Here’s an interesting paper published in JACC yesterday. The investigators studied 187 acute myocarditis patients with CMR (within a week) and repeated the CMR at 6 months.
onlinejacc.org/content/74/20/…
onlinejacc.org/content/74/20/…
They found that LGE was present in 96% at the initial presentation and 86% at 6 months. They conclude:
“In the acute setting, LGE does not mean definite fibrosis, and it may disappear at 6 months.”
“In the acute setting, LGE does not mean definite fibrosis, and it may disappear at 6 months.”
In the main text, they elaborate:
“Our data demonstrated that LGE in the acute phase of myocarditis is not necessarily synonymous with irreversible damage, because in 11% of our patients, LGE completely disappeared at follow-up.”
“Our data demonstrated that LGE in the acute phase of myocarditis is not necessarily synonymous with irreversible damage, because in 11% of our patients, LGE completely disappeared at follow-up.”
What do I think?
- What does LGE in acute myocarditis mean?
- It certainly does not mean fibrosis… fibrosis is another word for scar, and the human body takes time to heal and form a scar. In the acute setting, it is necrosis. This means dead myocardium with edema.
- What does LGE in acute myocarditis mean?
- It certainly does not mean fibrosis… fibrosis is another word for scar, and the human body takes time to heal and form a scar. In the acute setting, it is necrosis. This means dead myocardium with edema.
- Is LGE in the acute myocarditis synonymous with irreversible damage?
- Absolutely. See above. Until we figure out a way to regenerate human myocardium, the death of myocardium is irreversible damage.
- Absolutely. See above. Until we figure out a way to regenerate human myocardium, the death of myocardium is irreversible damage.
- But wait, if LGE represents irreversible injury, then why did it disappear in 11% of the cases in this paper?
- Because LGE detects focally dead myocardium and the technique has a minimum threshold for detection. Generally, it’s around 1 cm3 of myocardium.
- Because LGE detects focally dead myocardium and the technique has a minimum threshold for detection. Generally, it’s around 1 cm3 of myocardium.
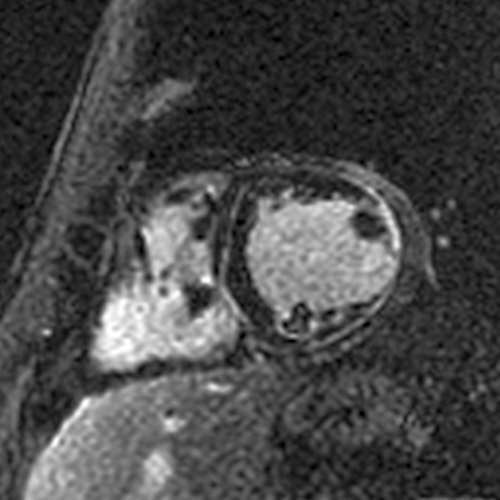
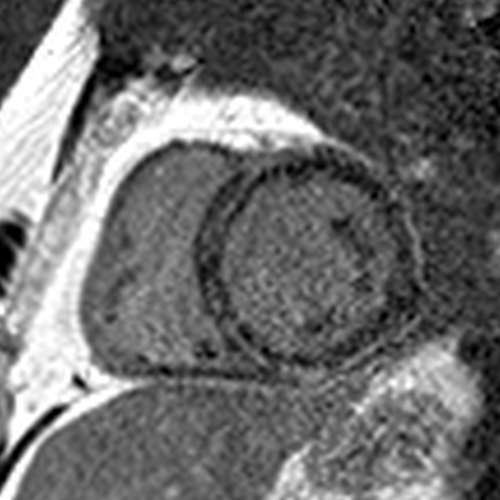
In acute myocarditis, the volume of the dead myocardium is larger because of edema (think of a swollen bruise or cut on your knee). 

In healed myocarditis, the volume of the same dead myocardium is smaller due to scar formation, shrinkage, and compaction (think of healed scar tissue on your knee). 

And in some instances, the volume of the healed dead myocardium may be below the threshold of detection by LGE.
Think of the injury in terms of the fraction of the cardiac cells that are dead. It’s the same in both the acute and healed stages, even if “LGE disappears”.
Think of the injury in terms of the fraction of the cardiac cells that are dead. It’s the same in both the acute and healed stages, even if “LGE disappears”.

So LGE in the acute stage indeed represents dead myocardium even if it disappears in some. The "disappearance" is explained by changes in the dead myocardium over time and thresholds of detection of dead myocardium by LGE.
The investigators also write: “For this reason, myocarditis differs from myocardial infarction, where LGE is always associated with irreversible myocardial damage, the extent of which usually decreases at follow-up due to scar shrinkage, although it never disappears completely.”
- So why does LGE disappear in myocarditis but not MI?
- Actually, LGE can "disappear" in MIs as well, and for the same reasons. It happens less often than in myocarditis because the dead myocardium in MIs is often larger in size than in myocarditis and MIs are serially imaged less often than myocarditis (so we don’t see it as much).
• • •
Missing some Tweet in this thread? You can try to
force a refresh