A #dermtwitter #tweetorial on the skin manifestations of:
SYPHILIS!
#MedEd #FOAMEd #medtwitter #syphilis @VisualDx
pc: en.wikipedia.org/wiki/Treponema…
1/
SYPHILIS!
#MedEd #FOAMEd #medtwitter #syphilis @VisualDx
pc: en.wikipedia.org/wiki/Treponema…
1/

Let's go back to the basics. Syphilis is from an infection by the bacterium Treponema pallidum. Usually spread by sexual means, syphilis has three main stages of disease.
Primary infection usually presents as a papule that turns into a painless ulcer called a chancre.
2/
Primary infection usually presents as a papule that turns into a painless ulcer called a chancre.
2/

Time from inoculation to chancre usually is 10-90 days (21 days is most typical).
There is a rare variant where the patient can get many smaller ulcerations, which is called Follman balanitis.
3/
There is a rare variant where the patient can get many smaller ulcerations, which is called Follman balanitis.
3/

Remember that early on, testing for syphilis can be negative because there isn't any hematogenous spread yet making serologic testing negative. You could use dark field microscopy, but usually empiric treatment (with penicillin) is used due to lack of accessibility of testing.
4/
4/
If the patient isn't treated, the chancre heals spontaneously 3-6 weeks later. Then, the spirochete can spread hematogenously and cause secondary syphilis (usually 3-10 weeks after the chancre).
Patient can have fever, malaise, lymphadenopathy, myalgias, headache.
5/
Patient can have fever, malaise, lymphadenopathy, myalgias, headache.
5/
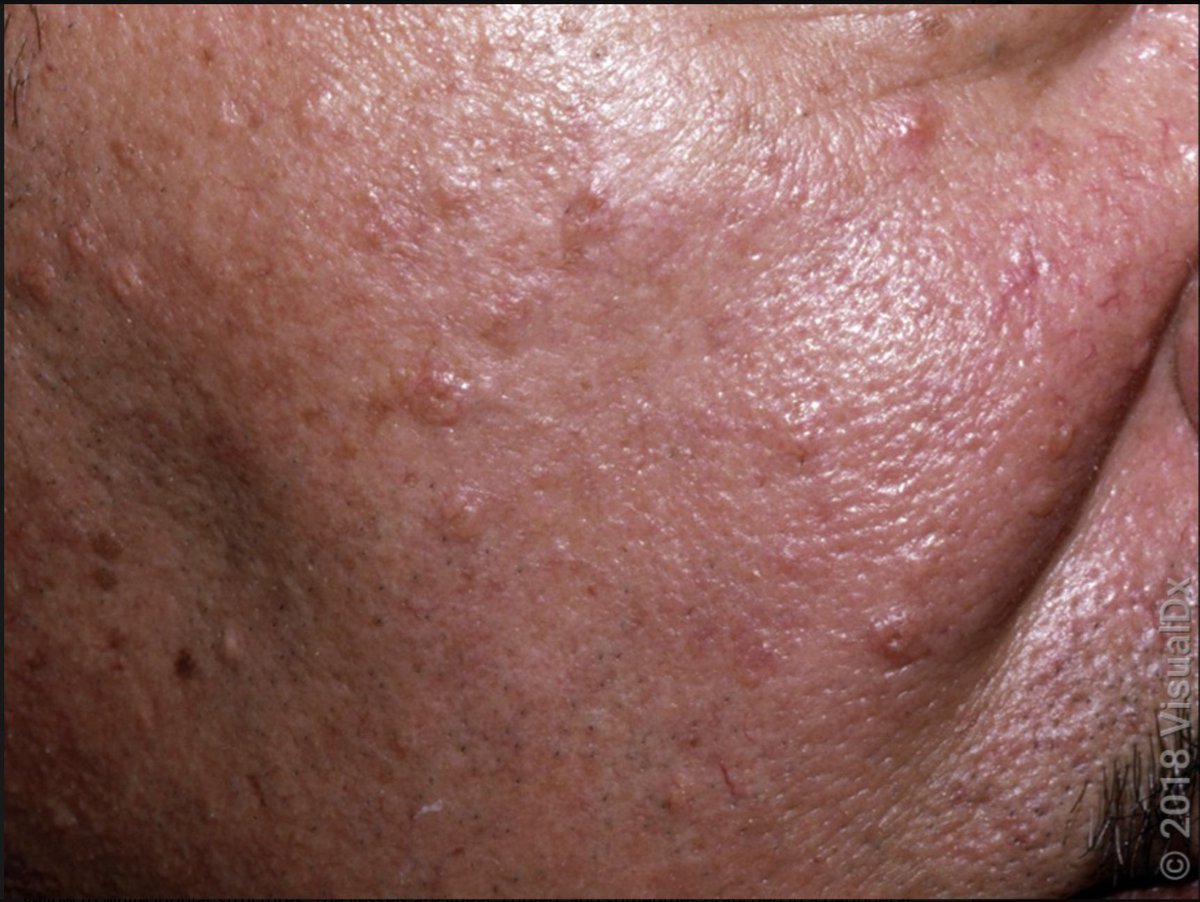
What about the skin?! In short, secondary syphilis can look like anything.
That said, the classic exam is papulosquamous (bumpy with scale). I've heard the typical exam described as "copper pennies" (see pics) including the palms and soles.
6/

That said, the classic exam is papulosquamous (bumpy with scale). I've heard the typical exam described as "copper pennies" (see pics) including the palms and soles.
6/


The scalp can also be involved with secondary syphilis. Described as "moth eaten alopecia (pic 1)."
There can also be mucosal lesions, and condyloma lata can appear, which highly infectious. (pic 2).
pc: ncbi.nlm.nih.gov/pmc/articles/P…
nejm.org/doi/full/10.10…
7/

There can also be mucosal lesions, and condyloma lata can appear, which highly infectious. (pic 2).
pc: ncbi.nlm.nih.gov/pmc/articles/P…
nejm.org/doi/full/10.10…
7/


In secondary syphilis, serologic testing would be positive. A quick interlude to discuss testing:
Remember that there are treponemal tests (TT) and nontreponemal tests (NTT). Classically, you'd start with a NTT (like an RPR) and confirm with a TT (like an FTA-ABS).
8/
Remember that there are treponemal tests (TT) and nontreponemal tests (NTT). Classically, you'd start with a NTT (like an RPR) and confirm with a TT (like an FTA-ABS).
8/
However, TT are now often run first with a NTT used to confirm (reverse of prior) for cost/automation reasons.
NTTs can also exhibit prozone effect with high bacterial/antibody level. Samples need dilution if you have a high index of suspicion. Our lab does it automatically.
9/
NTTs can also exhibit prozone effect with high bacterial/antibody level. Samples need dilution if you have a high index of suspicion. Our lab does it automatically.
9/
Also, NTTs work by detecting antibodies to lipids like cardiolipin that are produced from T pallidum binding. For that reason, you can get false positives (as can be seen in antiphospholipid/anticardiolipin and lupus).
TTs have also been reported to cause false positives!
10/
TTs have also been reported to cause false positives!
10/
Okay - back to skin manifestations:
If secondary syphilis isn't treated, it will resolve in 3-12 weeks, and then months to years later, tertiary syphilis can occur.
Tertiary syphilis presents on the skin with gummas which are locally destructive but heal spontaneously.
11/

If secondary syphilis isn't treated, it will resolve in 3-12 weeks, and then months to years later, tertiary syphilis can occur.
Tertiary syphilis presents on the skin with gummas which are locally destructive but heal spontaneously.
11/


In tertiary syphilis, you can get other manifestations like Argyll Robertson pupil, Tabes dorsalis, aortitis, etc.
Some notes:
Remember that neurosyphilis can occur at any stage of disease!
If patients are HIV+, disease progression can be much more severe and rapid.
12/
Some notes:
Remember that neurosyphilis can occur at any stage of disease!
If patients are HIV+, disease progression can be much more severe and rapid.
12/
Since this #tweetorial is already getting much too long, I'm going to leave congenital syphilis for another time!
We also didn't get into treatment, but penicillin is really the best treatment - even PCN allergic patients are usually desensitized so they can receive it.
13/
We also didn't get into treatment, but penicillin is really the best treatment - even PCN allergic patients are usually desensitized so they can receive it.
13/
I also think It's important to acknowledge the awful things that happened as a part of the unethical Tuskegee Syphilis Study. The deceiving of hundreds of African Americans led to unnecessary suffering, which has also led to longer lasting effects:
theatlantic.com/politics/archi…
14/
theatlantic.com/politics/archi…
14/
Let's recap skin findings:
✅ Syphilis usually presents as a painless chancre.
✅ If untreated, secondary syphilis presents with a papulosquamous eruption (but can look like anything).
✅ If still untreated, gummas appear in tertiary syphilis.
✅ Treat empirically if early!
15/
✅ Syphilis usually presents as a painless chancre.
✅ If untreated, secondary syphilis presents with a papulosquamous eruption (but can look like anything).
✅ If still untreated, gummas appear in tertiary syphilis.
✅ Treat empirically if early!
15/
Thanks for joining. We talked about syphilis and the skin, touched a little on testing, and left a lot on the table if others (especially from #IDtwitter or #dermtwitter) want to jump in.
Hope you learned something to take with you wherever you are in your medical journey!
16/16
Hope you learned something to take with you wherever you are in your medical journey!
16/16
• • •
Missing some Tweet in this thread? You can try to
force a refresh

 Read on Twitter
Read on Twitter