1. ENTER #mRNAvaccines for #pancreaticcancer! Long-term #PDAC survivor story PART3.
"Do #PDACs REALLY have vaccine neoantigens (NAs)"? (aren’t they lowly mutated?)
If each patient = own NAs, how do you vaccinate?
Maybe mRNA? But how?
@Nature nature.com/articles/s4158…
👇🏽 [1/32]
"Do #PDACs REALLY have vaccine neoantigens (NAs)"? (aren’t they lowly mutated?)
If each patient = own NAs, how do you vaccinate?
Maybe mRNA? But how?
@Nature nature.com/articles/s4158…
👇🏽 [1/32]
2. In 2017, we reported in @Nature here -> nature.com/articles/natur… -> that primary tumors of long-term survivors of #PDAC had ~12x more activated CD8 T cells vs. short-term survivors
AND
despite #PDAC’s few mutations, mutation-derived NAs may still be T cell antigens in #PDAC.
AND
despite #PDAC’s few mutations, mutation-derived NAs may still be T cell antigens in #PDAC.
3. Now, prevailing belief ->#PDAC = few mutations = fewer mutation-derived NAs = NAs unlikely #PDAC T cell antigens.
BUT...our #NeoantigenQualityModel(estimates the ~1-2% of immunogenic NAs)
found that long term #PDACsurvivors ∝ more “high quality” NAs ∝longer survival.
BUT...our #NeoantigenQualityModel(estimates the ~1-2% of immunogenic NAs)
found that long term #PDACsurvivors ∝ more “high quality” NAs ∝longer survival.

4. Ok, so……maybe NAs are spontaneous #PDAC antigens?
But these are merely correlations…any more evidence?
But these are merely correlations…any more evidence?
5. So, in 2022 – we examined how “high quality” NAs evolved in long term #PDACsurvivors from primary to recurrent tumors
Hypothesis: If “high quality” NAs = spontaneous #PDACantigens -> expect selective editing.
Results? Generally consistent [see ->
Hypothesis: If “high quality” NAs = spontaneous #PDACantigens -> expect selective editing.
Results? Generally consistent [see ->
https://twitter.com/TheVinodLab/status/1527340213479313409?s=20]
6. So, this led to the question:
-> if NAs are spontaneously immunogenic in long-term #PDAC survivors -> then longer survival
-> so can you make NAs immunogenic with #vaccines when NAs are not spontaneously immunogenic (i.e., phenocopy long-term #PDAC survivors with a therapy)?
-> if NAs are spontaneously immunogenic in long-term #PDAC survivors -> then longer survival
-> so can you make NAs immunogenic with #vaccines when NAs are not spontaneously immunogenic (i.e., phenocopy long-term #PDAC survivors with a therapy)?
7. But for #PDAC NA #vaccines, 👆🏽findings indicated 3 challenges:
a) #PDAC NAs individual to each tumor –> thus #vaccines must be custom-made.
b) #PDAC similar to many fast-evolving clones -> thus #vaccines must target multiple clones (and thus NAs)
a) #PDAC NAs individual to each tumor –> thus #vaccines must be custom-made.
b) #PDAC similar to many fast-evolving clones -> thus #vaccines must target multiple clones (and thus NAs)
8. #PDAC patients need rapid treatment -> thus #vaccines must be made quickly.
What platform fulfills all 3 requirements?
We thought, mRNA.
What platform fulfills all 3 requirements?
We thought, mRNA.

9. So, in 2017, we partnered with Ira Mellman @genentech + Ugur Sahin @BioNTech_Group, to answer:
Are #mRNAvaccinesagainst NAs in #PDAC
1) Feasible (despite #PDACs have few NAs)?
2) Safe?
3) Able to activate T cells?
Now answers in @Nature nature.com/articles/s4158….
Are #mRNAvaccinesagainst NAs in #PDAC
1) Feasible (despite #PDACs have few NAs)?
2) Safe?
3) Able to activate T cells?
Now answers in @Nature nature.com/articles/s4158….
10. From 2019 to 2022, we conducted a phase-I clinical trial like 👇🏽
- #PDAC surgery @MSKCancerCenter in NYC
- Ship tumors to @BioNTech_Group in ~3 days
- Make custom #mRNAvaccines for each #PDAC patient
- Vaccinate #PDAC patients 9 weeks (benchmark target) after surgery
- #PDAC surgery @MSKCancerCenter in NYC
- Ship tumors to @BioNTech_Group in ~3 days
- Make custom #mRNAvaccines for each #PDAC patient
- Vaccinate #PDAC patients 9 weeks (benchmark target) after surgery

11. Now, right after trial started, guess what? #PANDEMIC!
This posed several unique (to say the least) challenges –
- NYC was severely hit – clinical/research operations @MSKCancerCenter were in rapid flux to match #pandemic needs
This posed several unique (to say the least) challenges –
- NYC was severely hit – clinical/research operations @MSKCancerCenter were in rapid flux to match #pandemic needs
12.
- Supply chains were also disrupted –> impt. as this trial involved real-time cross-Atlantic transfer of patient-material and drug.
- @BioNTech_Group had to now also make #mRNAvaccines for SARS-CoV-2 (!)
Side story on this today in @nytimes nytimes.com/2023/05/10/hea…
- Supply chains were also disrupted –> impt. as this trial involved real-time cross-Atlantic transfer of patient-material and drug.
- @BioNTech_Group had to now also make #mRNAvaccines for SARS-CoV-2 (!)
Side story on this today in @nytimes nytimes.com/2023/05/10/hea…
13. But, thanks to phenomenal team @MSKCancerCenter, @genentech, @BioNTech_Group – despite the #pandemic, we
- completed the trial 1 year ahead of schedule
- vaccinated #PDAC patients within ~3 days of the 9 week after surgery target
- completed the trial 1 year ahead of schedule
- vaccinated #PDAC patients within ~3 days of the 9 week after surgery target

15. Ok, so this gives answer to ❓ # 1
“Are #mRNAvaccinesagainst NAs in #PDAC feasible (despite #PDACs have few NAs)”
Yes.
“Are #mRNAvaccinesagainst NAs in #PDAC feasible (despite #PDACs have few NAs)”
Yes.
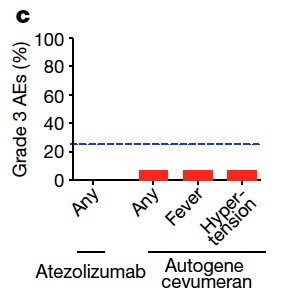
16. ❓# 2:
“Are #mRNAvaccines in #PDAC safe?”
In short – yes.
No surprises here - we now know #mRNAvaccines have good safety profile.
“Are #mRNAvaccines in #PDAC safe?”
In short – yes.
No surprises here - we now know #mRNAvaccines have good safety profile.
17. ❓# 3
“Can #mRNAvaccines activate T cells in #PDAC?
Yes.
#mRNAvaccines activate T cells in 50% of #PDAC patients
(see paper “responder” definition + discussion on why possibly 50% response, and role of the spleen)
“Can #mRNAvaccines activate T cells in #PDAC?
Yes.
#mRNAvaccines activate T cells in 50% of #PDAC patients
(see paper “responder” definition + discussion on why possibly 50% response, and role of the spleen)

18.
Great! So #mRNAvaccines can activate T cell in #PDAC. But are these T cells
a) NA-specific?
b) CD8? CD4? High magnitude?
c) Persistent (as we have to give chemotherapy after #mRNAvaccines)?
d) Functional and boostable?
Great! So #mRNAvaccines can activate T cell in #PDAC. But are these T cells
a) NA-specific?
b) CD8? CD4? High magnitude?
c) Persistent (as we have to give chemotherapy after #mRNAvaccines)?
d) Functional and boostable?
19.
❓3a: NA-specific?
Yes.
And to single + even multiple NAs. (-> see paper for more detailed mapping of #mRNAvaccine expanded T cell clones to NAs).
❓3a: NA-specific?
Yes.
And to single + even multiple NAs. (-> see paper for more detailed mapping of #mRNAvaccine expanded T cell clones to NAs).

20.
❓3b: CD8? CD4? High magnitude?”
So, to figure this out, @bengrbm and I, along with the super talents Zach Sethna + Luis Rojas developed #CloneTrack – a tool to longitudinally track #mRNAvaccine expanded T cell clones.
❓3b: CD8? CD4? High magnitude?”
So, to figure this out, @bengrbm and I, along with the super talents Zach Sethna + Luis Rojas developed #CloneTrack – a tool to longitudinally track #mRNAvaccine expanded T cell clones.
21. Sidebar – we think #CloneTrack can track any #vaccine expanded clones, so if interested 👉🏽github.com/zsethna/CloneT…
We found…
#mRNAvaccine expanded T cells are
- CD8’s (see paper; re: CD4’s > see discussion).
- High magnitude (👇🏽can reach upto 10% of all blood T cells….!)
We found…
#mRNAvaccine expanded T cells are
- CD8’s (see paper; re: CD4’s > see discussion).
- High magnitude (👇🏽can reach upto 10% of all blood T cells….!)

22.
❓3c:
Persistent (do we lose the expanded T cells after chemotherapy?)
No.
See here – they persist at quite high fractions despite post-vaccination chemotherapy.
❓3c:
Persistent (do we lose the expanded T cells after chemotherapy?)
No.
See here – they persist at quite high fractions despite post-vaccination chemotherapy.

23.
❓3d:
Functional and boostable?
Yes.
Produced polyfunctional cytokines + re-expanded with #mRNAvaccine booster in all patients.

❓3d:
Functional and boostable?
Yes.
Produced polyfunctional cytokines + re-expanded with #mRNAvaccine booster in all patients.


24. OK!
What about clinical outcome?
At a median follow-up of 18months (this extended beyond our pre-specified secondary endpoint of 18m recurrence free survival) 👇🏽
What about clinical outcome?
At a median follow-up of 18months (this extended beyond our pre-specified secondary endpoint of 18m recurrence free survival) 👇🏽

25. Could this correlation be due to differences in patient selection?
We did not find any evidence (-> see paper).
Also - no evidence that non-responders were less “immune fit”
-> they mounted nice immune response to CONCURRENT, UNRELATED #mRNAvaccine (SARS-CoV-2)
We did not find any evidence (-> see paper).
Also - no evidence that non-responders were less “immune fit”
-> they mounted nice immune response to CONCURRENT, UNRELATED #mRNAvaccine (SARS-CoV-2)

27. Can #mRNAvaccine expanded T cells detect micrometastases?
Interesting clinical vignette in Figure 4 👉🏽 here nature.com/articles/s4158….
Interesting clinical vignette in Figure 4 👉🏽 here nature.com/articles/s4158….
28. TAKE HOME:
- #mRNAvaccines in #PDAC – encouraging therapeutic signal
- Feasible
- Immunogenic (substantially + durably expands T cells)
- #mRNAvaccines immunity correlates with delayed recurrence
- Larger trial needed (randomized #PDAC trial opening SOON – stay tuned!)
- #mRNAvaccines in #PDAC – encouraging therapeutic signal
- Feasible
- Immunogenic (substantially + durably expands T cells)
- #mRNAvaccines immunity correlates with delayed recurrence
- Larger trial needed (randomized #PDAC trial opening SOON – stay tuned!)
29. Implications for other cancers?
Well, if #mRNAvaccines can stimulate high magnitude T cells in #PDAC where there are fewer NAs 👇🏽
Logical to extend to other cancers with fewer NAs (that were also thought to have insufficient NAs for #vaccines)
Well, if #mRNAvaccines can stimulate high magnitude T cells in #PDAC where there are fewer NAs 👇🏽
Logical to extend to other cancers with fewer NAs (that were also thought to have insufficient NAs for #vaccines)
30. Nice summaries of today’s paper
-> here from @NeehaZaidi nature.com/articles/d4158…
-> here from @MSKCancerCenter mskcc.org/news/can-mrna-…
And shareable link -> rdcu.be/dbPBq
-> here from @NeehaZaidi nature.com/articles/d4158…
-> here from @MSKCancerCenter mskcc.org/news/can-mrna-…
And shareable link -> rdcu.be/dbPBq
31. SO MANY AWESOME COLLEAGUES to highlight!
Luis Rojas, Zach Sethna @TheVinodLab; Ira Mellman @genentech, Ugur Sahin @BioNTech_Group; @EileenMOReilly, Jeffrey Drebin, and many talented physicians @MSKCancerCenter; my wonderful @CompOncMSK colleague @bengrbm + many others!
Luis Rojas, Zach Sethna @TheVinodLab; Ira Mellman @genentech, Ugur Sahin @BioNTech_Group; @EileenMOReilly, Jeffrey Drebin, and many talented physicians @MSKCancerCenter; my wonderful @CompOncMSK colleague @bengrbm + many others!
32. And huge thank you to our funders!
@SU2C @lustgartenfdn @DamonRunyon @NIH @NCI @psscra @CpcrMsk @parkerici #CancerMoonshot who supported @TheVinodLab when we began studying long-term #PDAC survivors and this trial !
And our patients! Thank you! You are amazing!!
That's all!
@SU2C @lustgartenfdn @DamonRunyon @NIH @NCI @psscra @CpcrMsk @parkerici #CancerMoonshot who supported @TheVinodLab when we began studying long-term #PDAC survivors and this trial !
And our patients! Thank you! You are amazing!!
That's all!
• • •
Missing some Tweet in this thread? You can try to
force a refresh

 Read on Twitter
Read on Twitter






