Moderated by Drs. @tomcnguyen @BrianMitzman Chikwe
Featuring Drs. @igeorge1975 @vinodthourani @TomMihaljevicMD et al
Zoom: zoom.us/j/559438750
Hashtag: #CTSNetLive
Live tweet thread to follow below

Lets learn together rather than apart #CTSNetLive #TSSMN
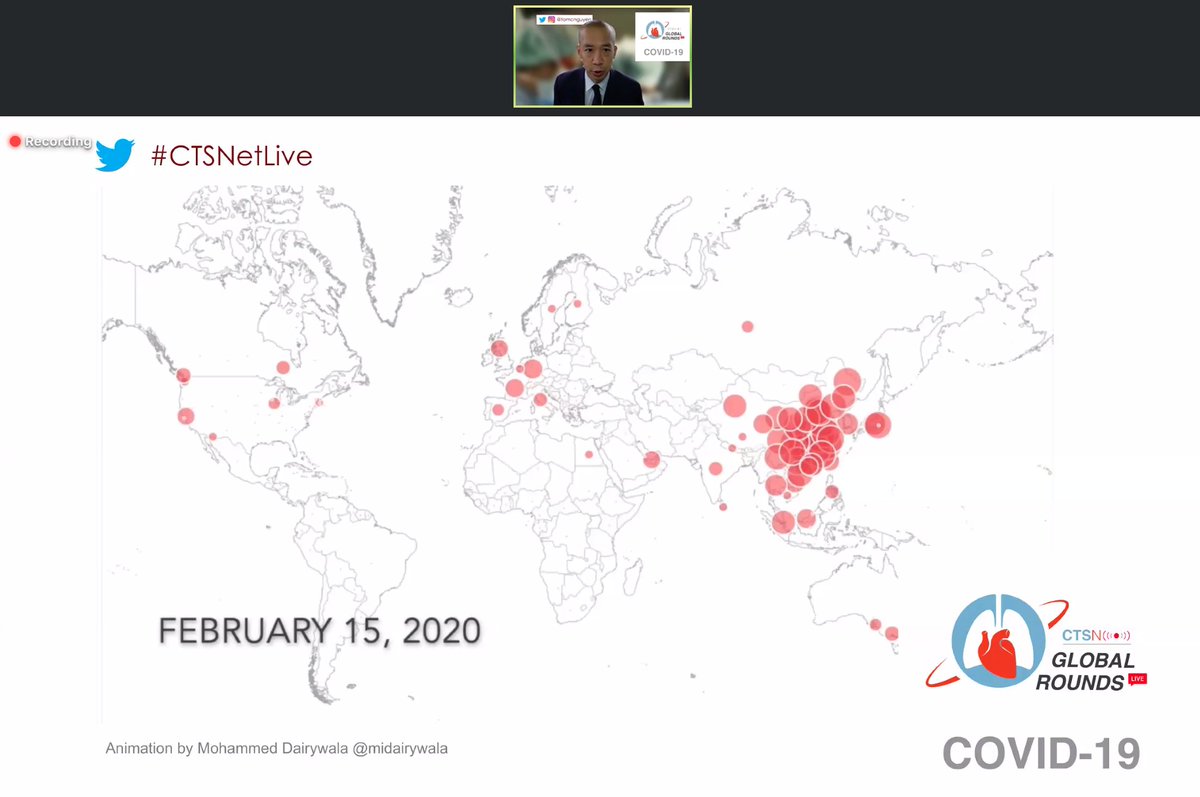
What we know:
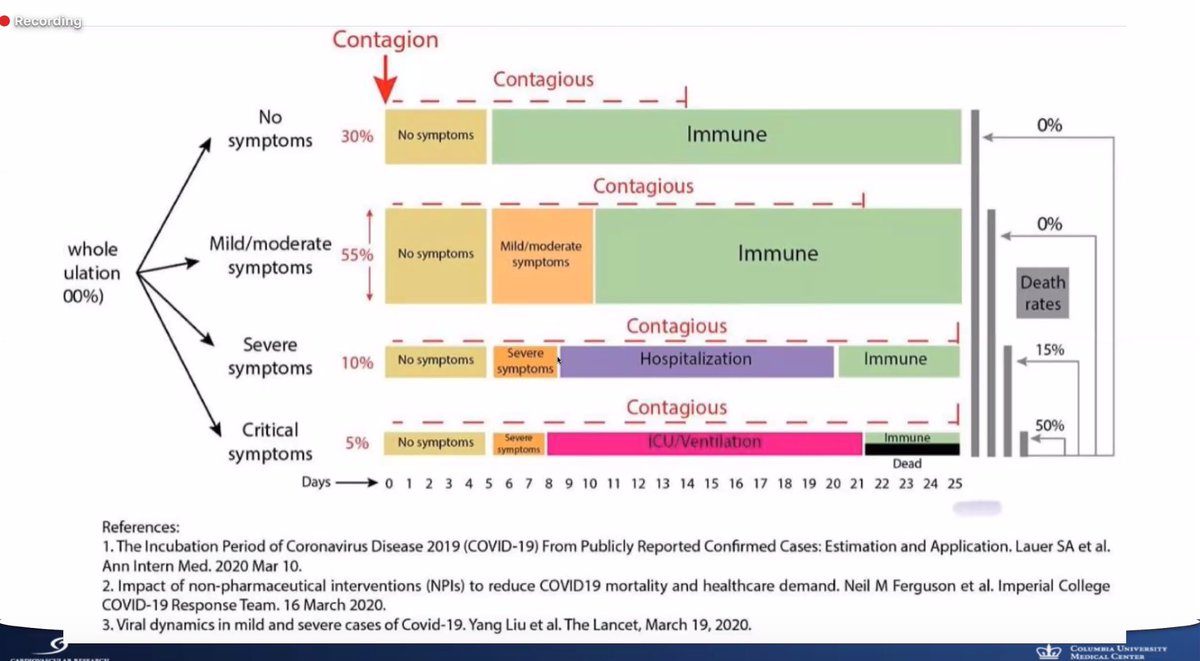
- #COVID19 has a capacity to kill depending on healthcare capacity and ability to take care of the patients
- need to identify cases quickly and suppress
- this is an unseen enemy that is capable of causing enormous problems
Key actions that need to be taken:
- #GetMePPE for your healthcare workers
- early detection, isolation and testing vital given unchecked rapid spread
Q: Do we need to isolate ourselves from family as healthcare workers? Depends on context, consequences. If high risk exposures or high risk individuals at home -> yes consider isolation at your own risk
@WHO actively seeking unique ways to overcome #GetmePPE shortages, ventilator and resource shortages - so calling all physicians to send @WHO links, resources and ideas.
Q: What will happen with low-and-middle income countries and how to cope with #COVID19? - hope differences in temperature, age of population etc will reduce impact. But ultimately, just don't know. Potential severe consequences
For isolation - there is potential for people's liberty rights restricted, travel bans and restrictions.
Need to focus on isolation, testing, mitigation, suppression and protection of our frontline workers.
COVID-19 - We're all going to get it, if we don't have it already"
#COVID19 is serious and attention needs to be paid to this disease.
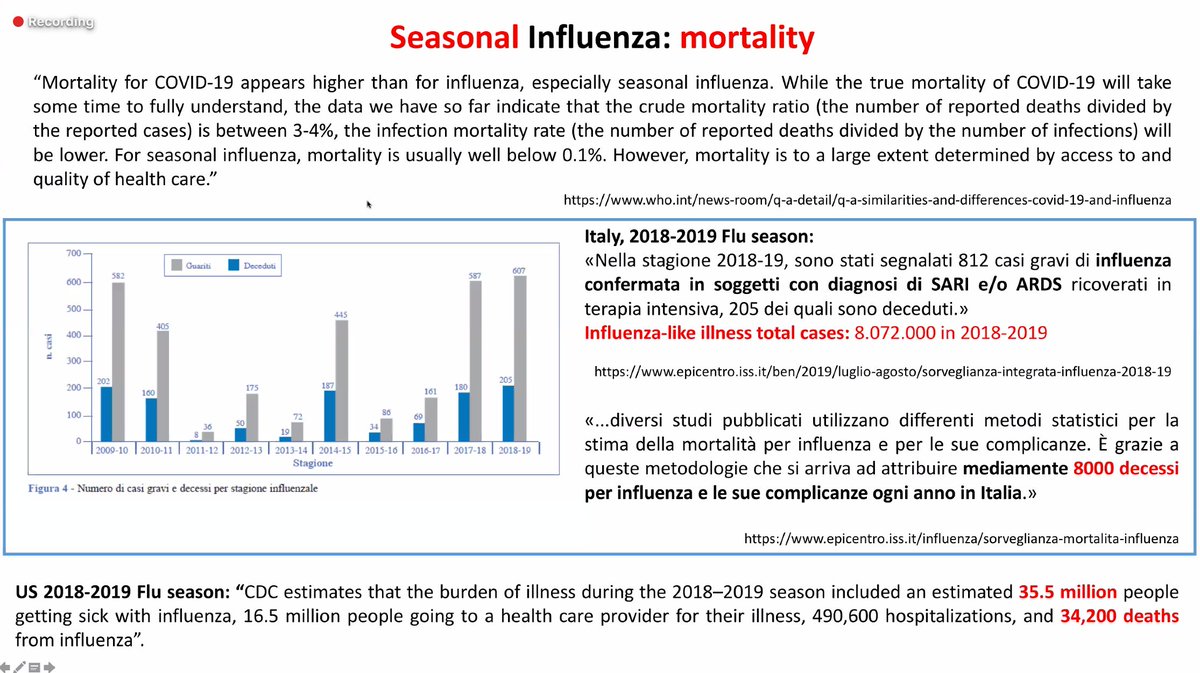
#COVID19 mortality is higher than influenza and infectivity is high.
Recommendations for the rest of the world, drawing from the Italy experience:
- Testing and protecting your healthcare workers are key
Q: If a healthcare worker has an exposure to #COVID19 patient without PPE, what should they do at home? - they should wear PPE
Q: Should all healthcare workers be screened given risk of asymptomatic exposure? -only if symptoms
Q: What is the sensitivity and specificity of current test? 90% sensitive, high specificity. If high suspicion - consider testing twice or treating the patient as #COVID19 positive despite a negative test if symptoamtic
I'm a cardiac surgeon and have COVID-19: Now what?"
@igeorge1975 - thank you so much for sharing your personal experience!
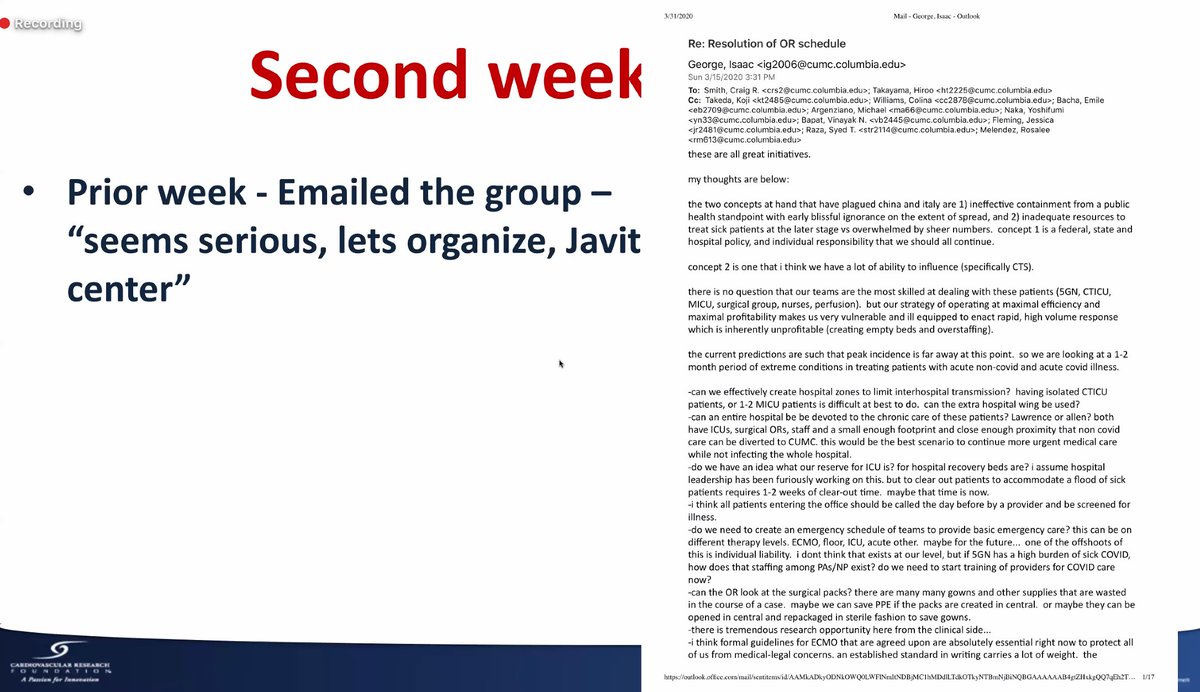
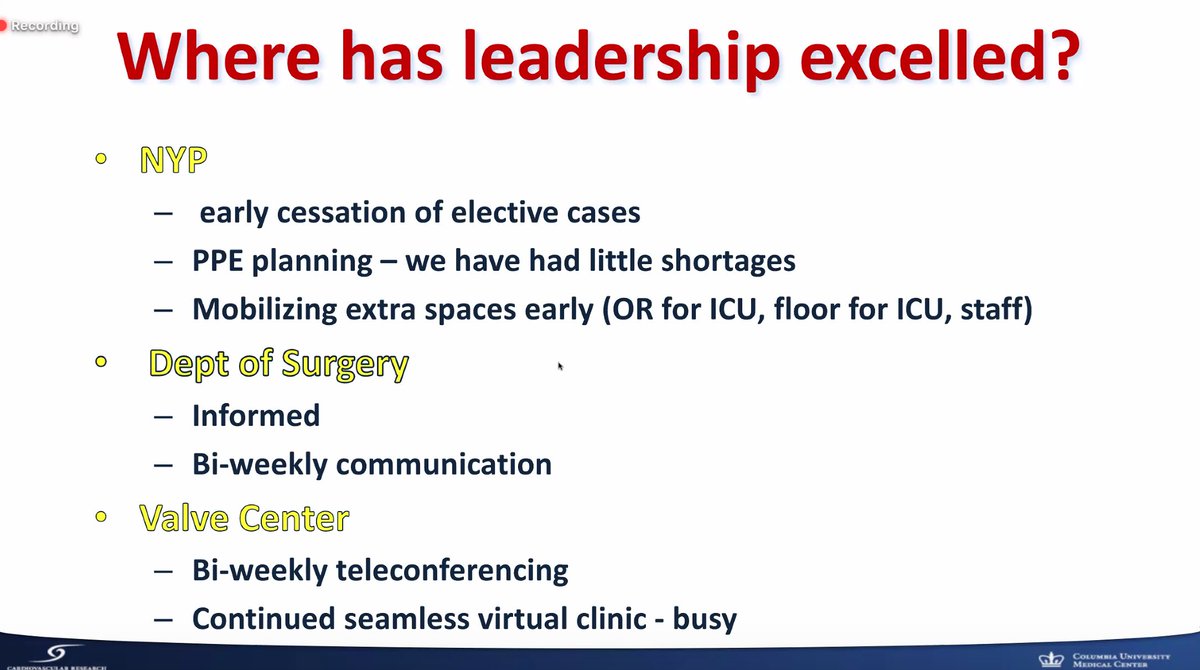
Their hospital-level approach to preparing for #COVID19
Timeline for symptoms with #COVID19 - key takeaway, very constitutional symptoms. Self-isolated from family when symptomatic. Wore PPE at home to protect family.
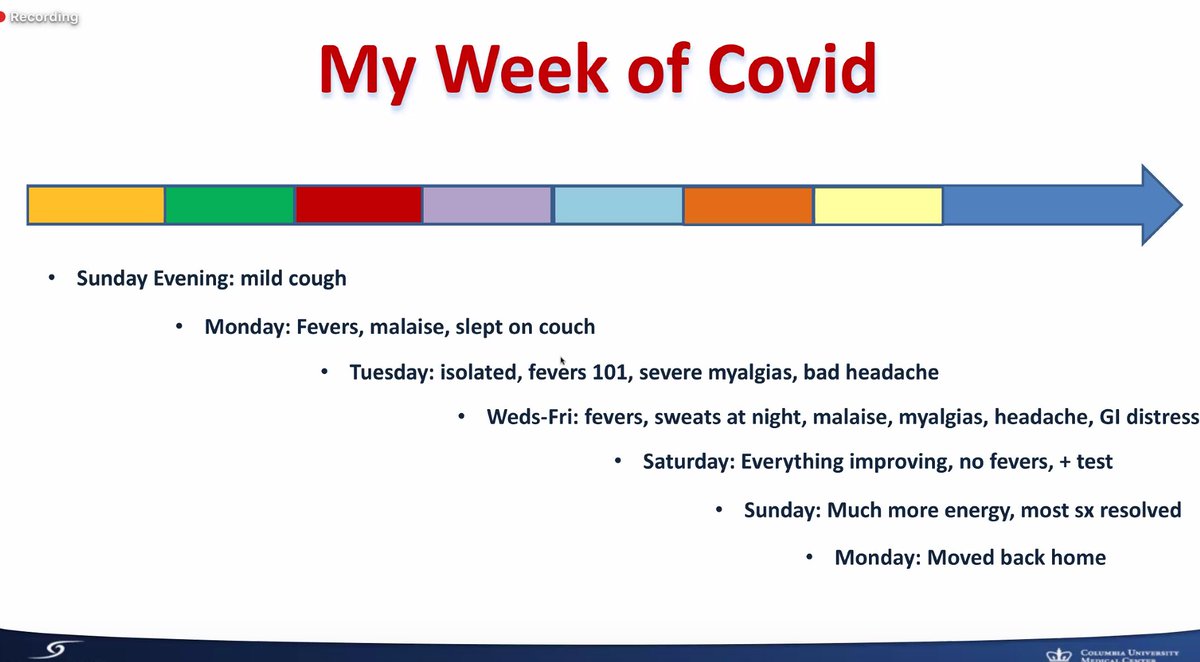
When do we go back to work? @CDCgov recommends 7 days since onset of symptoms or when afebrile for 72 hours (whichever is later).
Key takeaways:
- your risk of #COVID19 transmission can be from the last people you expect (those who are asymptomatic)
Key takeaways:
- stop elective cases to conserve PPE, resources and protect healthcare workers
- excellent communication
- utilize telecommunication technologies
What can be done better?
- mask protocol escalation (no mask -> surgical mask -> N95)
- ambiguous recommendations
- what isolation rooms should be
- testing for healthcare workers
Re-prioritize what is important in your life
We are all in this together and we will get through this
#BetterTogether
Q: Have you been re-tested to be negative prior to returning to work? I have not been re-tested. Serum testing needs to be 14 days out of the infection which would be the next step. (second confirmatory testing)
Q: Do you feel empowered with potential immunity against #COVID19? - We do not currently know whether there is immunity and only time will tell.
"Hello world, what could we have done differently?"
Symptoms included high fever and coughing. Stayed home. Need at least 2 negative swabs prior to returning to work at his institution
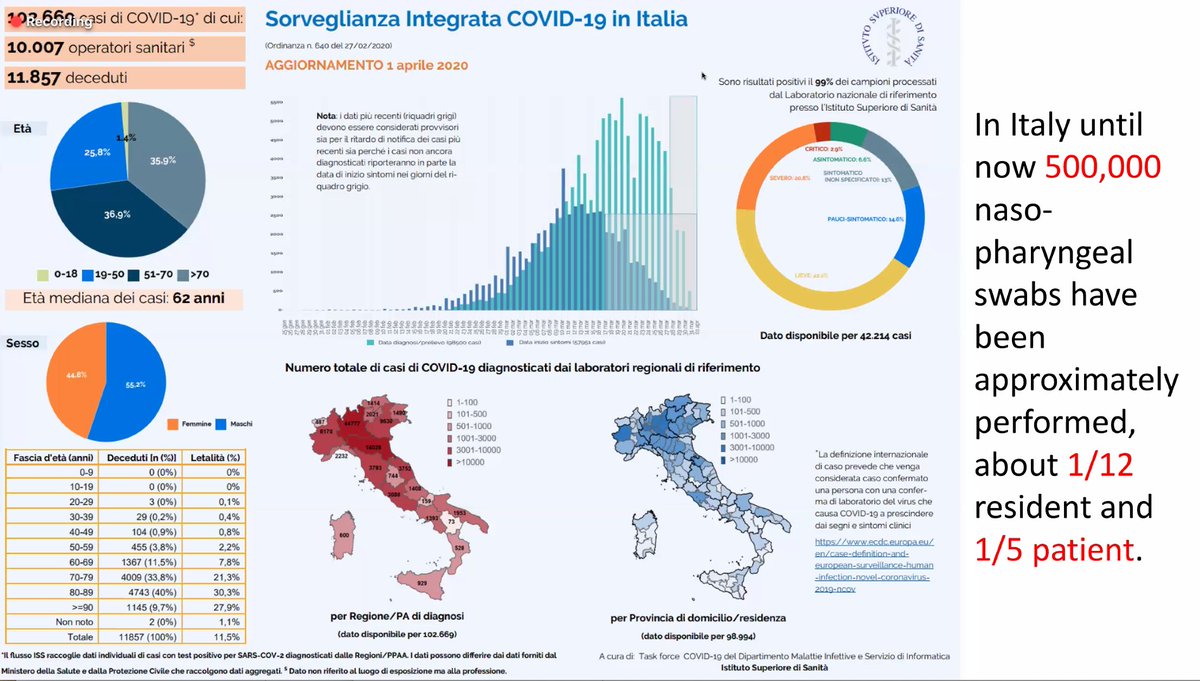
Italy has truly been on the forefront of the pandemic.
What we learned:
- testing key to combat #COVID19 -> quarantine the infected
- #GetMePPE vital to protect healthcare workers -> so far 80 doctors have died
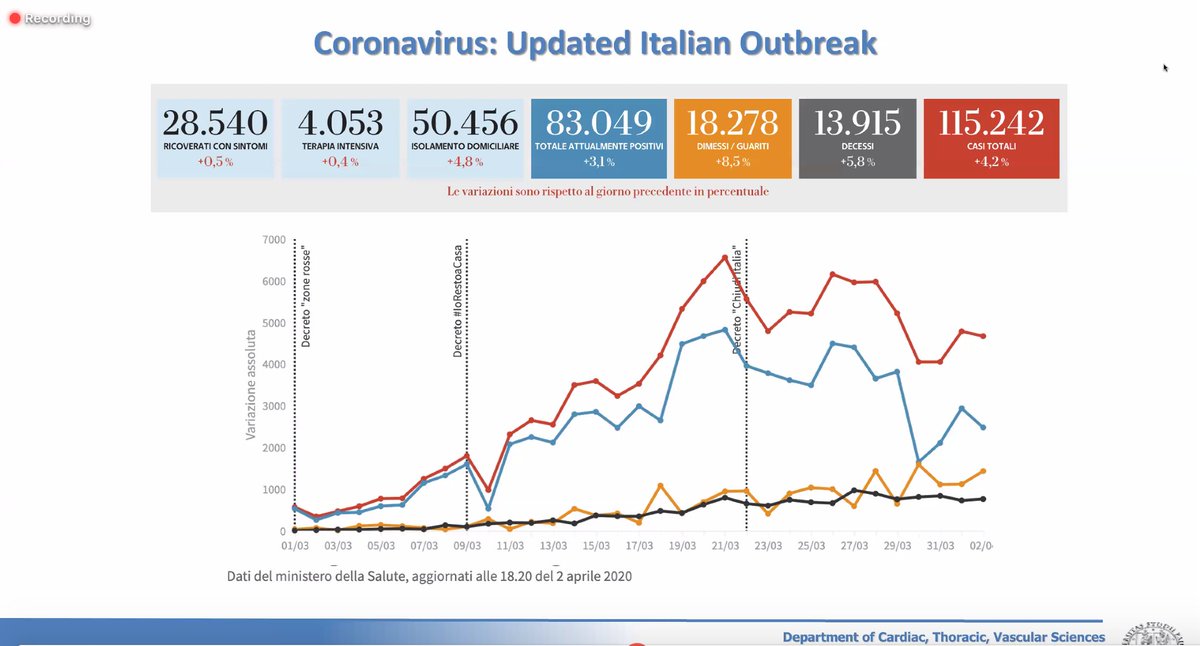
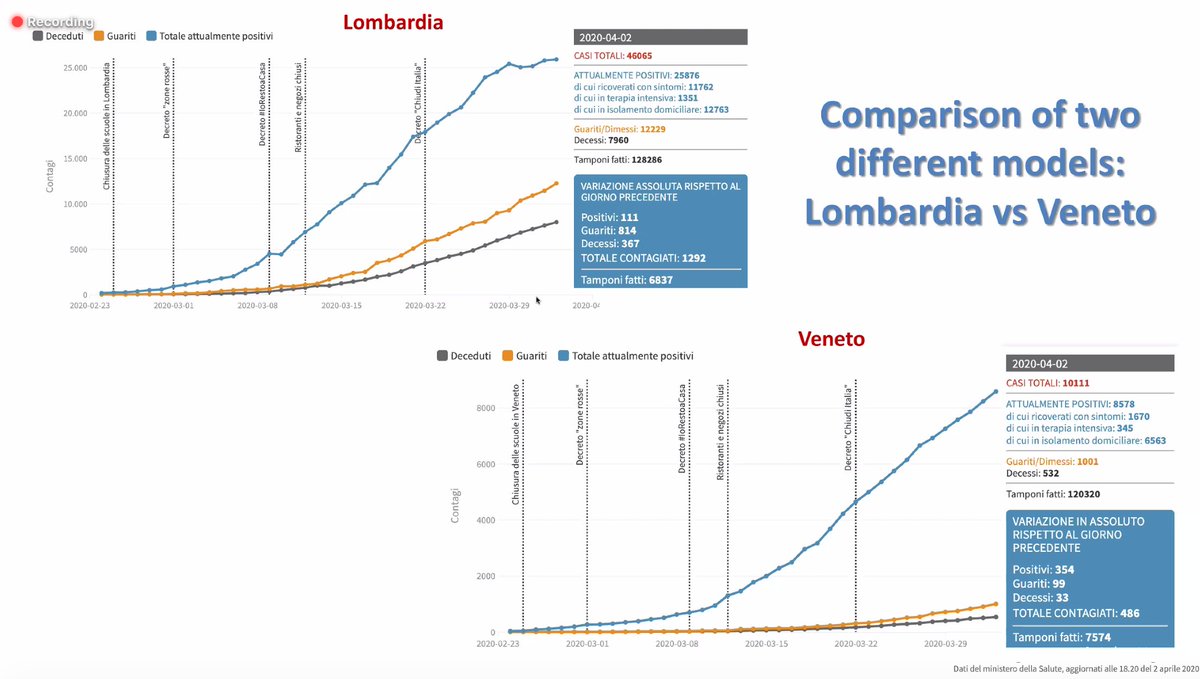
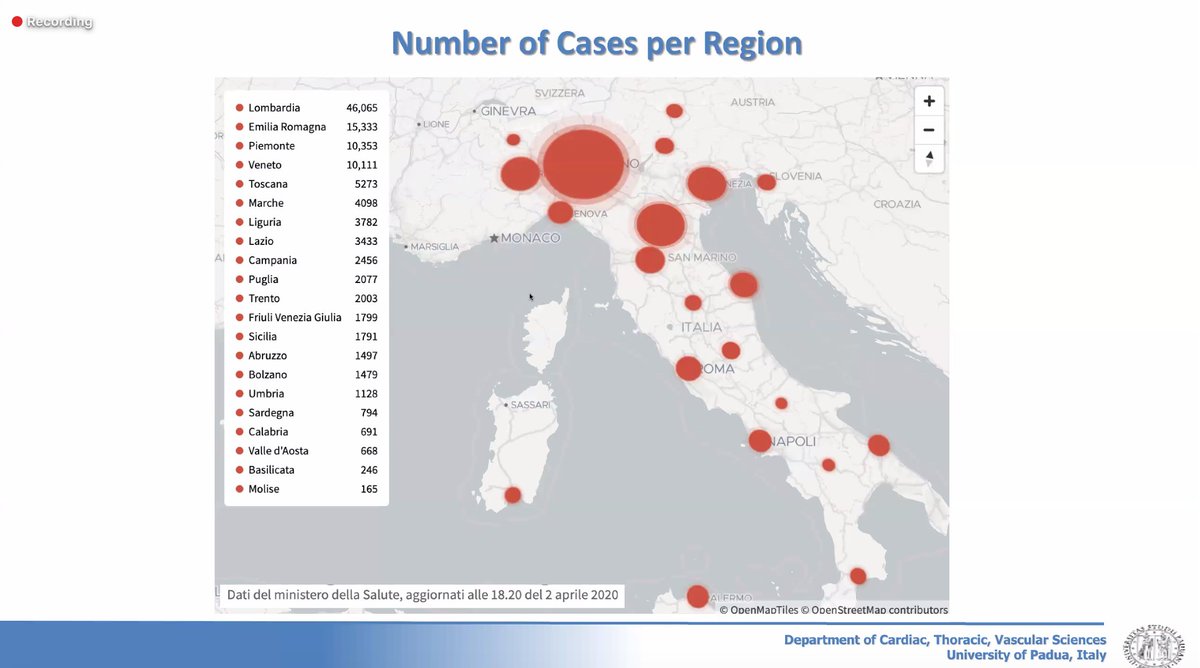
Lessons from the Italy experience:
- have COVID dedicated hospital
- close follow-up of patients as outpatients to keep them out of hospital
- isolate dead patients serum antibodies for testing and determine disease prevalence
Q: Why did Italy become the epicenter for #COVID19? Did not isolate and test those with exposures. This likely led to lots of community transmission with the lack of social distancing and quarantine.
Q: What is the morale now in Italy? Social distancing very seriously enforced in Italy with most non-essential services closed.
Q: What advice do you have for the rest of the world? Social distancing and testing key.
For heart transplants, less donors due to:
- Social distancing (less accidents)
- #COVID19 patients taking up ICU beds and hospital resources
- need to test donors and recipients to be #COVID19 negative prior to transplantation
"When (if) the COVID dust settles, what will be the long-term impact to economies and health care institutions?"
- tripled hospital and ICU capacity in anticipation for the wave
- social distancing in place (one of the first states in the US)
What to expect after #COVID19 pandemic:
- increased utilization of telemedicine
- increased ambulatory care
- hospital care reserved only for those who truly need it
- care for healthcare workers
The following would be emphasised post #COVID19
- Increased appreciation for healthcare workers, social life, leadership, integrated healthcare systems and what truly matters
- shared resources / care
What to see after #COVID19
- More integrated healthcare systems
- Centralization of care and resources
- Decline in small isolated healthcare systems
- We are #bettertogether
- Larger role for central payer
What to see after #COVID19
- Lifelong partnership between patients and providers
- Meet needs of patients with digital technology
- Emphasis of data-driven care and preparation for disasters
How to live with the pandemic?
- Help those in need
- Expect serious economic downturn
- Beware of deferred care
- Need to consider sustainability
Takeaways:
- Scale up digital technology
- Seek partnerships
- Predictive modelling+artificial intelligence to tailor approach to pandemic
- Know your data
- Work with worse case scenario -> Prepare for this
Takeaways:
- Educate+reassign healthcare providers where they are needed
- Support and protect your people #GetMePPE
- Communication is key to empower your team and the public
- Complete transparency
- Listen
Q: What will be the new norm with PPE? With greater availability of testing, we can taillor our response. But at this time, need PPE. Some will be here to stay as the new norm.
Q: What has been the role of advanced care providers in #COVID19? Ensure people are educated and well-supported in their new / altered roles with oversight by a multidisciplinary team.
Q: What is the financial sustainability of healthcare systems with #COVID19? We will always have losses because we have suspended our non-essential clinical activity along with delayed reimbursement with fixed HCW costs
"Stay calm and carry on" ... this pandemic will accelerate into some sort of good in medicine.
We are at a place where we do not have all the answers for, unlike #CTSurgery
- Critical to evaluate therapies in a scientific evidence-based manner
- Remain grounded -> patient safety first
- Scientifically and ethically sound
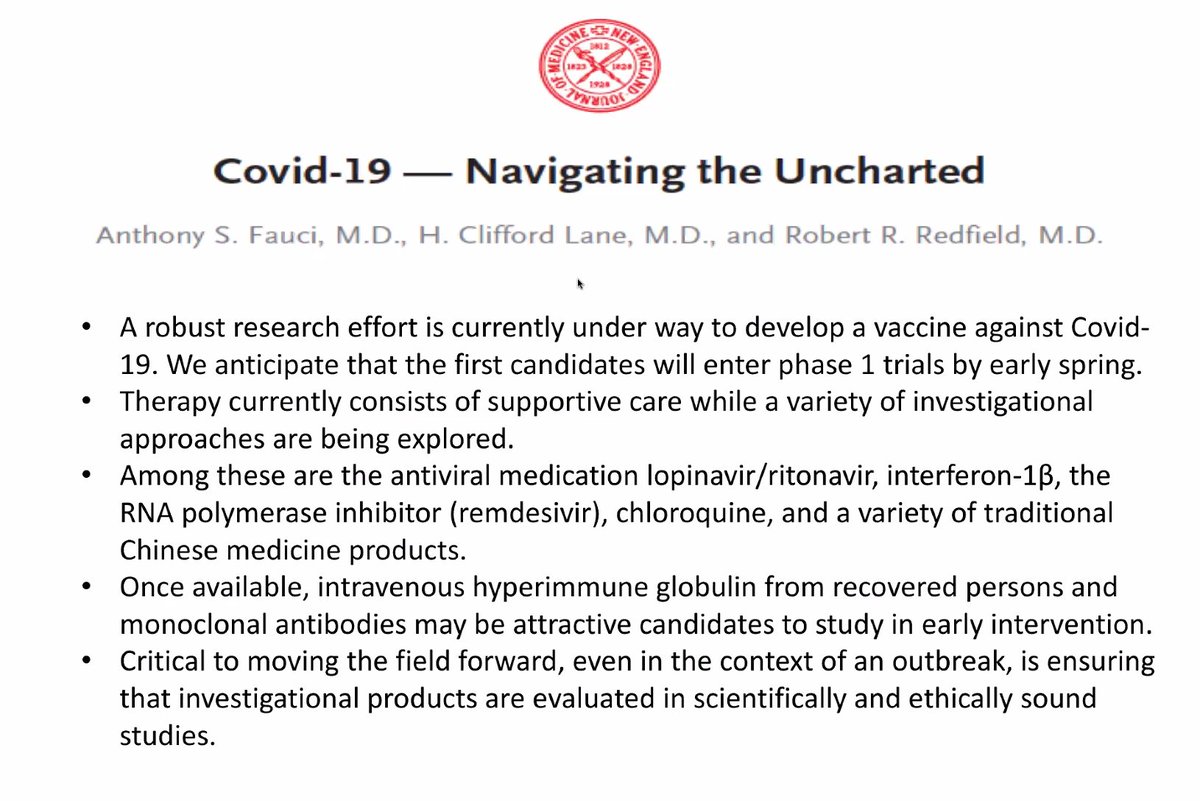
Monoclonal antibodies coming down the pipeline as a potential therapy for #COVID19
Antivirals coming down the pipeline as a potential therapy for #COVID19
Cell and RNA-based therapies coming down the pipeline as a potential therapy for #COVID19
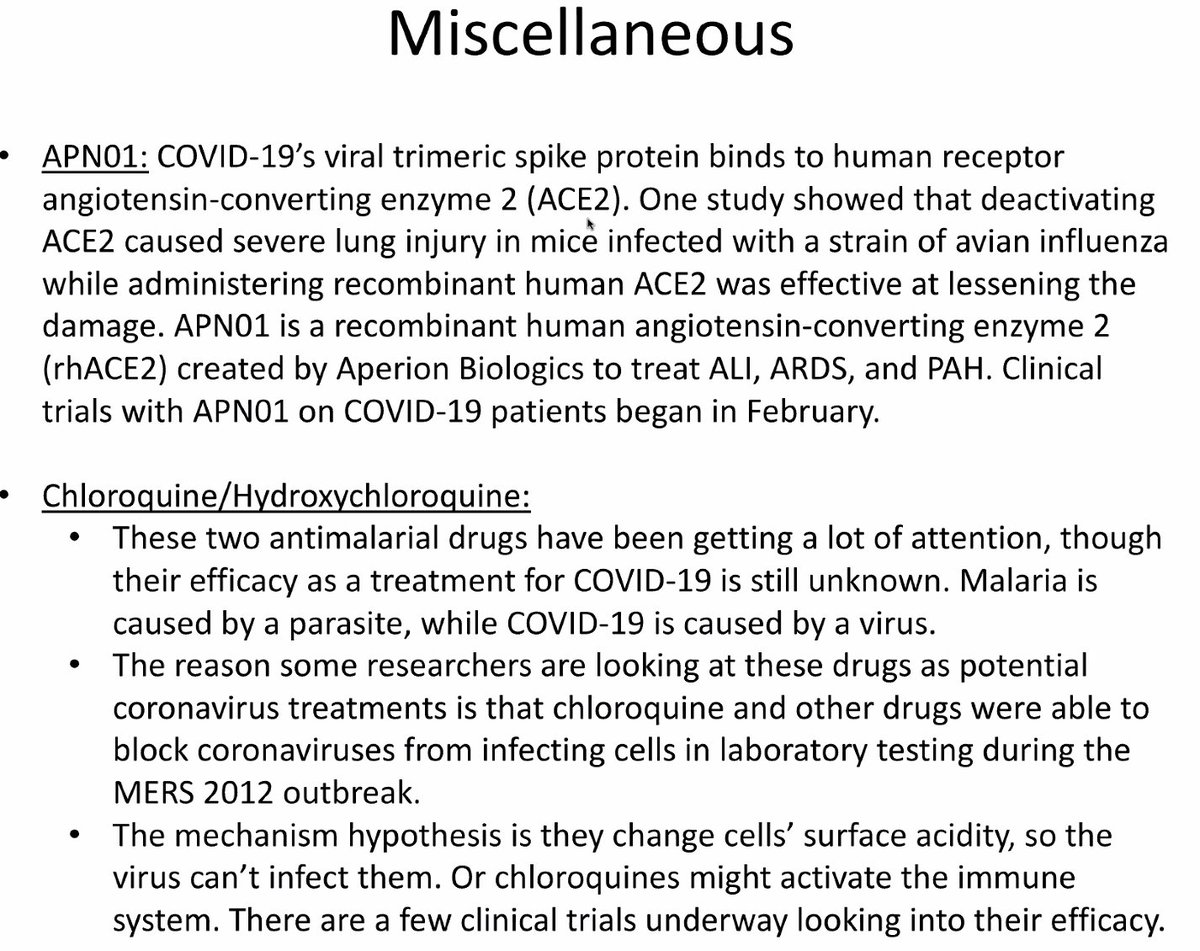
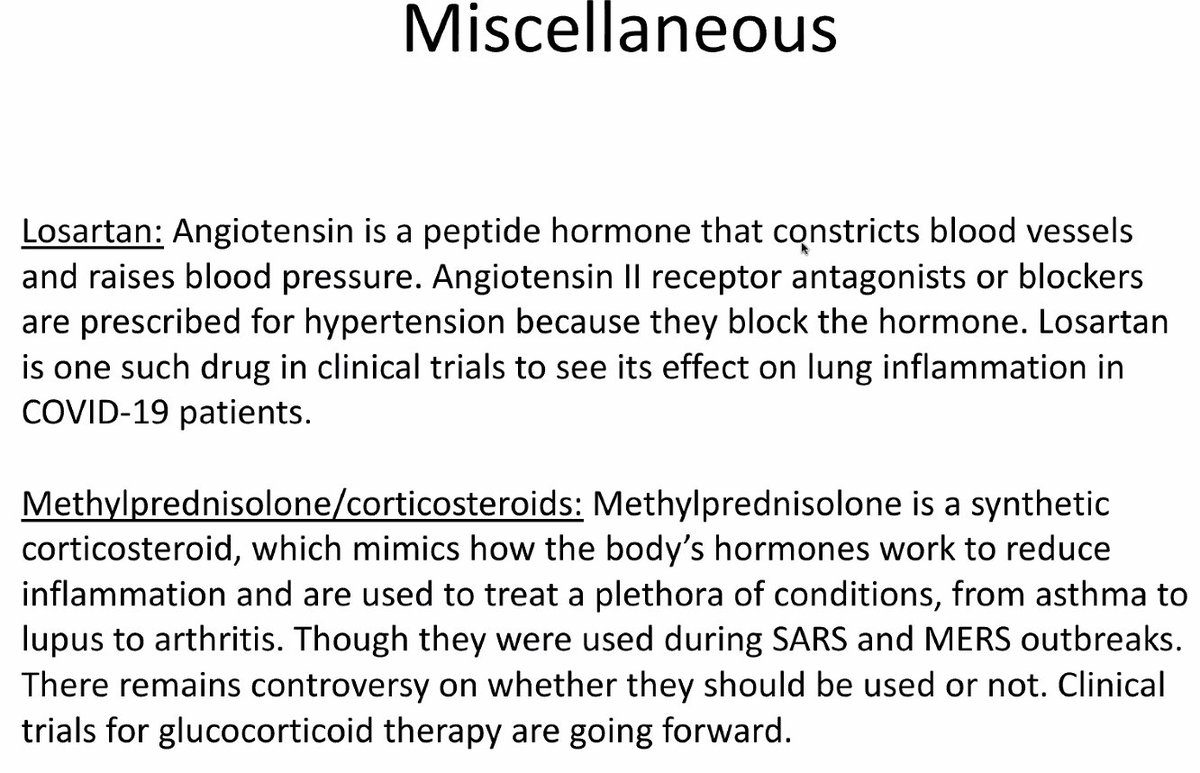
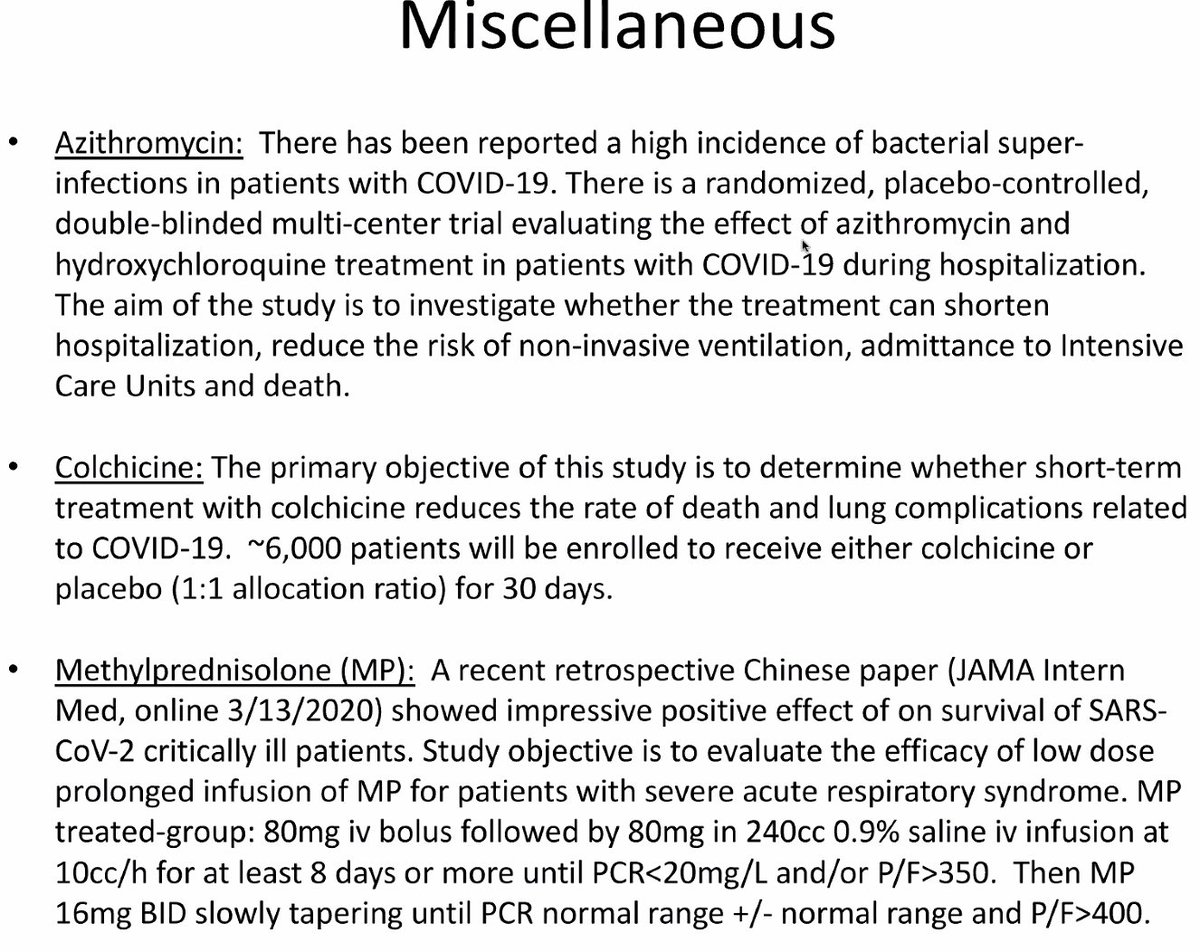
Miscellaneous therapies coming down the pipeline as a potential therapy for #COVID19
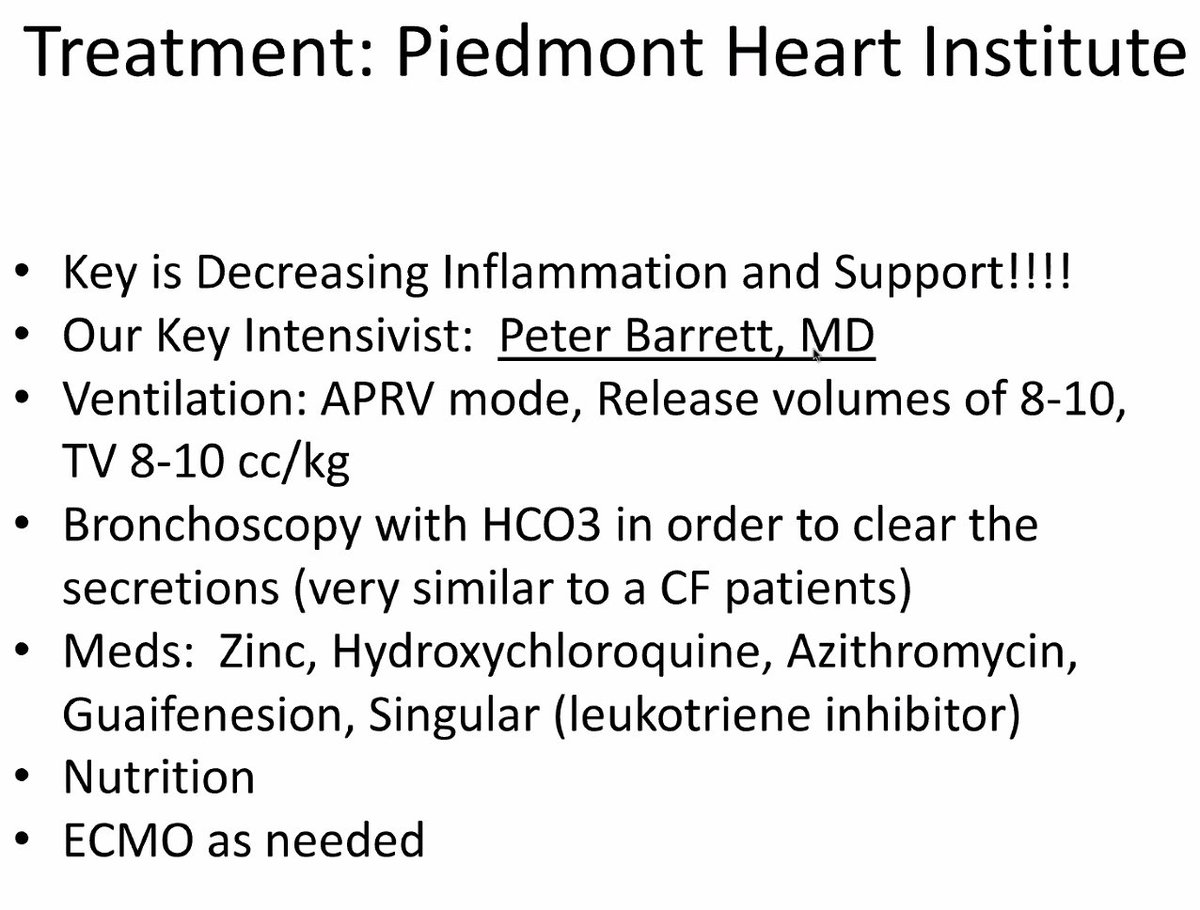
What they are doing at Piedmont Heart Institute
- Ventilation
- Bronchoscopy
- Zinc, hydroxychloroquine, azithromycine, singular
- Nutrition
- ECMO
ECMO in
- severe reversible hypoxia / hypercarbia
- earlier than later in those without irreversible end-organ damage
- be thoughtful in utilizing this modality if ventilation is not working
"Ground Zero in New York: Our hospital before and during the surge. What have we learned?"
The situation in New York:
- hospital tents being set up in Central Park
- US ship to relieve hospitals - but strict criteria for pt admission
At the start of the New York pandemic:
- COVID isolation rooms -> flooding in hallways -> reallocating other areas of hospital to become COVID designated areas -> ambulances flooding the roads
- Run out of ICUs
Situation now in New York:
- Nearly all hospitals on diversion
- Try to keep ER prioritized for people who need them
- People coding everywhere in stretchers - going apneic due to hypoxia
- Need to check on all pts on O2
- Pts (young and old) deteriorate quickly even though they may look fine initially
- Feel there is a failure in the healthcare system
- Need to protect healthcare workers
- Need a coordinated response to help prepare for surge

- Lack of #GetMePPE a huge issue, not available or being rationed
- Healthcare workers getting exposed to #COVID19 and getting sick or dying
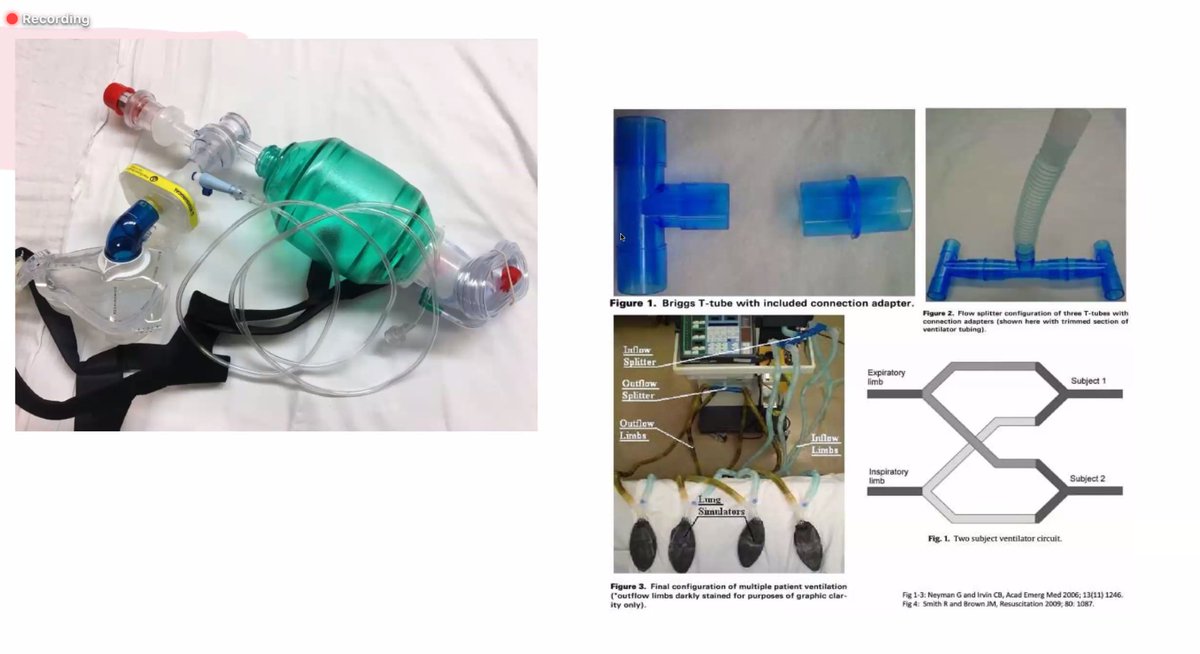
Makeshift tools for intubation:
- CPAP mask attached to ambu bag to create tight seal and able to pre-oxygenate patients prior to intubation
- Video laryngoscopy
- Kink the tube to decrease spray
- Ventilator splitting
Closing thoughts -
- Take care of each other
- Look after yourself
- We will get through this together
Q: What PPE are you using in these environments? N95, surgical mask and mask with shield and using this for several shifts.
Q: Mgmt for pts with regular issues? Ex. STEMI -> TPA rather than cath lab etc.
Take home message
- secure your supply chain
- prepare your resources
- expand your hospitals capacity
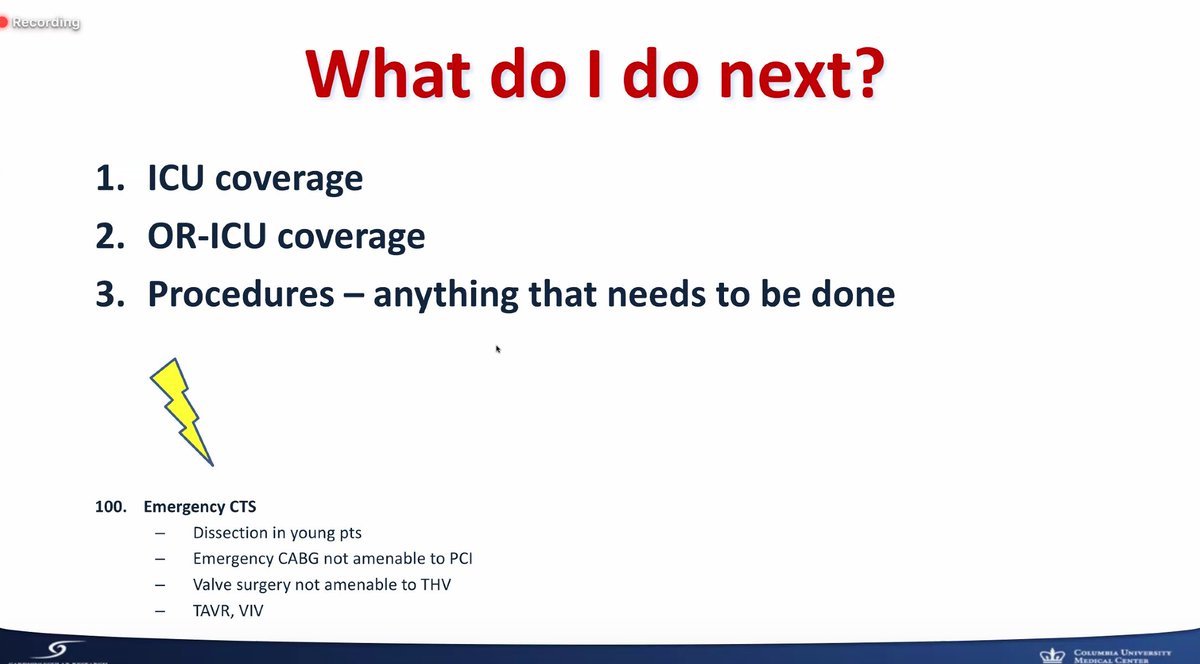
- ensure you have 24/7 coverage for non-COVID emergencies
- outsource patient care if possible (ex. telemedicine, ambulatory)
Stay well, be safe, look after each other. We will get through this. #tssmn
Make sure to also check out all the fantastic @ctsnetorg resources ctsnet.org/article/covid-…














