not being able to carry its flow. This results in release of angiogenetic factors as a response to injury

15/Like a new baby, new vessels formed are more easily injured & then bleed
Bleeds result in more repair—like a baby crying results in parents fixing what's wrong
This spoils a baby, who's more likely to cry again. More new/weak vessels means CCM is more likely to bleed again
Bleeds result in more repair—like a baby crying results in parents fixing what's wrong
This spoils a baby, who's more likely to cry again. More new/weak vessels means CCM is more likely to bleed again

16/Second theory is the two genetic hit theory.
Mutations in the PIK3CA gene can cause DVA formation.
But like having a drink before a fight—the mutation also makes you vulnerable to a second hit.
A 2nd mutation of another gene combined w/PIK3CA can cause a CCM to form
Mutations in the PIK3CA gene can cause DVA formation.
But like having a drink before a fight—the mutation also makes you vulnerable to a second hit.
A 2nd mutation of another gene combined w/PIK3CA can cause a CCM to form

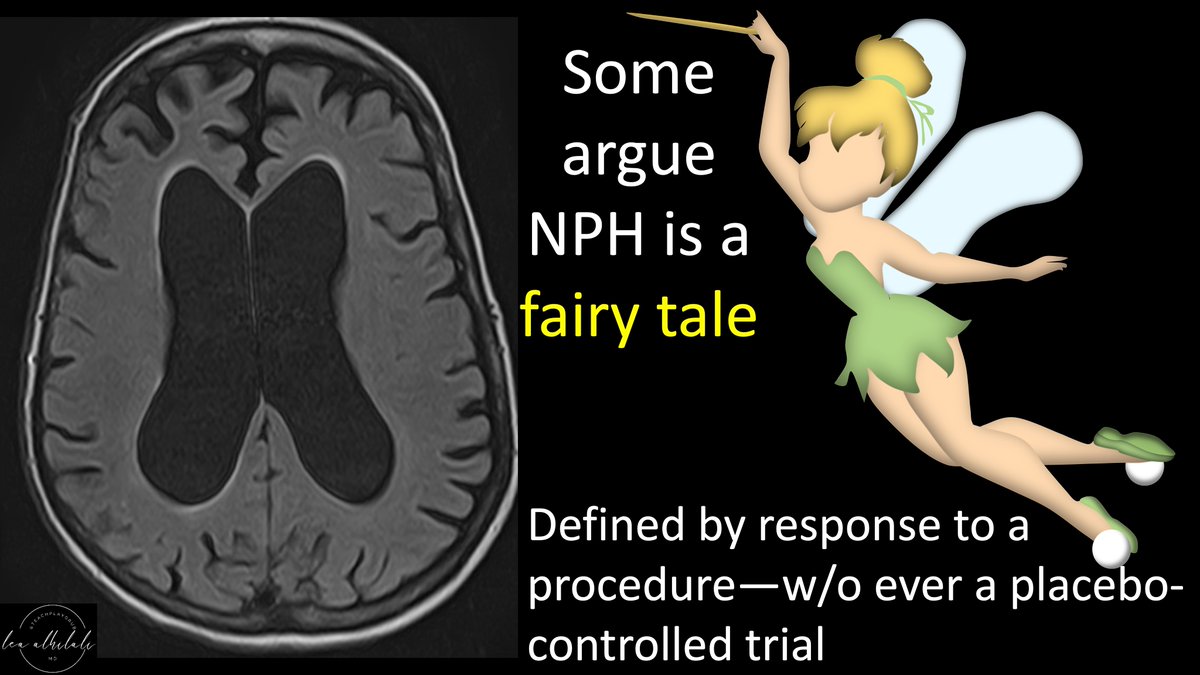
17/DVAs can also cause symptoms from mass effect.
DVAs can become large bc they drain a large territory.
B/c they are large, they can cause mass effect on the brain, cranial nerves, or even the ventricular system & cause hydrocephalus
DVAs can become large bc they drain a large territory.
B/c they are large, they can cause mass effect on the brain, cranial nerves, or even the ventricular system & cause hydrocephalus

18/When you’re overwhelmed & trying to clean up everything as fast as possible, you can accidentally pick up things that aren’t even trash & don’t need you to pick them up.
Same w/DVAs. They can pick up arterial flow & have microshunts or even AVMs—increasing risk of bleeding
Same w/DVAs. They can pick up arterial flow & have microshunts or even AVMs—increasing risk of bleeding

19/DVAs are also associated w/seizures—from CCMs & cortical malformations (also associated w/DVAs). It’s unclear if the association is b/c PIK3CA also predisposes to cortical malformations, or if normal venous architecture is important scaffolding to guide cortical development 

20/So before you write off a DVA as incidental, look for signs that it could be symptomatic, such as signs of venous hypertension (gliosis, stenosis, or microshunt) or for associated lesions such as CCMs or cortical malformations 

21/Remember, they’re not INCIDENTAL Venous Anomalies—they represent true pathology & you should be sure they don’t have abnormalities that may make them symptomatic before you write them off.
Remember, it’s always incidental to you if you don’t understand its significance!
Remember, it’s always incidental to you if you don’t understand its significance!

• • •
Missing some Tweet in this thread? You can try to
force a refresh

 Read on Twitter
Read on Twitter