PML in MS
Progressive multifocal leukoencephalopathy (PML) is an opportunistic infection of the CNS caused by John Cunningham virus (JCV)
PML in the setting of monoclonal antibody therapy has attracted tremendous attention particularly in MS patients treated with natalizumab/NTZ.
Progressive multifocal leukoencephalopathy (PML) is an opportunistic infection of the CNS caused by John Cunningham virus (JCV)
PML in the setting of monoclonal antibody therapy has attracted tremendous attention particularly in MS patients treated with natalizumab/NTZ.
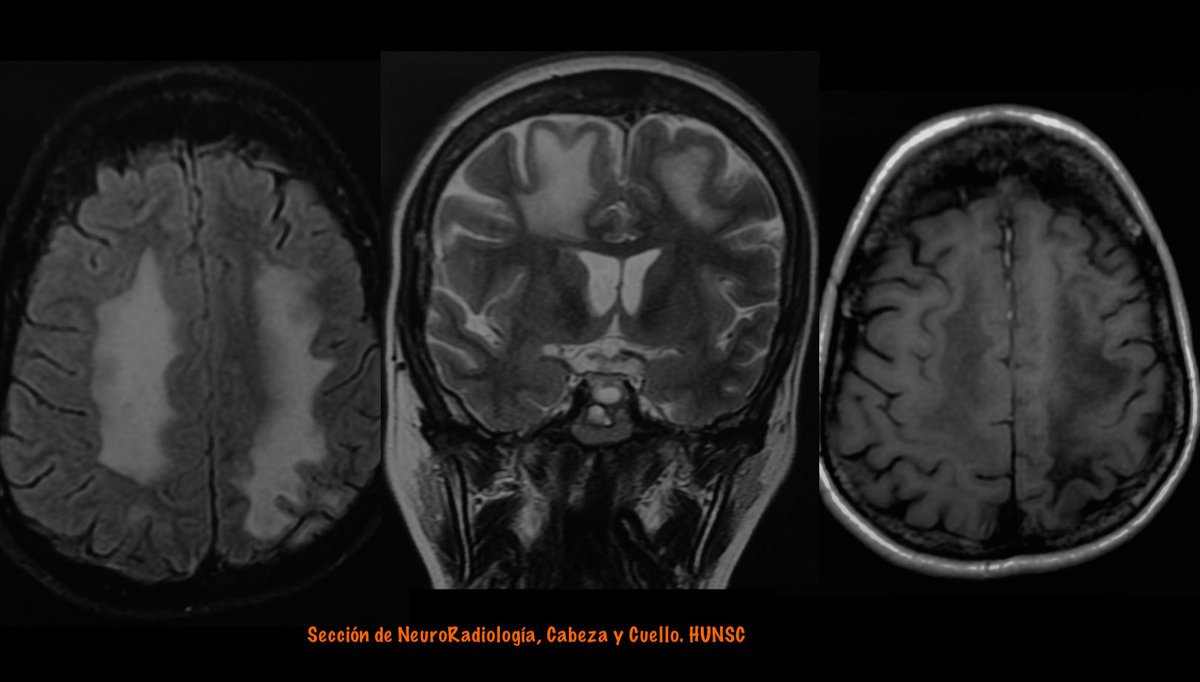
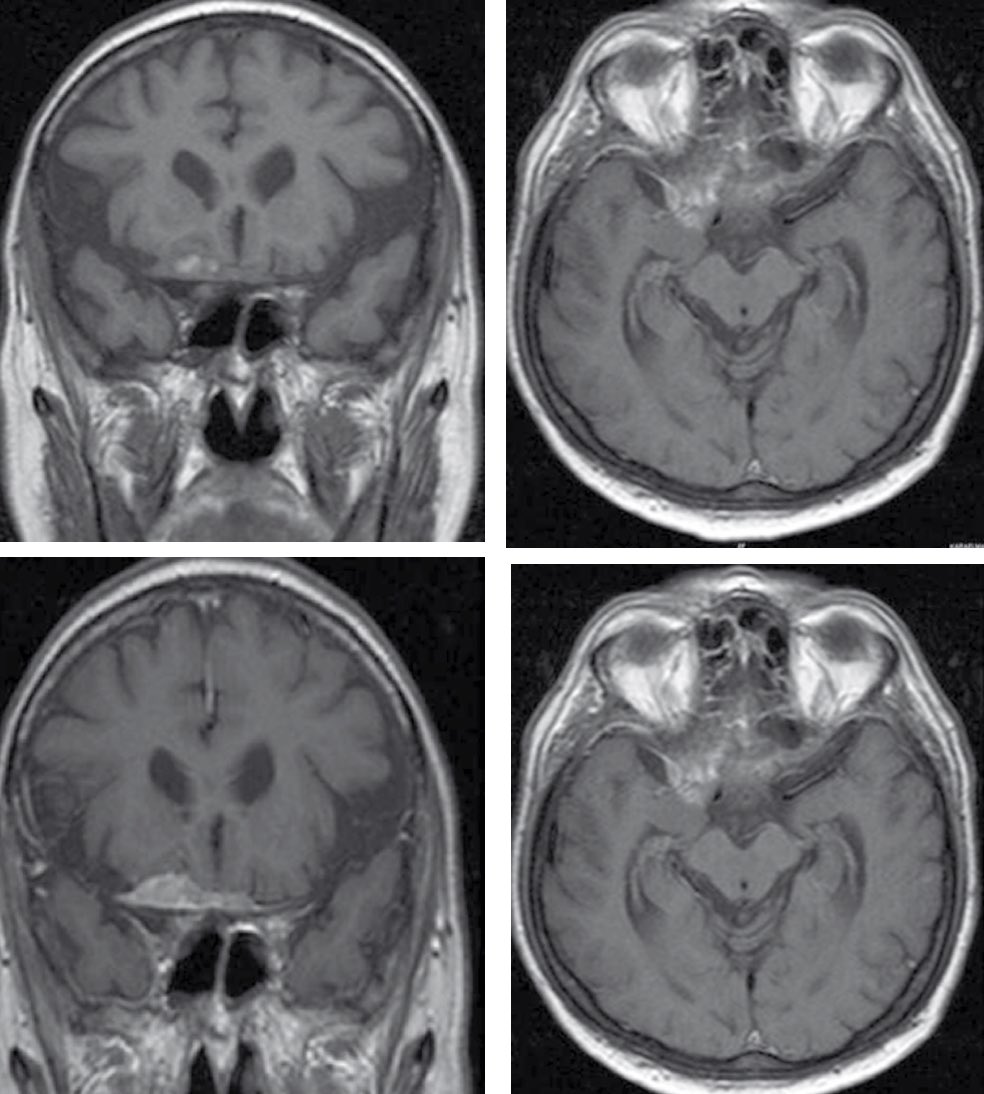
Features favoring PML over MS (as proposed by Yousry et al) are the following:
1) Diffuse subcortical rather than periventricular white matter involvement; frequent involvement of posterior fossa.
2) Irregular ill-defined infiltrating edge confined to the white matter.
1) Diffuse subcortical rather than periventricular white matter involvement; frequent involvement of posterior fossa.
2) Irregular ill-defined infiltrating edge confined to the white matter.

3) Persistent progression of the lesion confined within the white matter tract.
4) No mass effect even in large lesions.
5) Diffuse increased T2 signal intensity; recently involved areas more T2 hyperintense than the old areas.
4) No mass effect even in large lesions.
5) Diffuse increased T2 signal intensity; recently involved areas more T2 hyperintense than the old areas.
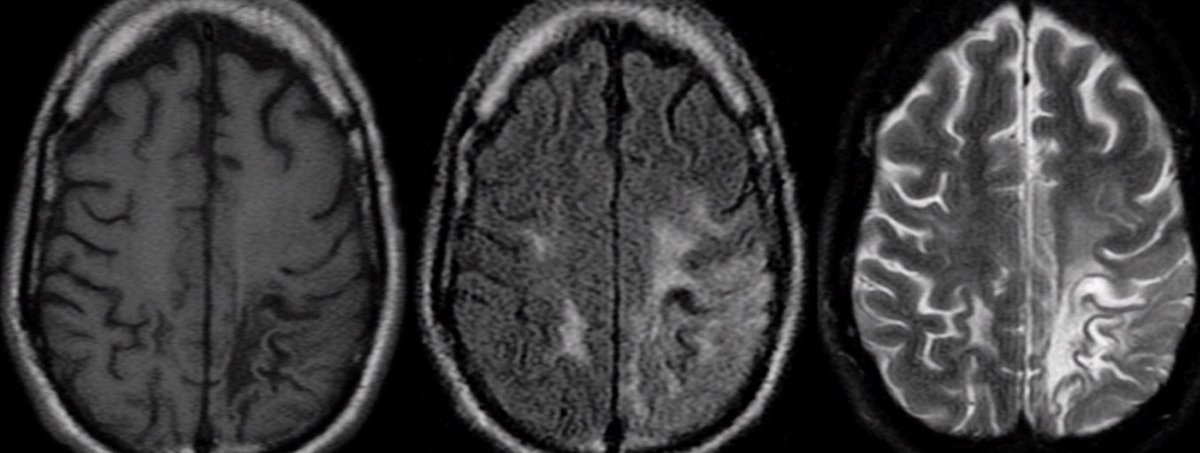
6) Initially iso- to hypointense with an incremental drop of T1 signal intensity with time; signal intensity never returning to normal.
7) Typically no enhancement, even in large lesions.
7) Typically no enhancement, even in large lesions.

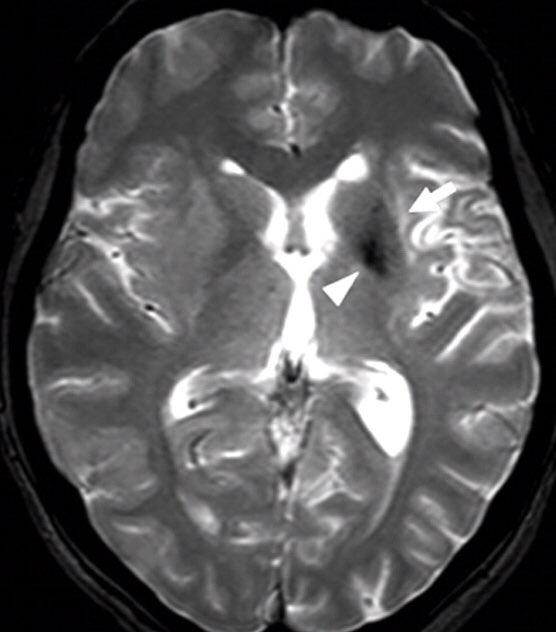
DWI In PML
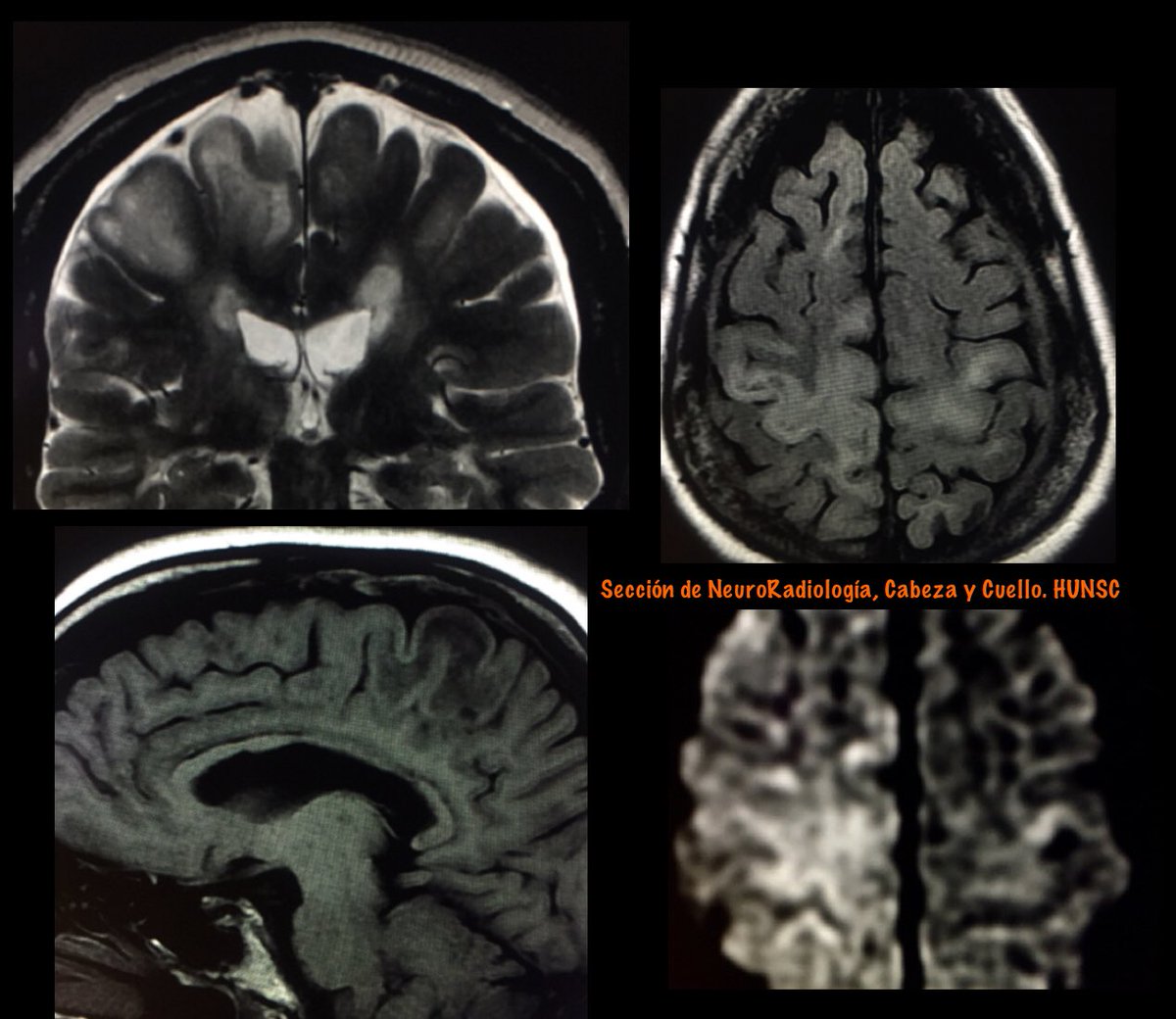
The appearance on DWI varies according to the disease stage.
In new active lesions, there is a rim of diffusion restriction at the advancing edge and a central core of facilitated diffusion
The rim is usually incomplete and signifies active infection
The appearance on DWI varies according to the disease stage.
In new active lesions, there is a rim of diffusion restriction at the advancing edge and a central core of facilitated diffusion
The rim is usually incomplete and signifies active infection

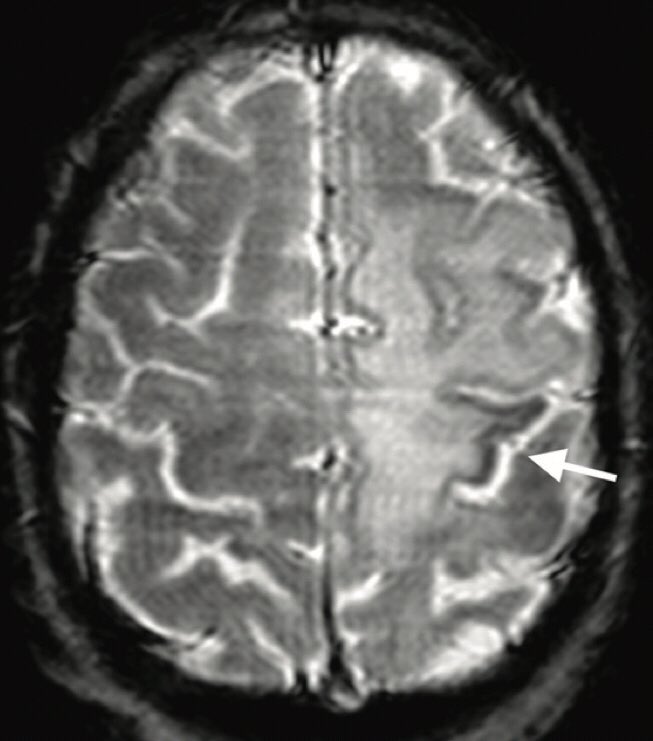
The Punctate Pattern (PP)
Refers to T2 weighted hyperintense or enhancing brain punctate lesions (milky way appearance)
The PP is a sensitive imaging feature of NTZ- PML and may be of use to differentiate PML lesions from MS plaques.

Refers to T2 weighted hyperintense or enhancing brain punctate lesions (milky way appearance)
The PP is a sensitive imaging feature of NTZ- PML and may be of use to differentiate PML lesions from MS plaques.


SWI Changes in PML
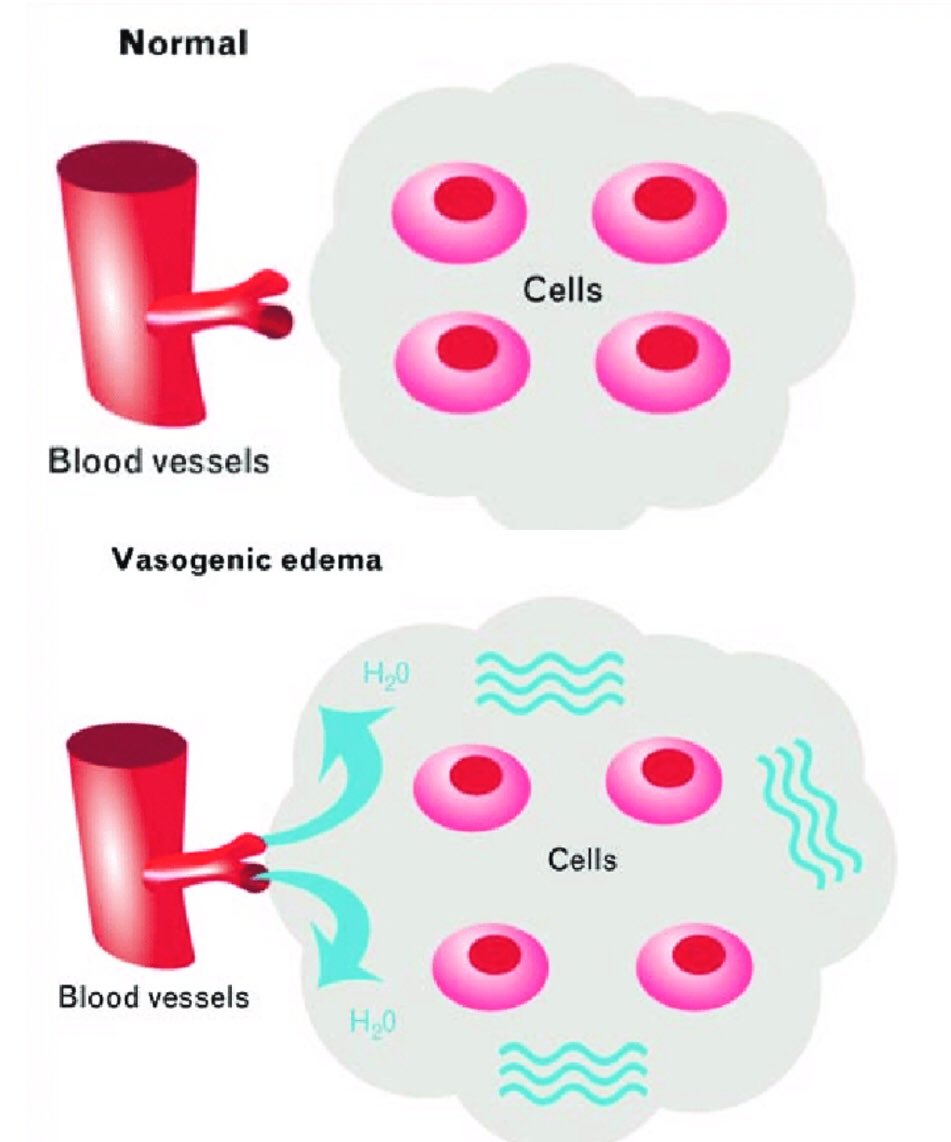
PML, related to NTZ or not, induces brain magnetic susceptibility changes within U-fibers or deep gray matter, visible on T2* or SWI and potentially explained by iron deposition
Such findings were observed at the presymptomatic stage

PML, related to NTZ or not, induces brain magnetic susceptibility changes within U-fibers or deep gray matter, visible on T2* or SWI and potentially explained by iron deposition
Such findings were observed at the presymptomatic stage
AJNR 2010
DOI 10.3174/ajnr.A2035
10.1594/ecr2015/B-0300
Neurology 2016;86;1516-1523
DOI 10.1212/WNL.0000000000002586
AJNR 2015
dx.doi.org/10.3174/ajnr.A…
Curr Opin Neurol 2014, 27:260–270
DOI:10.1097/WCO.0000000000000099
DOI 10.3174/ajnr.A2035
10.1594/ecr2015/B-0300
Neurology 2016;86;1516-1523
DOI 10.1212/WNL.0000000000002586
AJNR 2015
dx.doi.org/10.3174/ajnr.A…
Curr Opin Neurol 2014, 27:260–270
DOI:10.1097/WCO.0000000000000099
• • •
Missing some Tweet in this thread? You can try to
force a refresh