
Heart rhythm doc, writer for @Medscape, host of This Week in Cardiology podcast, editor of Sensible Medicine. The more you see, the harder medicine gets.
How to get URL link on X (Twitter) App


https://twitter.com/JReinerMD/status/1416811058040344584
 I discussed my experience in clinic with vaccine hesitant patients on This Week in Cardiology podcast
I discussed my experience in clinic with vaccine hesitant patients on This Week in Cardiology podcast https://twitter.com/plenary_session/status/1370509641709359107This principles in this podcast are so darn important for critical appraisal

https://twitter.com/JACCJournals/status/1370457134194917381Background:

https://twitter.com/PerPersvensson/status/1355426831797772290Here are the events to put in the 2x2 table and the published CI and RR



 He used a variant of ...sit down for this...the Fragility Index, which we reported on in cardiology
He used a variant of ...sit down for this...the Fragility Index, which we reported on in cardiology 

 If you put the new treatment on the left side of the interpretative diagram, there are four ways to make Non-inferiority. Scenarios 1-4. but....
If you put the new treatment on the left side of the interpretative diagram, there are four ways to make Non-inferiority. Scenarios 1-4. but.... 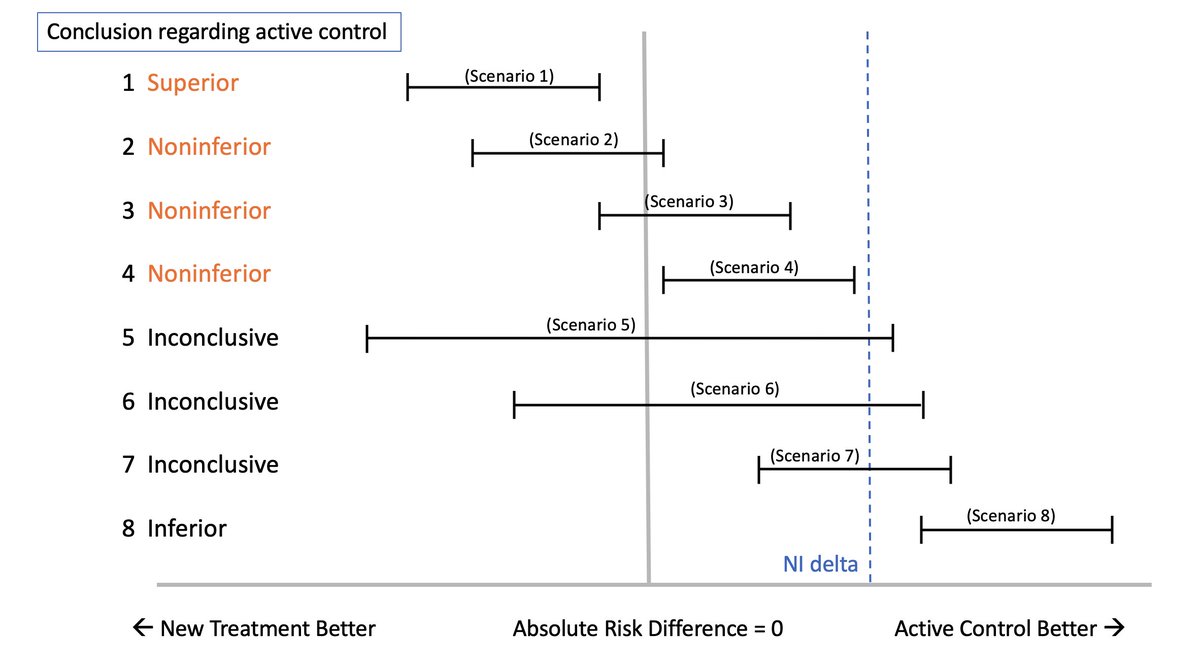
 It is an important topic b/c numerous studies have suggested a high rate of clot-related complications in acute #COVID19 illness. it makes sense to consider anti-coagulants...
It is an important topic b/c numerous studies have suggested a high rate of clot-related complications in acute #COVID19 illness. it makes sense to consider anti-coagulants...



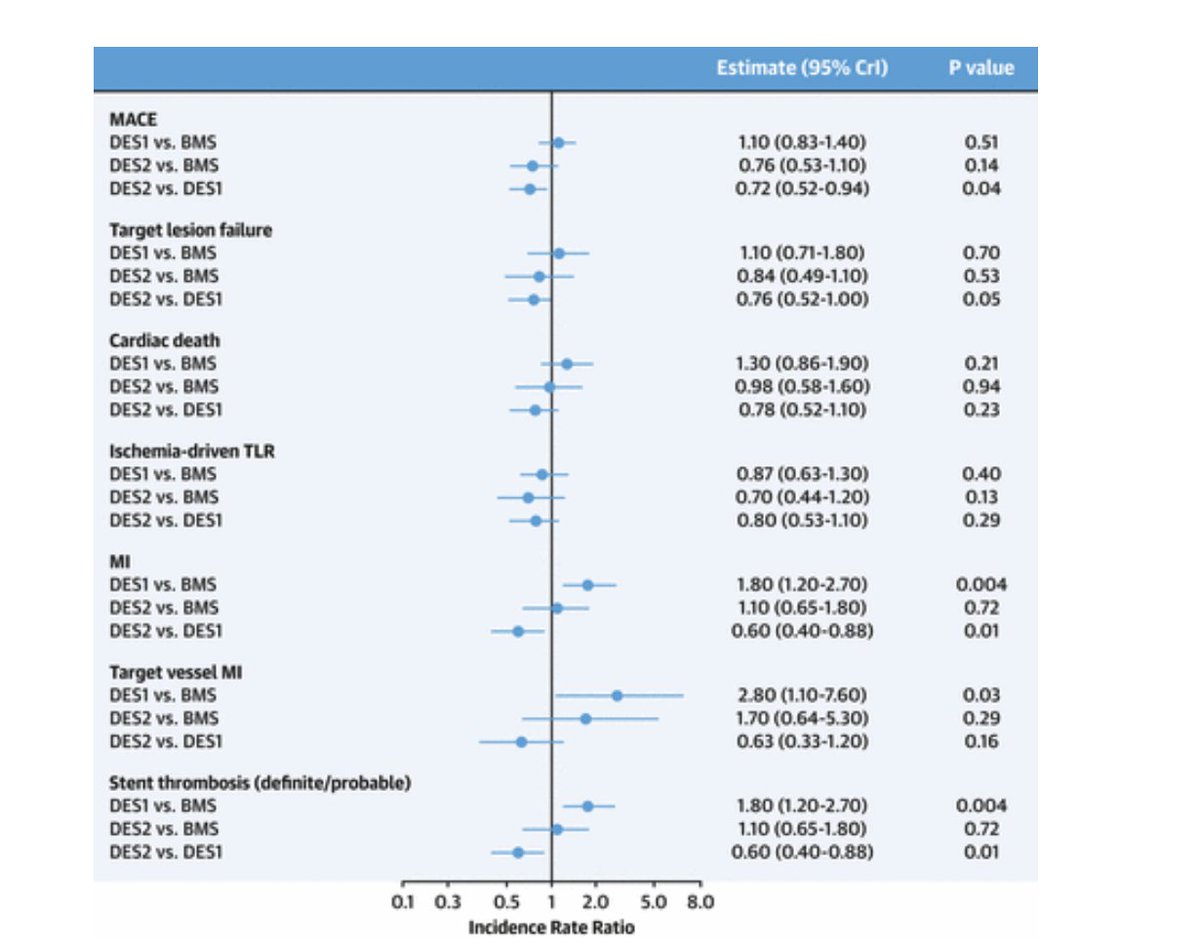
 2/ the other notable feature is that it lends credence to the findings of NORSTENT nejm.org/doi/full/10.10…
2/ the other notable feature is that it lends credence to the findings of NORSTENT nejm.org/doi/full/10.10…
 That's important because any human being given the choice b/w a PCI or open-heart surgery will choose PCI b/c it's far less invasive.
That's important because any human being given the choice b/w a PCI or open-heart surgery will choose PCI b/c it's far less invasive. 