1/ Today marks my 18 month-aversary since beginning the #LCCholesterolChallenge cholesterolcode.com/lccholesterolc… and exactly a year ago adding #LDLBounty to meet the challenge. To date, I've only found studies showing the opposite -> High LDL+High HDL+Low TG = Low cardiovascular disease..
2/ The reason I say "best study" in the challenge instead of "any study" is that I thought it may well be possible there were tens if not hundreds of studies that might meet the definition. Again, I've only found the opposite, like this one: ncbi.nlm.nih.gov/pubmed/27166203
3/ The colored overlays are mine, to emphasize this "triad" of high LDL, high HDL, and low triglycerides... 
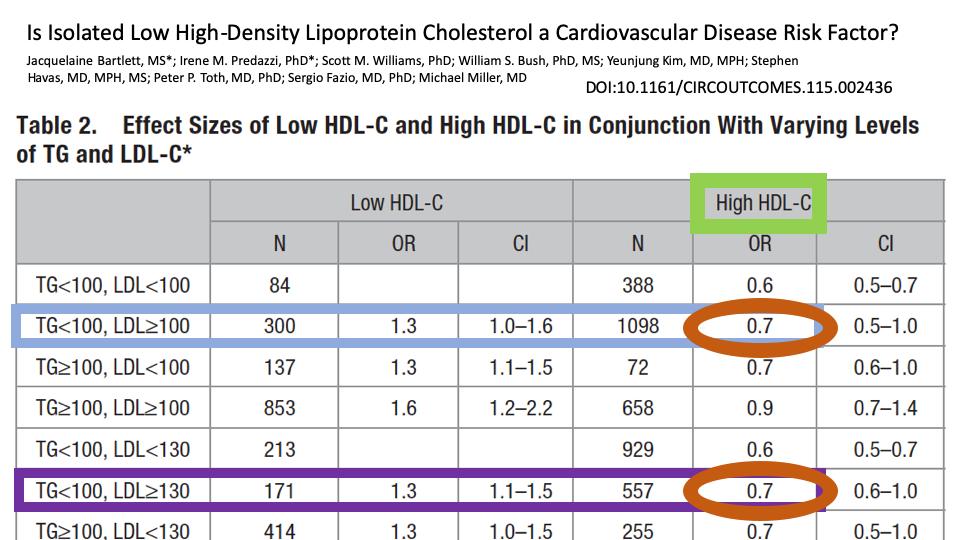
4/ And this one ncbi.nlm.nih.gov/pubmed/11176761 with the highly viral graph here...
5/ Where they first stratified between those with an LDL of < 170 and LDL ≥ 170, then substratified three groups of high HDL+low TG, low HDL+high TG, and one in between. 

6/ As it happens, the reverse of this triad already has a name in the literature, "Atherogenic Dyslipidemia", which is characterized by low HDL, high TG, and a preponderance of small dense LDL particles. It is has an extremely high association with cardiovascular disease...
7/ It's worth reminding everyone as to why I set up the challenge in the first place. I didn't pick these markers out of a hat, they are extremely relevant to the Lipid Energy Model we're working on at CC, which is central to my research and experiments. CholesterolCode.com/model
8/ I hypothesize high LDL, high HDL, and low TG generally suggests a healthy lipid metabolism. (Again, that's generally, not always) And if so, I suspect that's highly relevant to cardiovascular disease outcomes and especially all cause mortality.
9/ Getting a hold of NHANES was a game changer, as it helped to provide further evidence for this hypothesis, though with all the usual caveats that should be applied to observational data.
10/ Which brings me back to the #LCCholesterolChallenge. I'm now more skeptical than I've been before that it will be met. The bigger question is whether this will apply to those with *very* extraordinary levels of the triad, and by that I mean #LMHRs CholesterolCode.com/lmhr
11/ While I'm cautiously optimistic, I certainly emphasize that only real, clinical trial data will provide strong evidence. This is why I'm working very hard to make that happen as soon as possible.
• • •
Missing some Tweet in this thread? You can try to
force a refresh